Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (32): 5162-5167.doi: 10.3969/j.issn.2095-4344.2865
Previous Articles Next Articles
Variation of Fas/Fasl pathway in limb ischemia-reperfusion lung injury rats after etomidate post-treatment
Zou Haibo, Sun Xiaofeng
Affiliated Central Hospital, Shenyang Medical College, Shenyang 110000, Liaoning Province, China
-
Received:2019-11-19Revised:2019-11-22Accepted:2020-01-22Online:2020-11-18Published:2020-09-25 -
Contact:Sun Xiaofeng, MD, Chief physician, Affiliated Central Hospital, Shenyang Medical College, Shenyang 110000, Liaoning Province, China -
About author:Zou Haibo, Master, Associate chief physician, Affiliated Central Hospital, Shenyang Medical College, Shenyang 110000, Liaoning Province, China -
Supported by:the Liaoning Provincial Science and Technology Plan, No. 20180550621; the General Project of Liaoning Provincial Education Department, No. L2015540; the Youth Foundation of Shenyang Medical College, No. 20162029 and 20191013
CLC Number:
Cite this article
Zou Haibo, Sun Xiaofeng. Variation of Fas/Fasl pathway in limb ischemia-reperfusion lung injury rats after etomidate post-treatment[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(32): 5162-5167.
share this article
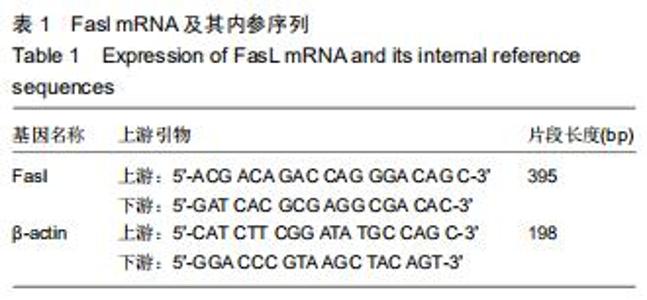
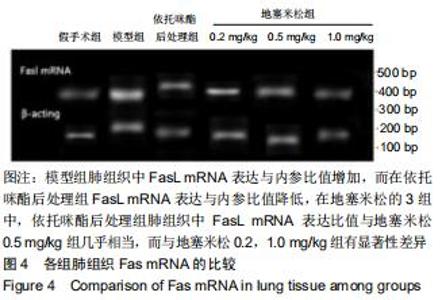
1.4.7 反转录-聚合酶链反应(RT-PCR)检测 应用PCR扩增仪(Biometra,德国)检测肺组织中Fasl mRNA的表达:取左肺下极1 cm3制备10%肺组织匀浆,Trizol法(Invitrogen,美国)抽提总RNA,反转录合成cDNA,然后应用PCR扩增仪进行扩增,Fasl mRNA引物[宝生物工程(大连)有限公司]序列如表1。Fasl mRNA反应条件:94 ℃预变性2 min;95 ℃ 45 s,57 ℃ 45 s,72 ℃ 60 s,35个循环;72 ℃延伸5 min。β-actin反应条件:94 ℃预变性2 min;94 ℃ 40 s,58 ℃ 40 s,72 ℃ 60 s,30个循环;72 ℃延伸 5 min。扩增产物经2%琼脂糖凝胶电泳,溴乙锭染色,凝胶成像仪成像。采用Scion Image图像分析系统分析仪目的产物与β-actin灰度值的比值反映Fasl mRNA表达水平。 "
|
[1] 邹海波,孙晓峰.姜黄素后处理肢体缺血再灌注肾损伤模型大鼠基质金属蛋白酶9及基质金属蛋白酶组织抑制因子1平衡的变化[J].中国组织工程研究,2019,23(23):3643-3648.
[2] 邹海波,孙晓峰.姜黄素后处理对大鼠肢体缺血再灌注肺损伤的影响[J].沈阳药科大学学报.2019.
[3] TSAROUCHA AK, VALSAMI G, KOSTOMITSOPOULOS N, et al. Silibinin Effect on Fas/FasL, HMGB1, and CD45 Expressions in a Rat Model Subjected to Liver Ischemia-Reperfusion Injury. J INVEST SURG. 2018;31(6):491-502.
[4] ZHU Y, YIN X. Overexpression of microRNA-204-5p alleviates renal ischemia-reperfusion injury in mice through blockage of Fas/FasL pathway. Exp Cell Res. 2019;381(2):208-214.
[5] 邹海波,孙晓峰.姜黄素后处理对缺血再灌注肾损伤大鼠Notch2/Hes-1通路的影响[J].中国现代医学杂志,2019,29(19):17-22.
[6] 李丽萌,郑晓春,郑艇,等.肢体缺血预处理对大鼠肝缺血再灌注诱发肠损伤和脑损伤的影响[J].中华麻醉学杂志,2018,38(1):105-109.
[7] ZOU HB, SUN XF. Post-treatment curcumin reduced ischemia- reperfusion-induced pulmonary injury via the Notch2/Hes-1 pathway. J Int Med Res. 2019.DOI: 10.1177/0300060519892432.
[8] ZHENG MX, SONG D, LUO ZY. Effect of puerarin on expression of Fas/FasL mRNA in pulmonary injury induced by ischemia-reperfusion in rabbits. Nat Prod Commun. 2015;10(2):252-256.
[9] 陈靖宜,柯昌斌,谢华.依托咪酯预处理对肺缺血再灌注损伤的影响[J].现代中西医结合杂志,2016,25(12):1285-1287.
[10] 王建军,刘亚楠,王建辉,等.二乙酰胺三氮脒对肢体缺血再灌注模型小鼠肾损伤的保护作用及其机制[J].吉林大学学报(医学版),2020,1:14-19.
[11] 武莉,曹定睿,刘臻.依托咪酯后处理对大鼠肝缺血再灌注肾细胞凋亡及Bcl-2和Bax表达的影响[J].中国药物与临床,2015,15(4):480-482.
[12] MCGRATH M, HOFMANN A, RAINES DE. Behavioral and steroidogenic pharmacology of phenyl ring substituted etomidate analogs in rats. BMC Pharmacol Toxicol. 2019;20:48.
[13] LIU X, SONG H, YANG J, et al. The etomidate analog ET-26 HCl retains superior myocardial performance: comparisons with etomidate in vivo and in vitro. PLoS One. 2018;13(1):1-13.
[14] NIIKAWA H, OKAMOTO T, AYYAT KS, et al. The protective effect of prone lung position on ischemia-reperfusion injury and lung function in an ex vivo porcine lung model. J Thorac Cardiovasc Surg. 2019;157(1): 425-433.
[15] 邓红,高静,刘金碧,等.依托咪酯对大鼠肺缺血再灌注损伤时NF-kB活性的影响[J].中华麻醉学杂志,2017,37(4):498-500.
[16] LEE B, LEE DG. Reactive oxygen species depletion by silibinin stimulates apoptosis-like death in escherichia coli. J Microbiol Biotechnol. 2017;27(12):12.
[17] 邓红,丁永永,彭捷.依托咪酯对大鼠脑缺血再灌注损伤的保护作用及机制[J].华西药学杂志,2017,32(4):381-384.
[18] RATHORE VS, GUPTA S. A Comparative study of propofol, etomidate and 50% admixture of etomidate and propofol for induction in general anaesthesia. J Dent Med Sci. 2018. DOI: 10.9790/0853-1707124145.
[19] 李睿,张立民,罗星,等.依托咪酯后处理对大鼠缺氧缺糖一复糖复氧皮质神经元线粒体通透性转换孔的影响:与Robo受体的关系[J].中华麻醉学杂志, 2016,36(2):253-256.
[20] ZHAO XR, ZHANG Z, GAO M, et al. MicroRNA-27a-3p aggravates renal ischemia/reperfusion injury by promoting oxidative stress via targeting growth factor receptor-bound protein 2. Pharmacol Res. 2020;18:104718.
[21] BISHT M, POKHRIYAL AS, KHURANA G, et al. Effect of Fentanyl and Nalbuphine for Prevention of Etomidate-Induced Myoclonus. Anesth Essays Res. 2019;13(1):119-125.
[22] MCGRATH M, MA C, RAINES DE. Dimethoxy-etomidate: a nonhypnotic etomidate analog that potently inhibits steroidogenesis. J Pharmacol Exp Ther. 2018;364(2):229-237.
[23] 张效云,宋桂芹,辇晓峰.阻断白介素-17对博来霉素诱导小鼠肺纤维化及肺组织Fas/FasL表达的影响[J].南京医科大学学报,2017,37(5):584-587.
[24] 杨迎春,王瑞芳,陈新骥,等.高血脂大鼠脑缺血再灌注损伤后Bcl-2和Bax的表达变化及灯盏乙素的影响[J].解剖学报,2019,50(4):431-437.
[25] 张红健,宋杨,杨明.pEGFP-N1-IL-17通过调控Fas/FasL信号通路影响喉癌Hep-2细胞的凋亡[J].安徽医科大学学报,2019,54(11):1683-1687.
[26] ALCOVERRO-FORTUNY Ò, ALARCÓN BG, USAN FV, et al. Etomidate improves seizure adequacy during electroconvulsive therapy. Psychiatry Res. 2019;273:350-354.
[27] JANYOU A, WICHA P, SEECHAMNANTURAKIT V, et al. Dihydrocapsaicin-induced angiogenesis and improved functional recovery after cerebral ischemia and reperfusion in a rat model. J Pharmacol Sci. 2020. DOI: 10.1016/j.jphs.2020.02.001.
[28] LEE JM, MIN G, LEE JM, et al. Efficacy and safety of etomidate– midazolam for screening colonoscopy in the elderly. Medicine. 2018; 97(20):e10635.
[29] 王振宇,彭红军,陈思,等.依托咪酯对老年冠心病患者非心脏手术中血流动力学及肌钙蛋白I和超敏C反应蛋白的影响[J].广东医学,2016,37(z1): 216-218.
[30] 李卫星,叶西就,韩海华.依托咪酯靶控输注复合瑞芬太尼诱导对中老年高血压患者血流动力学的影响及临床麻醉效果[J].北方药学,2016,13(9): 52.
[31] 张霖,耿庆,范涛,等.香草乙酮静注对大鼠肺缺血再灌注损伤的预防作用观察[J].山东医药,2020,3:30-33.
[32] 王继武,陈小珍,徐志强,等.核因子E2相关因子2信号通路对肺缺血再灌注损伤的保护机制[J].中华实验外科杂志,2019,36(8):1430-1432. |
| [1] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [2] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [3] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [4] | Shu Wenbo, Chen Mengchi, Li Hua, Huang Liqian, Huang Binbin, Zhang Wenhai, Wu Yachen, Wang Zefeng, Li Qiaoli, Liu Peng. Correlation between body fat distribution and characteristics of daily physical activity in college students [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1277-1283. |
| [5] | Ji Zhixiang, Lan Changgong. Polymorphism of urate transporter in gout and its correlation with gout treatment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1290-1298. |
| [6] | Wu Xun, Meng Juanhong, Zhang Jianyun, Wang Liang. Concentrated growth factors in the repair of a full-thickness condylar cartilage defect in a rabbit [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1166-1171. |
| [7] | Shen Jinbo, Zhang Lin. Micro-injury of the Achilles tendon caused by acute exhaustive exercise in rats: ultrastructural changes and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1190-1195. |
| [8] | Zeng Zhen, Hu Jingwei, Li Xuan, Tang Linmei, Huang Zhiqiang, Li Mingxing. Quantitative analysis of renal blood flow perfusion using contrast-enhanced ultrasound in rats with hemorrhagic shock during resuscitation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1201-1206. |
| [9] | Tang Hui, Yao Zhihao, Luo Daowen, Peng Shuanglin, Yang Shuanglin, Wang Lang, Xiao Jingang. High fat and high sugar diet combined with streptozotocin to establish a rat model of type 2 diabetic osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1207-1211. |
| [10] | Chai Le, Lü Jianlan, Hu Jintao, Hu Huahui, Xu Qingjun, Yu Jinwei, Quan Renfu. Signal pathway variation after induction of inflammatory response in rats with acute spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1218-1223. |
| [11] | Liu Xiangxiang, Huang Yunmei, Chen Wenlie, Lin Ruhui, Lu Xiaodong, Li Zuanfang, Xu Yaye, Huang Meiya, Li Xihai. Ultrastructural changes of the white zone cells of the meniscus in a rat model of early osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1237-1242. |
| [12] | Liu Cong, Liu Su. Molecular mechanism of miR-17-5p regulation of hypoxia inducible factor-1α mediated adipocyte differentiation and angiogenesis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1069-1074. |
| [13] | Wang Zhengdong, Huang Na, Chen Jingxian, Zheng Zuobing, Hu Xinyu, Li Mei, Su Xiao, Su Xuesen, Yan Nan. Inhibitory effects of sodium butyrate on microglial activation and expression of inflammatory factors induced by fluorosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1075-1080. |
| [14] | Wan Ran, Shi Xu, Liu Jingsong, Wang Yansong. Research progress in the treatment of spinal cord injury with mesenchymal stem cell secretome [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1088-1095. |
| [15] | Xie Wenjia, Xia Tianjiao, Zhou Qingyun, Liu Yujia, Gu Xiaoping. Role of microglia-mediated neuronal injury in neurodegenerative diseases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1109-1115. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||