Chinese Journal of Tissue Engineering Research ›› 2014, Vol. 18 ›› Issue (44): 7133-7137.doi: 10.3969/j.issn.2095-4344.2014.44.015
Previous Articles Next Articles
Effect of percutaneous vertebroplasty and percutaneous kyphoplasty on adjacent intervertebral disc degeneration and mechanism
Tian Li1, Meng Chun-yang2, Xu Xiao-meng1
- 1First People’s Hospital of Jining, Jining 272000, Shandong Province, China; 2Affiliated Hospital of Jining Medical University, Jining 272000, Shandong Province, China
-
Online:2014-10-22Published:2014-10-22 -
Contact:Meng Chun-yang, Master, Master’s supervisor, Affiliated Hospital of Jining Medical University, Jining 272000, Shandong Province, China -
About author:Tian Li, Master, First People’s Hospital of Jining, Jining 272000, Shandong Province, China -
Supported by:Medical Science Project of Jining Municipal Science and Technology Bureau, No. 201085
CLC Number:
Cite this article
Tian Li, Meng Chun-yang, Xu Xiao-meng. Effect of percutaneous vertebroplasty and percutaneous kyphoplasty on adjacent intervertebral disc degeneration and mechanism[J]. Chinese Journal of Tissue Engineering Research, 2014, 18(44): 7133-7137.
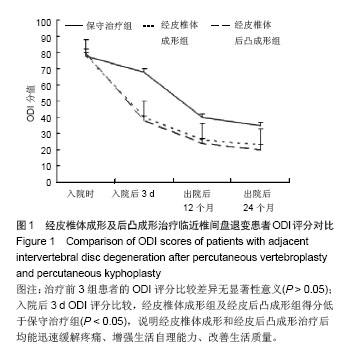
share this article
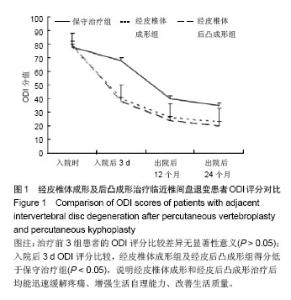
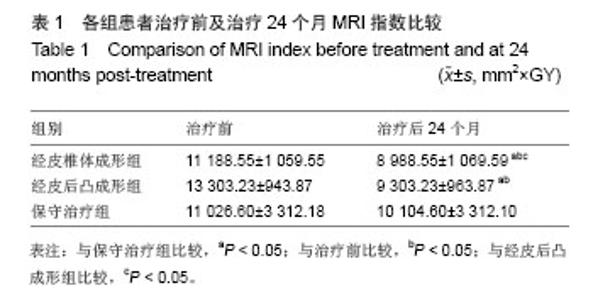
2.1 参与者数量分析 实验过程中能坚持随访的患者共85例,保守治疗组患者腰背部疼痛减轻较缓慢,住院时间一般需3周,在佩戴支具后可出院。经皮椎体成形组及经皮后凸成形组患者腰背部疼痛缓解迅速,平均住院日3.2 d,一般治疗后第2天出院。 2.2 各组不同时间点ODI评分比较 治疗前3组患者的ODI评分比较差异无显著性意义(P > 0.05);入院后3 d ODI评分比较,经皮椎体成形组及经皮后凸成形组得分低于保守治疗组,差异有显著性意义(P < 0.05),说明经皮椎体成形和经皮后凸成形治疗后均能迅速缓解疼痛、增强生活自理能力、改善生活质量。 出院后12,24个月的ODI评分比较,3组间比较差异均无显著性意义(P > 0.05),见图1。"
| [1]Campbell PG,Harrop JS. Incidence of fracture in adjacent levels in patients treated with balloon kyphoplasty: a review of the literature. Curr Rev Musculoskelet Med.2008;1(1): 61-64. [2]杨惠林.科学认识椎体成形术与椎体后凸成形术的临床价值[J].中国脊柱脊髓杂志,2010, 20(6):441-443. [3]Weiler C, Nerlich AG, Bachmeier BE, et al. Expression and distribution of tumor necrosis factor alpha in human lumbar intervertebral discs:a study in surgical specimen and autopsy controls. Spine (Phila Pa 1976). 2005;30(1):44-53. [4]Hiyama A, Mochida J, Sakai D. Stem cellapplications in intervertebral disc repair. Cell Mol Biol;2008, 54:24-32. [5]Le Maitre CL, Hoyland JA, Freemont AJ.Catabolic cytokine expression in degenerate and herniated human intervertebral discs: IL-1beta and TNFalpha expression profile.Arthritis Res Ther. 2007;9(4):R77. [6]Steiner G, Studnicka-Benke A, Witzmann G, et al.Soluble receptors for tumor necrosis factor and interleukin-2 in serum and synovial fluid of patients with rheumatoid arthritis, reactive arthritis and osteoarthritis.J Rheumatol. 1995;22(3): 406-412. [7]Séguin CA, Pilliar RM, Roughley PJ, et al. Tumor necrosis fac-tor-alpha modulates matrix production and catabolism in nucleuspulposus tissue. Spine ( Phila Pa 1976 ). 2005;30 (17): 1940-1948. [8]Holm S,Mackiewicz Z,Holm AK, et al. Pro-inflammatory, pleiotropic, and anti- inflammatory TNF-a, IL-6,and IL-10 in experimental porcine intervertebral disk degeneration. Vet Pathol.2009;6: 1292-1300. [9]Wu CL, Lin LY, Yang JS, et al. Attenuation of lipopolysaccharide-induced acute lung injury by treatment with IL-10. Respirology.2009; 4: 511-521. [10]Takahashi H. A meckenism for sciatic pain causrd by lumbar disk herniation involvement of inflammation cytokins with sciatic pain. Nippon Seikeigeka Gakkai Zasshi. 1995; 69(1): 17- 29. [11]Sobajima S, Kompel JF, Kim JS, et al. A slowly progressive and reproducible animal model of intervertebral disc degeneration characterized by MRI, X-ray, and histology. Spine (Phila Pa 1976). 2005;30 (1): 15-24. [12]Galibert P, Deramond H, Rosat P, et al. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vcrtebroplasty. Ncurochirurgie.1987;33(2):166-168. [13]Pitton MB, Herber S, Bletz C, et al. CT-guided vertebroplasty in osteoproticvertebral fractures; incidence of secondary fractures and inpact of intradisal cement leakages during follow up. Eur Radiol. 2008;18:43-50. [14]Qian J, Yang HL, Jing JH, et al. The Early Stage Adjacent Disc Degeneration afterPercutaneous Vertebroplasty and Kyphoplasty in The Trcatment of Osteoporotic VCFs. Plos ONE.2012;7(10): c46323. [15]Fan SW, Zhou ZJ, Hu ZJ, et al. Quantitative MRI analysis of the surface area, signal intensity and MRI index of the central bright area for the evaluation of early adjacent disc degeneration after lumbar fusion. Eur Spine.2012; 21(9): 1709-1715. [16]Berlemann U, Ferguson SJ, Nohe LP, et al. Adjacent vertebral failure after vertebroplasty:a biomechanical investigation . J Bone Joint Surg Br.2002; 84(5):748-752. [17]Polikeit A,Nolte LP,Ferguson SJ. The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit:finite-element analysis.Spine. 2003; 28(10):991-996. [18]李志远,申勇,王林峰,等,椎体成形术治疗老年骨质疏松椎体压缩骨折对邻近节段生物力学的影响[J].中国脊柱脊髓杂志, 2009, 19(5): 388-391. [19]Ogata K, Whiteside LA.An experimental study using hydrogen washout technique.Spine.1981; 6:211-216. [20]Sato M, Asazuma T, Ishihara M, et al.An experimental study of the regeneration of the intervertebral disc with an allograft of cultured annulus fibrosus cells using a tissue-engineering method.Spine (Phila Pa 1976). 2003 Mar 15; 28(6):548-553. [21]Nerlich AG, Schleicher ED, Boos N. Immunohistologic markers for age-related changes of human lumbar intervertebral discs. Spine.1997;22: 2781-2795. [22]Weiler C, Nerlich AG, Bachmeier BE, et al.Expression and distribution of tumor necrosis factor alpha in human lumbar intervertebral discs: a study in surgical specimen and autopsy controls.Spine (Phila Pa 1976). 2005; 30(1):44-53; discussion 54. [23]Liu GZ, Ishihara H, Osada R, et al. Nitric oxide mediates the Change of proteoglycan synthesis in the human lumbar intervertebral disc in response to hydrostatic pressure. Spine; 2001; 26:134-141. [24]Genevay S, Finkh A, Mezin F, et al. Influence of cytokine inhibitors on concentration and active of MMP-1 and MMP-3 in disc herniation. Arthritis Res Ther, 2009, 11: R169. [25]Sadowski T, Steinmeyer J.Effects of non-steroidal antiinflammatory drugs and dexamethasone on the activity and expression of matrix metalloproteinase-1, matrix metalloproteinase-3 and tissue inhibitor of metalloproteinases-1 by bovine articular chondrocytes. Osteoarthritis Cartilage. 2001; 9(5):407-415. [26]Elfervig MK, Minchew JT, Francke E, et al. IL-1β Sensitizes Intervertebral Disc Annulus Cells to Fluid-Induced Shear Stress. J Cell Biochem.2001;82:290-298. [27]Keller TS, Kosmopoulos V, Lieberman IH.Vertebroplasty and kyphoplasty affect vertebral motion segment stiffness and stress distributions: a microstructural finite-element study.Spine (Phila Pa 1976). 2005; 30(11):1258-1265. [28]Kim JM, Shin DA, Byun DH, et al. Effect of bone cement volume and stiffness on occurrences of adjacent vertebral fractures after vertebroplasty. J Korean Neurosurg Soc.2012; 52 (5): 435-440. |
| [1] | Zhong Yuanming, Wan Tong, Zhong Xifeng, Wu Zhuotan, He Bingkun, Wu Sixian. Meta-analysis of the efficacy and safety of percutaneous curved vertebroplasty and unilateral pedicle approach percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 456-462. |
| [2] | Sun Jianwei, Yang Xinming, Zhang Ying. Effect of montelukast combined with bone marrow mesenchymal stem cell transplantation on spinal cord injury in rat models [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3962-3969. |
| [3] | Feng Guancheng, Fang Jianming, Lü Haoran, Zhang Dongsheng, Wei Jiadong, Yu Bingbing. How does bone cement dispersion affect the early outcome of percutaneous vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3450-3457. |
| [4] | Jiang Shengyuan, Li Dan, Jiang Jianhao, Shang-you Yang, Yang Shuye. Biological response of Co2+ to preosteoblasts during aseptic loosening of the prosthesis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3292-3299. |
| [5] | Sun Yiqiang, Xing Jianqiang, Li Xuecheng, Wang Xin, Tian Shenglan, Zhao Zihao, Geng Xiaopeng. Kyphoplasty versus vertebroplasty in the treatment of osteoporotic vertebral compression fracture in the elderly: a comparison of vertebral height recovery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2851-2855. |
| [6] | Li Qiang, Li Jun, Luan Jian, Jin Canghai, Hao Meng, Lin Yong. Bone cement distribution of percutaneous curved vertebroplasty for the treatment of osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(16): 2466-2471. |
| [7] | Zhong Yuanming, Wan Tong, Zhong Xifeng, Wu Zhuotan, He Bingkun, Wu Sixian. Meta-analysis of efficacy and safety of bone filling bag vertebroplasty and percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fracture#br# [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1930-1935. |
| [8] | Jing Wanli, Zhang Tao, Teng Donghui, Shi Tao, Zhou Qiang. Poor outcomes of bone filling mesh container vertebroplasty for the treatment of osteoporotic vertebral compression fractures with vertebral body wall incompetence [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(10): 1522-1527. |
| [9] | Zhang Zhiwei, Li Li, Huang Ziyu, Wu Duoyi, Gan Farong, Ye Baofei, Zhang Yan, Zhang Taibiao, Hu Wanjun. Percutaneous vertebroplasty through unilateral and bilateral pedicle approaches and unilateral pedicle extrapedicle approach for the treatment of thoracolumbar vertebral compression fractures: bone cement perfusion volume and cement leakage rate [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(9): 1353-1358. |
| [10] | Wang Yiya, Zhang Han, Lan Hai. Digital evaluation of finite element model for percutaneous kyphoplasty with bone cement injection [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(9): 1378-1383. |
| [11] | Ma Zhigang, Guo Liping, Zhang Jianning, Li Yonggang. Changes in related factors in synovial fluid of osteoarthritis rabbits after treatment with different molecular weights of sodium hyaluronate injection [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(5): 694-698. |
| [12] | Li Kaiming, Wang Shangquan, Li Linghui, Zhu Liguo, Zhang Qing, Xie Rui. Bone filling bag vertebroplasty and percutaneous kyphoplasty for the treatment of thoracolumbar osteoporotic compression fractures: a meta-analysis of improving Cobb angle and reducing bone cement leakage [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(4): 650-656. |
| [13] | Wang Xiuting, Li Sisheng, Sun Jian, Zhang Genyuan, Liu Fayin, Zhang Jintao. Effectiveness of artificial intelligent laser location system in reducing the location time and radiation dose of vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(33): 5295-5299. |
| [14] | Zhan Fangbiao, Xie Lizhong, Zou Xinsen, Long Jie, Cheng Jun, Zhang Xianwei. Efficacy and safety of percutaneous kyphoplasty versus posterior short-segment fixation with vertebra augmentation for Kummell’s disease: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(33): 5397-5404. |
| [15] | Zou Haibo, Sun Xiaofeng. Variation of Fas/Fasl pathway in limb ischemia-reperfusion lung injury rats after etomidate post-treatment [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(32): 5162-5167. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 138
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 243
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||