Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (12): 1930-1935.doi: 10.3969/j.issn.2095-4344.3792
Previous Articles Next Articles
Meta-analysis of efficacy and safety of bone filling bag vertebroplasty and percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fracture#br#
Zhong Yuanming1, Wan Tong2, Zhong Xifeng2, Wu Zhuotan2, He Bingkun2, Wu Sixian2
- 1First Affiliated Hospital of Guangxi University of Chinese Medicine, Nanning 530001, Guangxi Zhuang Autonomous Region, China; 2Graduate School of Guangxi University of Chinese Medicine, Nanning 530001, Guangxi Zhuang Autonomous Region, China
-
Received:2020-04-11Revised:2020-04-20Accepted:2020-06-12Online:2021-04-28Published:2020-12-26 -
Contact:Zhong Yuanming, First Affiliated Hospital of Guangxi University of Chinese Medicine, Nanning 530001, Guangxi Zhuang Autonomous Region, China -
About author:Zhong Yuanming, Doctoral supervisor, Professor, Chief physician, First Affiliated Hospital of Guangxi University of Chinese Medicine, Nanning 530001, Guangxi Zhuang Autonomous Region, China -
Supported by:the National Natural Science Foundation of China, No. 81760874 (to ZYM); the First Class Discipline Project of Traditional Chinese Medicine in Guangxi, No. GJKY [2018]12 (to ZYM)
CLC Number:
Cite this article
Zhong Yuanming, Wan Tong, Zhong Xifeng, Wu Zhuotan, He Bingkun, Wu Sixian. Meta-analysis of efficacy and safety of bone filling bag vertebroplasty and percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fracture#br#[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1930-1935.
share this article

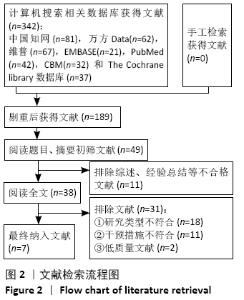
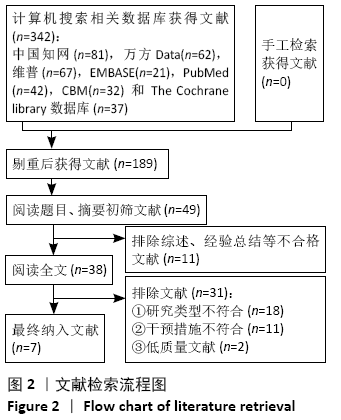
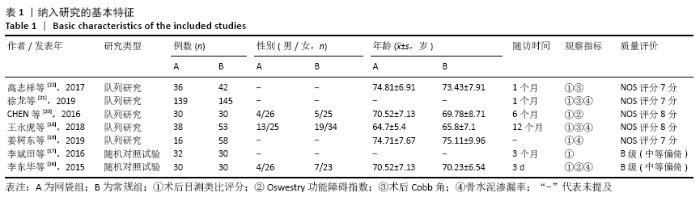
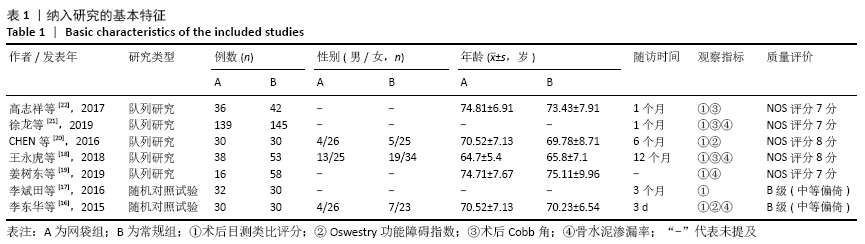
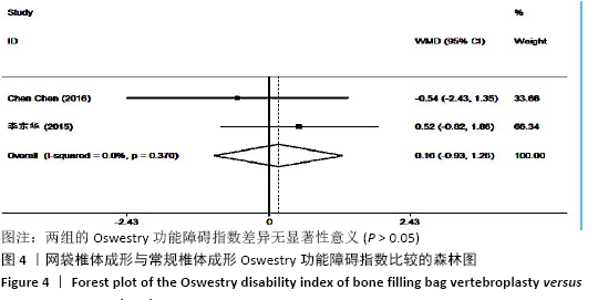
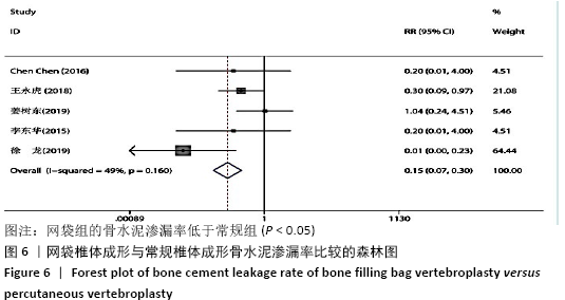
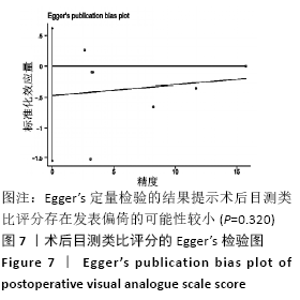
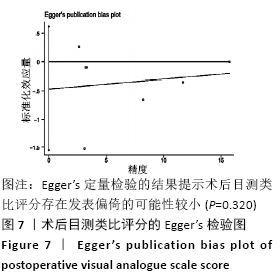
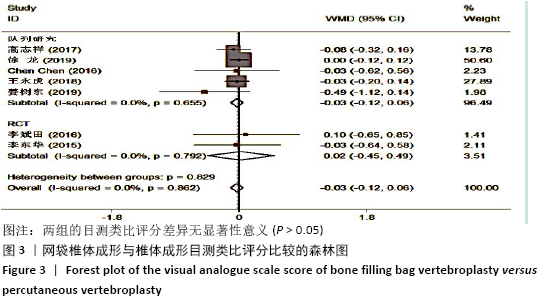
2.2 纳入研究文献质量 共纳入7个研究[16-22],有2个随机对照试验[16-17],5个队列研究[18-22]。2个随机对照试验均按随机原则进行病例分组,但未具体描述随机方法、分配、评价和脱落情况,文献等级评为B级;5个队列研究经NOS量表评价后,2个队列研究为8分,另外3个队列研究为7分,见表1。 2.3 Meta分析结果 2.3.1 各组术后目测类比评分变化 纳入的7个研究比较了两组患者经治疗后的目测类比评分[16-22]。固定效应模型Meta分析结果显示:网袋组与常规组的目测类比评分相比,差异无显著性意义(P > 0.05)。根据研究类型的不同进行亚组分析,固定效应模型Meta分析结果显示:①队列研究:网袋组与常规组的目测类比评分相比,差异无显著性意义(MD=-0.03,95%CI:-0.12-0.06,P > 0.05);②随机对照试验:网袋组与常规组的目测类比评分相比,差异无显著性意义(MD=0.02,95%CI:-0.45-0.49,P > 0.05),见图3。 "
| [1] 杨九杰,赵伟,王楠,等.脂肪间充质干细胞成骨分化条件培养基联合骨形态发生蛋白2治疗去卵巢大鼠骨质疏松症[J].中国组织工程研究, 2020,24(1):7-13. [2] MALIK AT, RETCHIN S, PHILLIPS FM, et al. Declining trend in osteoporosis management and screening following vertebral compression fractures - a national analysis of commercial insurance and medicare advantage beneficiaries. Spine J. 2020; 20(4):538-546. [3] SHIGENOBU K, HASHIMOTO T, KANAYAMA M, et al. The efficacy of osteoporotic treatment in patients with new spinal vertebral compression fracture pain, ADL, QOL, bone metabolism and fracture-healing-In comparison with weekly teriparatide with bisphosphonate. Bone Rep. 2019;11:100217. [4] ORHURHU V, AGUDILE E, CHU R, et al. Socioeconomic disparities in the utilization of spine augmentation for patients with osteoporotic fractures: an analysis of National Inpatient Sample from 2011 to 2015. Spine J. 2020;20(4):547-555. [5] 李凡杰,杜怡斌,刘艺明,等.椎体成形与弯角椎体成形治疗骨质疏松性椎体压缩骨折:骨水泥注射后分布与渗漏率的比较[J].中国组织工程研究,2020,24(10):1484-1490. [6] POURTAHERI S, LUO W, CUI C, et al. Vertebral augmentation is superior to nonoperative care at reducing lower back pain for symptomatic osteoporotic compression fractures. Clin Spine Surg. 2018;31(8):339-344. [7] HUANG S, ZHU X, XIAO D, et al. Therapeutic effect of percutaneous kyphoplasty combined with anti-osteoporosis drug on postmenopausal women with osteoporotic vertebral compression fracture and analysis of postoperative bone cement leakage risk factors: a retrospective cohort study. J Orthop Surg Res. 2019;14(1):1-12. [8] BALÁZSFI M, KIS D, TÓTH T, et al. Radiofrequency facet joint denervation efficiency based on the severity of spondylarthrosis and in osteoporotic vertebral compression fractures. A retrospective study. Clin Neurol Neurosurg. 2019;186:105497. [9] OH Y, LEE B, LEE S, et al. Percutaneous vertebroplasty versus conservative treatment using a transdermal fentanyl patch for osteoporotic vertebral compression fractures. J Korean Neurosurg Soc. 2019;62(5):594. [10] XIE L, ZHAO ZG, ZHANG SJ, et al. Percutaneous vertebroplasty versus conservative treatment for osteoporotic vertebral compression fractures: an updated meta-analysis of prospective randomized controlled trials. Int J Surg. 2017;47:25-32. [11] KHAN M, KUSHCHAYEV SV. Percutaneous vertebral body augmentations: the state of art. Neuroimaging Clin N Am. 2019;29(4):495-513. [12] ZUO XH, ZHU XP, BAO HG, et al. Network meta-analysis of percutaneous vertebroplasty, percutaneous kyphoplasty, nerve block, and conservative treatment for nonsurgery options of acute/subacute and chronic osteoporotic vertebral compression fractures (OVCFs) in short-term and long-term effects. Medicine (Baltimore). 2018;97(29):e11544. [13] ALHASHASH M, SHOUSHA M, BARAKAT AS, et al. Effects of polymethylmethacrylate cement viscosity and bone porosity on cement leakage and new vertebral fractures after percutaneous vertebroplasty: a prospective study. Global Spine J. 2019;9(7):754-760. [14] KLINGLER JH, SIRCAR R, DEININGER MH, et al. Vesselplasty: a new minimally invasive approach to treat pathological vertebral fractures in selected tumor patients-preliminary results. Rofo. 2013;185(4):340-350. [15] 印平,马远征,马迅,等.骨质疏松性椎体压缩性骨折的治疗指南[J].中国骨质疏松杂志,2015, 21(6):643-648. [16] 李东华,刘训伟,彭湘涛,等.骨填充网袋灌注骨水泥修复椎体压缩骨折:可降低骨水泥椎体外渗漏率[J].中国组织工程研究,2015,19(3):358-363. [17] 李斌田. PVP、PKP、扩张型编织囊袋椎体后凸成形术在治疗新鲜胸腰椎骨质疏松性压缩骨折的临床疗效分析[D].济南:山东中医药大学,2016. [18] 王永虎.网袋椎体成形术与常规PVP手术治疗骨质疏松性椎体压缩骨折的疗效对比[J].颈腰痛杂志,2018,39(6):745-747. [19] 姜树东,洪毅,张军卫,等.椎体成形与网袋成形治疗骨质疏松性骨折早期效果比较[J].中国矫形外科杂志,2019,27(4):289-293. [20] CHEN C, LI D, WANG Z, et al. Safety and efficacy studies of vertebroplasty, kyphoplasty, and mesh-container-plasty for the treatment of vertebral compression fractures: preliminary report. PLoS One. 2016;11(3):e0151492. [21] 徐龙,辛健.PVP、PKP、囊袋治疗新鲜骨质疏松性椎体压缩骨折的临床分析[J].中国矫形外科杂志,2019,27(19):1812-1815. [22] 高志祥,李淳,李磊,等.PVP、PKP、骨填充网袋治疗胸腰段骨质疏松性椎体压缩性骨折的疗效分析[J].实用骨科杂志, 2017,23(8):680-683, 697. [23] YANG S, CHEN C, WANG H, et al. A systematic review of unilateral versus bilateral percutaneous vertebroplasty/percutaneous kyphoplasty for osteoporotic vertebral compression fractures. Acta Orthop Traumatol Turc. 2017;51(4):290-297. [24] LI HM, ZHANG RJ, GAO H, et al. New vertebral fractures after osteoporotic vertebral compression fracture between balloon kyphoplasty and nonsurgical treatment PRISMA. Medicine. 2018; 97(40):e12666. [25] SUN X, LIU X, WANG J, et al. The effect of early limited activity after bipedicular percutaneous vertebroplasty to treat acute painful osteoporotic vertebral compression fractures. Pain Physician. 2020;23(1):E31-E40. [26] JACOBS E, SENDEN R, MCCRUM C, et al. Effect of a semirigid thoracolumbar orthosis on gait and sagittal alignment in patients with an osteoporotic vertebral compression fracture. Clin Interv Aging. 2019;14:671-680. [27] CHEN YC, ZHANG L, LI EN, et al. Unilateral versus bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures in elderly patients: a meta-analysis. Medicine. 2019; 98(8):e14317. [28] ZHANG Z, JIAO F, HUANG H, et al. A second puncture and injection technique for treating osteoporotic vertebral compression fractures. J Orthop Surg Res. 2019;14(1):1-7. [29] ZHU RS, KAN SL, NING GZ, et al. Which is the best treatment of osteoporotic vertebral compression fractures: balloon kyphoplasty, percutaneous vertebroplasty, or non-surgical treatment? A Bayesian network meta-analysis. Osteoporos Int. 2019;30(2):287-298. [30] LI J, LIN JS, XU JC, et al. A novel approach for percutaneous vertebroplasty based on preoperative computed tomography–based three-dimensional model design. World Neurosurg. 2017;105:20-26. [31] ZHU Y, CHENG J, YIN J, et al. Therapeutic effect of kyphoplasty and balloon vertebroplasty on osteoporotic vertebral compression fracture: A systematic review and meta-analysis of randomized controlled trials. Medicine. 2019; 98(45):e17810. [32] GUO D, YU M, ZHANG S, et al. Novel Surgical Strategy for Treating Osteoporotic Vertebral Fractures with Cord Compression. Orthop Surg. 2019;11(6):1082-1092. [33] YANG J. Correlation between the distribution of bone cement and clinical efficacy in the treatment of osteoporotic spinal fractures with percutaneous vertebroplasty. Zhongguo Gu Shang. 2019;32(12):1128. [34] TIAN J, XIANG L, ZHOU D, et al. The clinical efficacy of vertebroplasty on osteoporotic vertebral compression fracture: a meta-analysis. Int J Surg. 2014;12(12):1249-1253. [35] ZHOU X, MENG X, ZHU H, et al. Early versus late percutaneous kyphoplasty for treating osteoporotic vertebral compression fracture: a retrospective study. Clin Neurol Neurosurg. 2019;180:101-105. [36] YEH KL, WU SH, WU SS, et al. Rare episode of cement leakage during vesselplasty in a case of vertebral compression fracture. World Neurosurg. 2020;137:416-420. [37] FUSCO A. Benefits and harms of percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fracture: a cochrane review summary with commentary. Am J Phys Med Rehabil. 2019;98(12):1151-1152. [38] WANG B, ZHAO CP, SONG LX, et al. Balloon kyphoplasty versus percutaneous vertebroplasty for osteoporotic vertebral compression fracture: a meta-analysis and systematic review. J Orthop Surg Res. 2018;13(1):264. [39] FLORS L, LONJEDO E, LEIVA-SALINAS C, et al. Vesselplasty: a new technical approach to treat symptomatic vertebral compression fractures. Am J Roentgenol. 2009;193(1):218-226. [40] DUAN ZK, ZOU JF, HE XL, et al. Bone-filling mesh container versus percutaneous kyphoplasty in treating Kümmell’s disease. Arch Osteoporos. 2019;14(1):109. [41] ZHONG R, LIU J, WANG R, et al. Unilateral curved versus bipedicular vertebroplasty in the treatment of osteoporotic vertebral compression fractures. BMC Surg. 2019;19(1):193. |
| [1] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [2] | Jiang Yong, Luo Yi, Ding Yongli, Zhou Yong, Min Li, Tang Fan, Zhang Wenli, Duan Hong, Tu Chongqi. Von Mises stress on the influence of pelvic stability by precise sacral resection and clinical validation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1318-1323. |
| [3] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [4] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [5] | Li Dadi, Zhu Liang, Zheng Li, Zhao Fengchao. Correlation of total knee arthroplasty efficacy with satisfaction and personality characteristics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1346-1350. |
| [6] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [7] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [8] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [9] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [10] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [11] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [12] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [13] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [14] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [15] | Zhang Shangpu, Ju Xiaodong, Song Hengyi, Dong Zhi, Wang Chen, Sun Guodong. Arthroscopic suture bridge technique with suture anchor in the treatment of acromioclavicular dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1417-1422. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 189
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 500
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||