Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (4): 555-560.doi: 10.3969/j.issn.2095-4344.1890
Previous Articles Next Articles
Clinical outcomes of drug-eluting balloons and drug-eluting stents for the treatment of in-stent restenosis
Xie Xiufeng, Zhang Yue, Qu Ze
- Second District of Geriatrics Center, the Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010050, Inner Mongolia Autonomous Region, China
-
Received:2019-05-09Revised:2019-05-23Accepted:2019-06-27Online:2020-02-08Published:2020-01-04 -
Contact:张越,主任医师,硕士生导师,内蒙古医科大学附属医院老年医学中心二区,内蒙古自治区呼和浩特市 010050 -
About author:Xie Xiufeng, MD, Associate chief physician, Second District of Geriatrics Center, the Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010050, Inner Mongolia Autonomous Region, China
CLC Number:
Cite this article
Xie Xiufeng, Zhang Yue, Qu Ze. Clinical outcomes of drug-eluting balloons and drug-eluting stents for the treatment of in-stent restenosis[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(4): 555-560.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
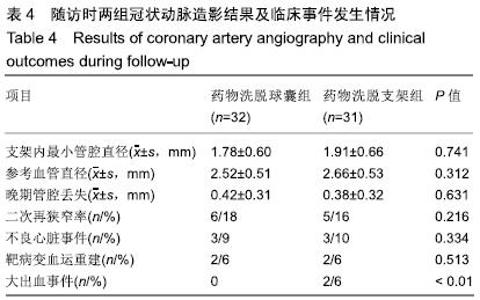
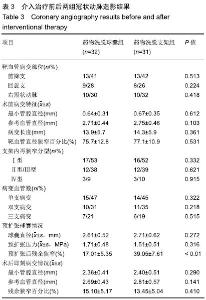
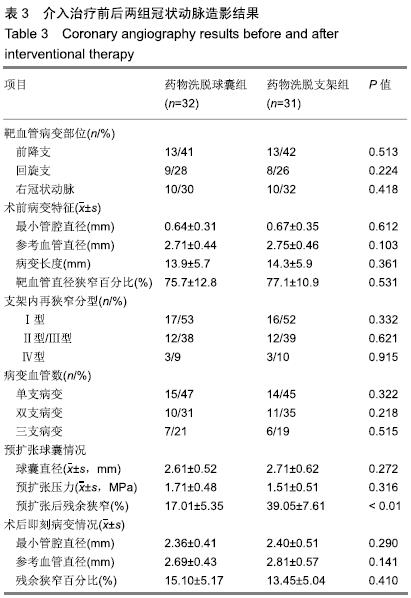
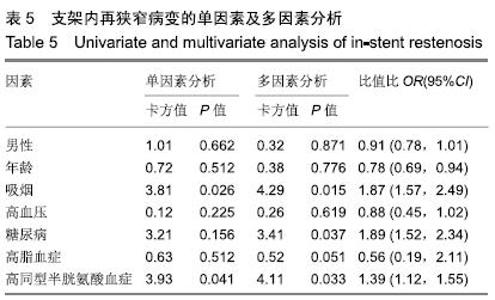
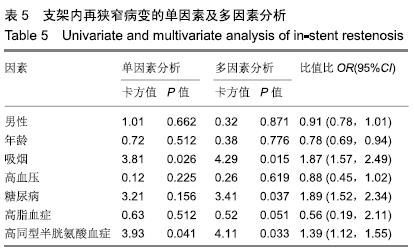
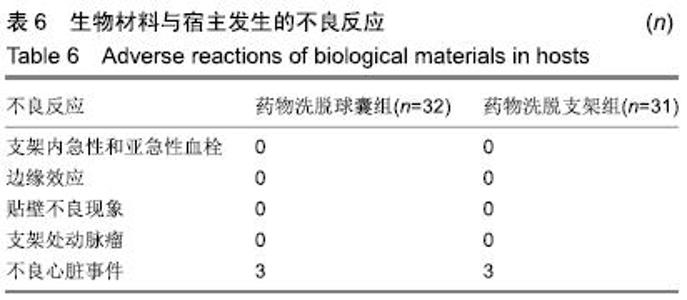
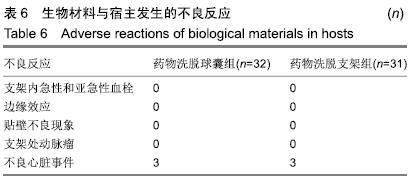
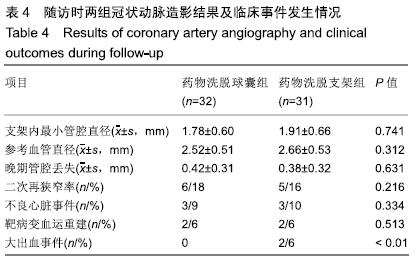
两组间支架内再狭窄的病变靶血管主要分布在前降支、右冠状动脉及回旋支,且两组病变靶血管分布比例、病变血管数比较差异无显著性意义(P > 0.05)。另外,两组间的最小管腔直径、参考管腔直径、病变长度及管腔狭窄率比较差异无显著性意义(P > 0.05)。两组预扩张情况中球囊直径及预扩张压力比较差异无显著性意义意义(P > 0.05),但是预扩张后残余狭窄药物洗脱支架组大于药物洗脱球囊组(P < 0.01),术后两组即刻残余狭窄百分比比较无显著性意义(P > 0.05),见表3。 2.5 术后随访结果 两组支架内最小管腔直径、参考血管直径、支架内狭窄率、支架内晚期管腔丢失比较均无显著性意义(P均> 0.05),并且两组治疗支架内再狭窄后二次再狭窄概率比较差异无显著性意义(18%,16%,P=0.216);两组治疗后靶病变血运重建情况、主要不良心脏事件事件情况比较差异无显著性意义(P=0.513,P=0.334);随访过程中有药物洗脱支架组有2例出现消化道大出血,两组间比较差异有显著性意义(P < 0.01),见表4。"
| [1] AKIN I, NIENABER CA.Treatment of coronary in-stent restenosis—evidence for universal recommendation? J Thorac Dis.2015;7(10):1672-1675. [2] SIONTIS GC, STEFANINI GG, MAVRIDIS D, et al. Percutaneous coronary interventional strategies for treatment of in-stent restenosis: a network meta-analysis.Lancet. 2015; 386(9994):655-664. [3] RITTGER H, WALISZEWSKI M, BRACHMANN J, et al. Long-Term Outcomes After Treatment With a Paclitaxel- Coated Balloon Versus Balloon Angioplasty: Insights From the PEPCAD-DES Study (Treatment of Drug-eluting Stent [DES] In-Stent Restenosis With SeQuent Please Paclitaxel- Coated Percutaneous Transluminal Coronary Angioplasty [PTCA] Catheter). JACC Cardiovasc Interv.2015;8(13): 1695-1700. [4] UNVERDORBEN M, VALLBRACHT C, CREMERS B, et al. Paclitaxel-coated balloon catheter versus paclitaxel-coated stent for the treatment of coronary in-stent restenosis: the three-year results of the PEPCAD II ISR study. EuroIntervention.2015;11(8):926-934. [5] ALFONSO F, PÉREZ-VIZCAYNO MJ, CÁRDENAS A, et al. A Prospective Randomized Trial of Drug-Eluting Balloons Versus Everolimus-Eluting Stents in Patients With In-Stent Restenosis of Drug-Eluting Stents: The RIBS IV Randomized Clinical Trial.J Am Coll Cardiol.2015;66(1):23-33. [6] INDERMUEHLE A, BAHL R, LANSKY AJ, et al.Drug-eluting balloon angioplasty for in-stent restenosis: a systematic review and meta-analysis of randomised controlled trials. Heart.2013;99(5):327-333. [7] KLEBER FX ,RITTGER H, BONAVENTURA K, et al. Drug-coated balloons for treatment of coronary artery disease: updated recommendations from a consensus group. Clin Res Cardiol.2013;102(11):785-797. [8] JAMSHIDI P, NYFFENEGGER T, SABTI Z, et al.A novel approach to treat in-stent restenosis: 6- and 12-month results using the everolimuseluting bioresorbable vascular scaffold. EuroIntervention.2016;11(13):1479-1486. [9] BNAA KH, MANNSVERK J, WISETH R, et al.Drug-Eluting or Bare-MetalStents for Coronary Artery Disease.N Engl J Med. 2016;375(13):1242-1252. [10] LEE JM, PARK J, KANG J, et al.Comparison among drug-eluting balloon,drug-eluting stent, and plain balloon angioplasty for the treatment of in-stent restenosis: a network meta-analysis of 11 randomized, controlled trials.JACC Cardiovasc Interv.2015;8(3):382-394. [11] 田宏伟,乔树宾.药物涂层球囊的研究进展[J].中国循环杂志, 2017,32(11):1134-1136. [12] WAKSMAN R, PAKALA R.Drug-eluting balloon: the comeback kid? Circ Cardiovasc Interv. 2009;2(4):352-358. [13] SCHELLER B, HEHRLEIN C, BOCKSCH W, et al.Treatment of coronary instent restenosis with a paclitaxel-coated balloon catheter.N Engl J Med.2006;355(20):2113-2124. [14] 中国成人血脂异常防治指南修订联合委员会.中国成人血脂异常防治指南(2016修订版) [J].中华心血管病杂志, 2016,44(10): 833-853. [15] 中国高血压防治指南修订委员会,高血压联盟(中国),中华医学会心血管病学分会,等.中国高血压防治指南(2018年修订版)[J].中国心血管杂志,2019,24(1):24-56. [16] IAKOVOU I, SCHMIDT T, GE L, et al. Angiographic patterns of restenosis after paclitaxel-eluting stent implantation.J Am Coll Cardiol.2005;45(5):805-806. [17] CAI JZ, ZHU YX, WANG XY, et al.Comparison of new-generation drug-eluting stents versus drug-coated balloon for in-stent restenosis: a meta-analysis of randomised controlled trials. BMJ Open.2018;8(2):e017231. [18] BASAVARAJAIAH S, NAQANUMA T, LATIB A, et al. Treatment of drugeluting stent restenosis: Comparison between drug-eluting balloon versus second-generation drug-eluting stents from a retrospectiveobservational study.Catheter Cardiovasc Interv.2016;88(4):522-528. [19] BYRNE RA, NEUMANN FJ, MEHILLI J, et al. Paclitaxel-eluting balloons,paclitaxel-eluting stents, and balloon angioplasty in patients with restenosis after implantation of a drug-eluting stent (ISARDESIRE 4):a randomised,open-label trial.Lancet.2013;381(9865):461-467. [20] HABARA S, KADOTA K, SHIMADA T, et al.Late Restenosis After Paclitaxel-Coated Balloon Angioplasty Occurs in Patients With Drug-Eluting Stent Restenosis.J Am Coll Cardiol. 2015;66(1):14-22. [21] CREMERS B, BIEDERMANN M, MAHNKOPF D, et al. Comparison of two different paclitaxel-coated balloon catheters in the porcine coronary restenosis model.Clin Res Cardiol.2009;98(5):325-330. [22] NAGANUMA T, LATIB A, SGUEGLIA GA, et al.A 2-year follow-up of a randomized multicenter study comparing a paclitaxel drug-eluting balloon with a paclitaxel-eluting stent in small coronary vessels the BELLO study.Int J Cardio. 2015; 184(8):17-21. [23] LIOU K, JEPSON N, CAO C, et al.Drug-eluting Balloon Versus Second Generation Drug Eluting Stents in the Treatment of In-stent Restenosis: A Systematic Review and Meta-analysis. Heart Lung Circ.2016;25(12):1184-1194. [24] MAMUTI W, ABLIMIT A, KELIMU W, et al.Comparison of drugeluting balloon versus drug-eluting stent in patients with in-stent restenosis: insight from randomized controlled trials. Int J Cardio.2015;179(1):424-429. [25] 蔡金赞,陈凯伦,贾海波,等.普通球囊、药物涂层球囊及药物洗脱支架治疗冠状动脉支架内再狭窄的长期疗效Meta分析[J].中国循环杂志,2018,33(9):837-878. [26] KUBO S, KADOTA K, OTSURU S, et al.Optimal treatment of recurrent restenosis lesions after drug-eluting stent implantation for in-stent restenosis lesions.EuroIntervention 2013;9(7):788-796 [27] NAVARESE EP, AUSTIN D, GURBEL PA, et al. Drug-coated balloons in treatment of in-stent restenosis:a meta-analysis of randomised controlled trials.Clin Res Cardiol.2013;102(4): 279-287. [28] WANG Y, LOU X, XU X, et al. Drug-eluting balloons versus drugeluting stents for the management of in-stent restenosis: a metaanalysis of randomized and observational studies. J Cardiol.2017;70(5):446-453. [29] 张文广,裴汉军,吴永健,等.药物洗脱支架治疗糖尿病合并冠状动脉支架内再狭窄远期疗效及安全性观察[J].中国循环杂志, 2013, 28(2):96-99. [30] KUFNER S, CASSESE S, VALESKINI M, et al. Long-Term Eficacy and Safety of Paclitaxel-Eluting Balloon for the Treatment of Drug-Eluting Stent Restenosis: 3-Year Results of a Randomized Controlled Trial. JACC Cardiovasc Interv. 2015;8(7):877-884. |
| [1] | Wu Kai, Liu Kun, Xie Lin, Lu Guanjun, Ma Shengchao, Li Guizhong, Cao Jun, Jie Yuzhen, Jiang Yideng, Hao Yinju. Mechanism of hyperhomocysteinemia induced renal injury in Cbs+/- mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(11): 1728-1732. |
| [2] | Wan Huazhe, Chai Guangxin, Xiao Xiaoling, Huang Wenying. Effects of phellinus igniarius crude polysaccharides on sporting ability and free radical metabolism of skeletal muscle in mice suffering passive smoking [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(5): 689-693. |
| [3] |
Zheng Haijun, Jin Hui, Cui Hongling, Zhu Yakun, Zeng Hui, Han Fengjie, Qiu Cuiting, Liu Jing.
Safety of drug-coated balloon versus drug-eluting stents in the treatment of type 2 diabetes mellitus complicated by coronary artery small vessel disease in older adult patients [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(28): 4573-4579. |
| [4] | Zhang Shuangyuan, Li Wenjin, Zhu Li, Wang Yu, Wei Zhoudan, Zhao Jiaoyang, Chen Yanan. Meta-analysis of dental implantation success rate in diabetic patients with 6% < glycated hemoglobin level < 8% [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(16): 2620-2624. |
| [5] |
Jin Hui, Li Meng.
A novel single-sided groove target release biodegradable stent inhibits coronary artery intimal hyperplasia [J]. Chinese Journal of Tissue Engineering Research, 2017, 21(26): 4222-4227. |
| [6] |
Wu Jin.
Screening and application of drug-eluting stents in patients with cardiovascular diseases
[J]. Chinese Journal of Tissue Engineering Research, 2016, 20(38): 5770-5776.
|
| [7] | Fang Ling-hai, Ying Hai-rong, Sun Wei . Rapamycin- and paclitaxel-eluting stents for prevention of cardiovascular events: effectiveness and safety [J]. Chinese Journal of Tissue Engineering Research, 2015, 19(8): 1223-1227. |
| [8] | Yang Feng, Zhao Qian, Zhang Shi-xuan, Zhao Tie-nan, Feng Bo. Specificity to capture endothelial progenitor cells in the peripheral blood by CD34 antibody applied on a rapamycin eluting stent [J]. Chinese Journal of Tissue Engineering Research, 2015, 19(41): 6694-6698. |
| [9] | Chi Xin-dong, Mayinuer Simailahong, Gan Qing-lei, Yang Na. Biodegradable sirolimus eluting stents in coronary artery stenosis: a safety evaluation [J]. Chinese Journal of Tissue Engineering Research, 2015, 19(34): 5501-5505. |
| [10] | Zhang Jin-ru, Wang Dong-mei. Effect of heparin slow-release stent on angiogenesis and cardiac function of patients with acute myocardial infarction [J]. Chinese Journal of Tissue Engineering Research, 2015, 19(30): 4815-4819. |
| [11] | Jia Ming-li. Short-term prognostic implication for patients with ST-elevation myocardial infarction undergoing domestic rapamycin drug-eluting stent implantation [J]. Chinese Journal of Tissue Engineering Research, 2015, 19(12): 1878-1883. |
| [12] | Xie Yu-xia, Shi Xue-kun, Yang Jie, Wu Gang, Cheng Lu, Qiao Rui. Predictive factors for in-stent late loss and non-culprit coronary lesion progression in diabetic patients undergoing drug eluting stenting [J]. Chinese Journal of Tissue Engineering Research, 2014, 18(30): 4906-4910. |
| [13] | Zhu Jian-hua, Wang Ying, Zhao Zhong-nan, Liu Ji-guang. Smoking promotes the resorption of periodontal alveolar bone [J]. Chinese Journal of Tissue Engineering Research, 2014, 18(20): 3172-3177. |
| [14] | Wang Shi-xiong, Li Ning-yin, Zhao Qi-ming, Gao Bing-ren. Off-pump coronary artery bypass grafting treats high-risk coronary heart disease [J]. Chinese Journal of Tissue Engineering Research, 2013, 17(5): 920-930. |
| [15] | Li Hu, Li Xiao-yan, Jiang Xue-jun, Zheng Xiao-xin, Feng Gao-ke, He Su-yuan, Ren Shan, Yi Xin. Safety of a novel biodegradable stent implanted in the coronary artery in a porcine model [J]. Chinese Journal of Tissue Engineering Research, 2013, 17(38): 6773-6778. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||