Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (15): 2427-2436.doi: 10.3969/j.issn.2095-4344.0250
Previous Articles Next Articles
Meta-analysis of risk factors of the surgical site infection through lumbar posterior approach
Zhong De-gui1, Liu Qi-yu2, Mai Xiu-jun2, Wang Wen-hao2, Lai Jun-hui1, Huang Yong-ming2, Huang Yong-quan2, Hou Qiu-ke2, Su Hai-tao2
- 1Second Clinical Medical School of Guangzhou University of Chinese Medicine, Guangzhou 510006, Guangdong Province, China; 2Guangdong Provincial Hospital of Traditional Chinese Medicine, Guangzhou 510120, Guangdong Province, China
-
Online:2018-05-28Published:2018-05-28 -
Contact:Su Hai-tao, Master, Chief physician, Guangdong Provincial Hospital of Traditional Chinese Medicine, Guangzhou 510120, Guangdong Province, China -
About author:Zhong De-gui, Master, Second Clinical Medical School of Guangzhou University of Chinese Medicine, Guangzhou 510006, Guangdong Province, China -
Supported by:the China Postdoctoral Science Fund Project, No. 2017M612641
CLC Number:
Cite this article
Zhong De-gui, Liu Qi-yu, Mai Xiu-jun, Wang Wen-hao, Lai Jun-hui, Huang Yong-ming, Huang Yong-quan, Hou Qiu-ke, Su Hai-tao . Meta-analysis of risk factors of the surgical site infection through lumbar posterior approach[J]. Chinese Journal of Tissue Engineering Research, 2018, 22(15): 2427-2436.
share this article

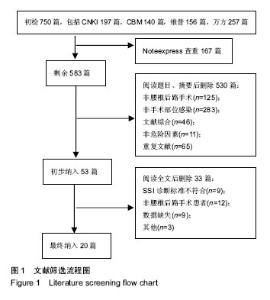
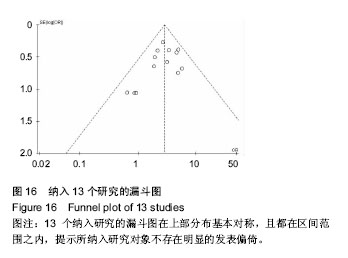
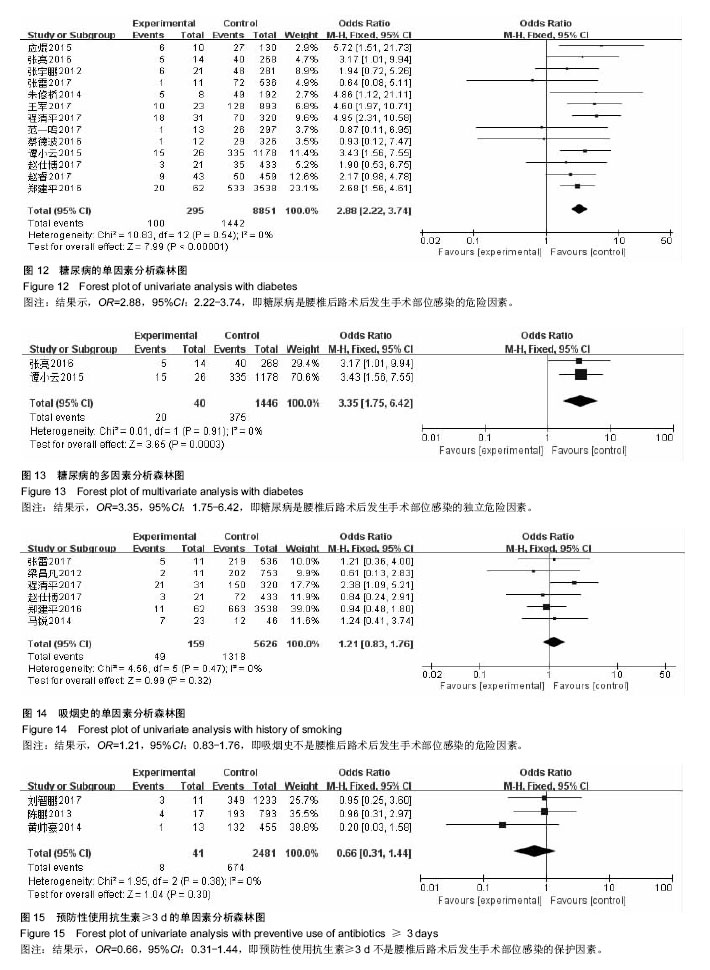
纳入研究包括3个回顾性队列研究[12,18,23],17个病例对照研究[4-11,13-17,19-22],其中观察组423例,对照组139 95例,NOS评分最高8分,最低5分。纳入研究基本特征与风险偏倚见表1。 2.2 Meta分析结果 2.2.1 体质量指数≥27 kg/m2 单因素分析中,以体质量指数≥27 kg/m2作为观察指标,共计纳入3个研究[5,11,22],采用固定效应模型进行Meta分析,结果显示:体质量指 数≥27 kg/m2是腰椎后路术后发生SSI的危险因素[OR=3.82,95%CI(2.47,5.91),P < 0.000 01](图2)。多因素分析中,共计纳入2个研究[11,22],采用固定效应模型将进行Meta分析,结果显示:体质量指数≥27 kg/m2也是腰椎后路术后发生SSI的独立危险因素[OR=3.21,95%CI (1.97,5.22),P < 0.000 01](图3)。"
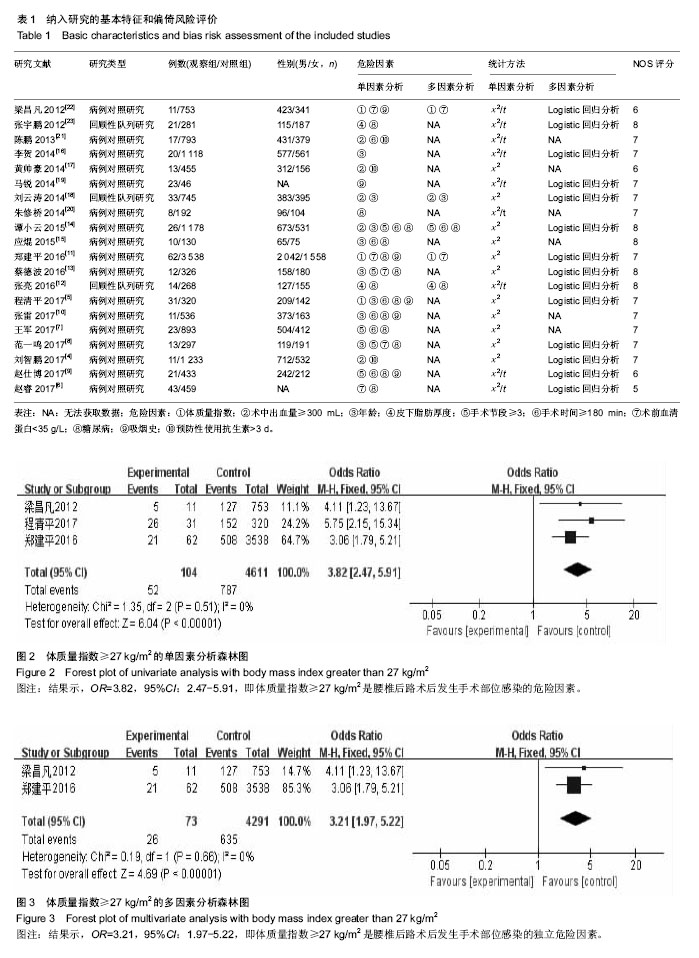

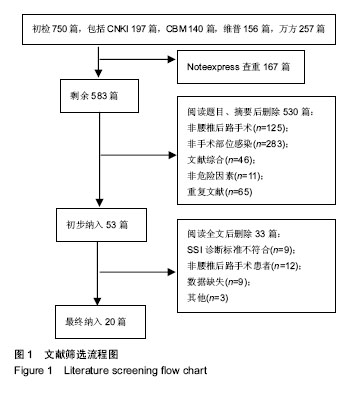
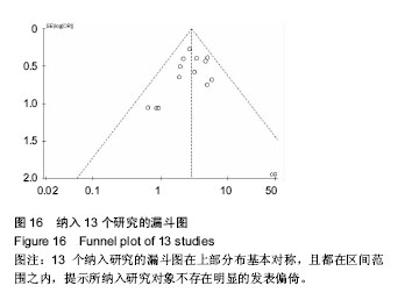
2.2.2 年龄≥60岁 单因素分析中,以年龄≥60岁作为观察指标,共计纳入8个研究[5,8,10,13-16,18],采用固定效应模型进行Meta分析,结果显示:年龄≥60岁是腰椎后路术后发生SSI的危险因素[OR=1.99,95%CI(1.44,2.76),P < 0.000 1](图4);多因素分析中只纳入了1个研究[18]。 2.2.3 术中出血量≥300 mL 单因素分析中,以术中出血量≥300 mL作为观察指标,共计纳入5个研究[4,14,17-18,21],采用固定效应模型进行Meta分析,结果显示:术中出血量≥300 mL是腰椎后路术后发生SSI的危险因素[OR=3.98,95%CI(2.50,6.33),P < 0.000 01](图5);多因素分析中只纳入了1个研究[18]。 2.2.4 皮下脂肪厚度 以皮下脂肪厚度作为观察指标时,单因素分析和多因素分析中,均纳入2个研究[12,23],采用随机效应模型进行Meta分析,结果显示:皮下脂肪厚度与腰椎后路术后发生SSI有显著相关性[MD=5.35,95%CI (3.58,7.12),P < 0.000 01](图6)。 2.2.5 手术节段≥3 单因素分析中,以腰椎手术节段≥3作为观察指标,共计纳入5个研究[7-9,13-14],采用随机效应模型进行Meta分析,结果显示:腰椎手术节段≥3是腰椎后路术后发生SSI的危险因素[OR=3.83,95%CI(2.02,7.26),P < 0.000 1](图7)。多因素分析中,共计纳入2个研究[8,14],采用随机效应模型将进行Meta分析,结果显示:腰椎手术节段≥3不是腰椎后路术后发生SSI的独立危险因素[OR=4.93,95%CI(1.03,23.47),P=0.05] (图8)。 2.2.6 手术时间≥180 min 单因素分析中,以术中手术时间≥180 min作为观察指标,共计纳入7个研 究[5,7, 9-10,14-15,21],采用固定效应模型进行Meta分析,结果显示:手术时间≥180 min是腰椎后路术后发生SSI的危险因素[OR=2.96,95%CI(2.06,4.27),P < 0.000 01] (图9);多因素分析中只纳入了1个研究[14]。 2.2.7 术前血清蛋白< 35 g/L 单因素分析中,以术前血清蛋白<35 g/L作为观察指标,共计纳入5个研究[6,8,11, 13,22],采用固定效应模型进行Meta分析,结果显示:术前血清蛋 白< 35 g/L是腰椎后路术后发生SSI的危险因素[OR=2.37,95%CI(1.63,3.46),P < 0.000 01](图10)。 多因素分析中,共计纳入2个研究[11,22],采用固定效应模型将进行Meta分析,结果显示:术前血清蛋白< 35 g/L也是腰椎后路术后发生SSI的独立危险因素[OR=3.73,95%CI(2.30,6.04),P < 0.000 01] (图11)。 "
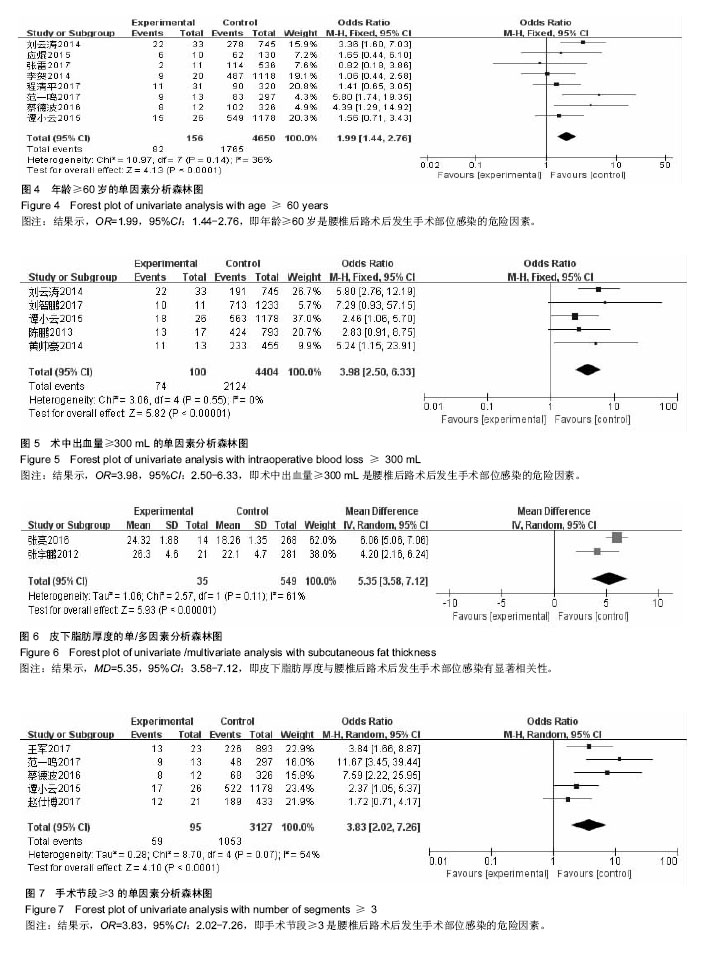

2.2.8 糖尿病 单因素分析中,以糖尿病病史作为观察指标,共计纳入13个研究[5-15,20,23],采用固定效应模型进行Meta分析,结果显示:糖尿病病史是腰椎后路术后发生SSI的危险因素[OR=2.88,95%CI(2.22,3.74),P < 0.000 01] (图12);多因素分析中,共计纳入2个研究[12,14],采用固定效应模型将进行Meta分析,结果显示:糖尿病病史也是腰椎后路术后发生SSI的独立危险因素[OR=3.35,95%CI (1.75,6.42),P=0.003](图13)。 2.2.9 吸烟史 单因素分析中,以长期吸烟史作为观察指标,共计纳入6个研究[5,9-11,19,22],采用固定效应模型进行Meta分析,结果显示,长期吸烟史不是腰椎后路术后发生SSI的危险因素[OR=1.21,95%CI(0.83,1.76),P=0.32] (图14)。 2.2.10 预防性使用抗生素≥3 d 单因素分析中,以预防性使用抗生素≥3 d作为观察指标,共计纳入3个研究[4,17,21],采用固定效应模型进行Meta分析,结果显示:预防性使用抗生素≥3 d不是腰椎后路术后发生SSI的保护因素[OR=0.66,95%CI(0.31,1.44),P=0.30](图15)。"
| [1] Ogihara S, Yamazaki T, Maruyama T, et al. Prospective multicenter surveillance and risk factor analysis of deep surgical site infection after posterior thoracic and/or lumbar spinal surgery in adults. J Orthop Sci. 2015;20(1):71-77.[2] Meredith DS, Kepler CK, Huang RC, et al. Postoperative infections of the lumbar spine: presentation and management. Int Orthop. 2012;36(2):439-444.[3] 中华人民共和国卫生部.医院感染诊断标准(试行)[J]. 中华医学杂志, 2001,81(5):61-67.[4] 刘智鹏,张伟. 腰椎管狭窄症椎弓根内固定术后深部感染的因素分析及处理措施[J]. 河北医学, 2017,23(10):1642-1646.[5] 程清平,王东福,焦朋,等. 腰椎间盘突出症术后椎间隙感染的治疗及危险因素分析[J]. 中国骨与关节损伤杂志, 2017,32(1): 32-35.[6] 赵睿,王锋,赵晓东,等. 高龄患者PLIF术后感染的危险因素分析[J]. 中国社区医师, 2017,33(34):87-88.[7] 王军,郜顺兴,刘晓慧,等. 腰椎后路手术后早期感染危险因素分析[J]. 航空航天医学杂志, 2017,28(11):1330-1332.[8] 范一鸣,王征,王岩. 腰椎后路内固定术后早期切口深部感染的相关因素分析[J]. 颈腰痛杂志, 2017,38(4):327-330.[9] 赵仕博. 胸腰椎后路手术术后切口感染的危险因素分析[D]. 新疆医科大学, 2017.[10] 张雷,田永昊,刘新宇,等. 腰椎后路微创髓核摘除术后切口感染的风险因素分析[J]. 临床骨科杂志,2017,20(4):419-423.[11] 郑建平,郑琦. 腰椎间盘突出症患者术后椎间隙感染的危险因素分析与预防[J].中华医院感染学杂志,2016,26(9): 2076-2078.[12] 张亮,王文俊,巢玉柳,等. 皮下脂肪厚度对腰椎后路术后发生手术部位感染的影响[J]. 河北医药,2016,38(20):3107-3109.[13] 蔡德波.腰椎后路内固定术后早期深部感染的危险因素分析[D]. 广西医科大学,2016.[14] 谭小云,蒲涛,刘季鲁,等. 腰椎融合内固定术后切口感染危险因素分析[J]. 中华临床感染病杂志,2015,8(5):451-453.[15] 应焜. 腰椎后路减压融合内固定术术后感染及危险因素分析[D]. 浙江大学, 2015.[16] 李贺,王宸,吴小涛,等. 腰椎后路椎间融合术后伤口感染的相关因素分析[J]. 江苏医药,2014,40(7):794-796.[17] 黄帅豪,柯雨洪,王义生,等. 腰椎后路内固定术后感染的原因分析与治疗体会[J].中国矫形外科杂志, 2014,22(21):2002-2005.[18] 刘云涛. 手术台次是否是腰椎手术术后切口感染的危险因素[D]. 新疆医科大学,2014.[19] 马锐. 腰椎管狭窄症手术部位感染相关危险因素Logistic回归分析[D]. 新疆医科大学,2014.[20] 朱修桥,郭景东,吕慧,等. 颈椎病与腰椎管狭窄症术后感染的危险因素分析[J]. 中华医院感染学杂志,2014,24(17):4319-4321.[21] 陈鹏,陈刚,朱国兴. 腰椎术后感染的原因分析与治疗策略[J]. 临床骨科杂志,2013,16(5):506-509.[22] [梁昌凡,徐应林,张贤锋. 腰椎间盘突出症术后椎间隙感染的原因分析及预防措施[J]. 中国医学创新,2012,9(31):6-8.[23] 张宇鹏,王晓晶,李利,等. 皮下脂肪厚度对腰椎术后感染的影响[J]. 感染、炎症、修复, 2012,13(4):219-222.[24] Chen SH, Lee CH, Huang KC, et al. Postoperative wound infection after posterior spinal instrumentation: analysis of long-term treatment outcomes. Eur Spine J. 2015;24(3): 561-570.[25] DeSanto J, Ross JS. Spine infection/inflammation. Radiol Clin North Am. 2011;49(1):105-127.[26] Schuster JM, Rechtine G, Norvell DC, et al. The influence of perioperative risk factors and therapeutic interventions on infection rates after spine surgery: a systematic review. Spine (Phila Pa 1976). 2010;35(9 Suppl):S125-S137.[27] D'Agostino C, Scorzolini L, Massetti AP, et al. A seven-year prospective study on spondylodiscitis: epidemiological and microbiological features. Infection. 2010;38(2):102-107.[28] Cronquist AB, Jakob K, Lai L, et al. Relationship between skin microbial counts and surgical site infection after neurosurgery. Clin Infect Dis. 2001;33(8):1302-1308.[29] Cronquist AB, Jakob K, Lai L, et al. Relationship between skin microbial counts and surgical site infection after neurosurgery. Clin Infect Dis. 2001;33(8):1302-1308.[30] Vaidya R, Carp J, Bartol S, et al. Lumbar spine fusion in obese and morbidly obese patients. Spine (Phila Pa 1976). 2009;34(5):495-500.[31] Ho C, Sucato DJ, Richards BS. Risk factors for the development of delayed infections following posterior spinal fusion and instrumentation in adolescent idiopathic scoliosis patients. Spine (Phila Pa 1976). 2007;32(20):2272-2277.[32] Pull TGA, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine (Phila Pa 1976).2009;34(13):1422-1428. [33] Klein JD, Hey LA, Yu CS, et al. Perioperative nutrition and postoperative complications in patients undergoing spinal surgery. Spine (Phila Pa 1976). 1996;21(22):2676-2682.[34] Govender S. Spinal infections. J Bone Joint Surg Br. 2005; 87(11):1454-1458.[35] Chen KW, Yang HL, Lu J, et al. Risk factors for postoperative wound infections of sacral chordoma after surgical excision. J Spinal Disord Tech. 2011;24(4):230-234.[36] Schuster JM, Rechtine G, Norvell DC, et al. The influence of perioperative risk factors and therapeutic interventions on infection rates after spine surgery: a systematic review. Spine (Phila Pa 1976). 2010;35(9 Suppl):S125-S137.[37] Chen S, Anderson MV, Cheng WK, et al. Diabetes associated with increased surgical site infections in spinal arthrodesis. Clin Orthop Relat Res. 2009;467(7):1670-1673.[38] Chen KW, Yang HL, Lu J, et al. Risk factors for postoperative wound infections of sacral chordoma after surgical excision. J Spinal Disord Tech. 2011;24(4):230-234.[39] Olsen MA, Nepple JJ, Riew KD, et al. Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am. 2008;90(1):62-69.[40] Milstone AM, Maragakis LL, Townsend T, et al. Timing of preoperative antibiotic prophylaxis: a modifiable risk factor for deep surgical site infections after pediatric spinal fusion. Pediatr Infect Dis J. 2008;27(8):704-708.[41] Pull TGA, van Laarhoven CJ, Cohen DB. Incidence of surgical site infection following adult spinal deformity surgery: an analysis of patient risk. Eur Spine J. 2010;19(6):982-988.[42] Hegde V, Meredith DS, Kepler CK, et al. Management of postoperative spinal infections[J]. World J Orthop. 2012;3(11): 182-189.[43] Meredith DS, Kepler CK, Huang RC, et al. Postoperative infections of the lumbar spine: presentation and management. Int Orthop.2012;36(2):439-444.[44] 关炳瑜,阿海,贺元,等. 脊柱外科术后感染的影响因素分析[J]. 临床骨科杂志,2016,19(5):547-549. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [3] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [4] | Zhang Chao, Lü Xin. Heterotopic ossification after acetabular fracture fixation: risk factors, prevention and treatment progress [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1434-1439. |
| [5] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [6] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [7] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [8] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [9] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [10] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [11] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [12] | Song Chengjie, Chang Hengrui, Shi Mingxin, Meng Xianzhong. Research progress in biomechanical stability of lateral lumbar interbody fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 923-928. |
| [13] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [14] | Li Yan, Wang Pei, Deng Donghuan, Yan Wei, Li Lei, Jiang Hongjiang. Electroacupuncture for pain control after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 957-963. |
| [15] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||