Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (12): 1895-1901.doi: 10.3969/j.issn.2095-4344.0208
Previous Articles Next Articles
Portal vein arterialization for acute hepatic failure in rats
Chen Peng, Jiang Yi, Zhang Xiao-jin
- Department of Hepatobiliary Surgery, Fuzhou General Hospital of Nanjing Military Command, Fuzhou 350025, Fujian Province, China
-
Received:2017-11-12Online:2018-04-28Published:2018-04-28 -
Contact:Jiang Yi, Chief physician, Department of Hepatobiliary Surgery, Fuzhou General Hospital of Nanjing Military Command, Fuzhou 350025, Fujian Province, China -
About author:Chen Peng, Department of Hepatobiliary Surgery, Fuzhou General Hospital of Nanjing Military Command, Fuzhou 350025, Fujian Province, China
CLC Number:
Cite this article
Chen Peng, Jiang Yi, Zhang Xiao-jin. Portal vein arterialization for acute hepatic failure in rats[J]. Chinese Journal of Tissue Engineering Research, 2018, 22(12): 1895-1901.
share this article

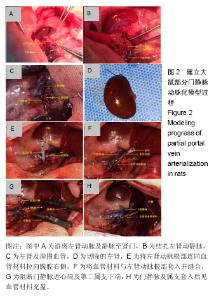
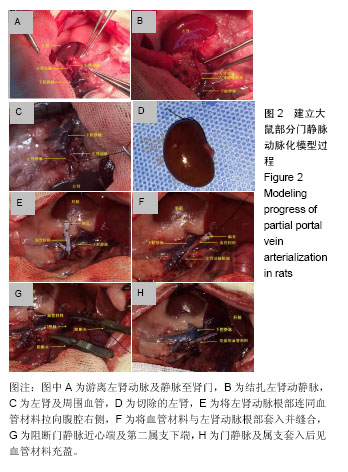
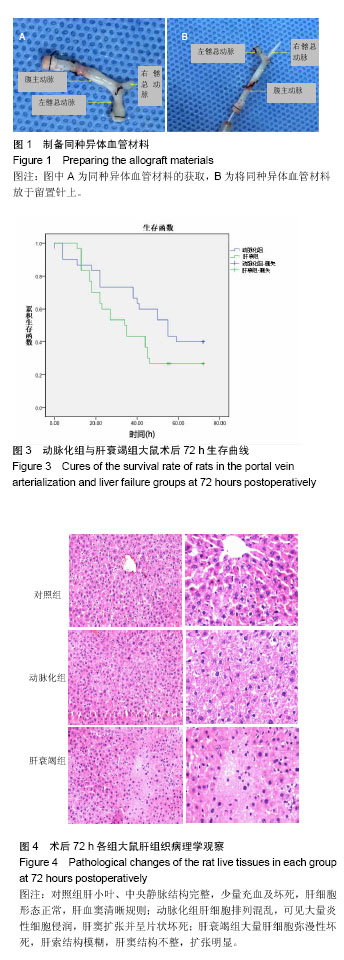
2.1 各组大鼠手术时间和门静脉阻断时间 动脉化组平均手术时间为(55.9±6.6) min,肝衰竭组平均手术时间为(32.5±2.8) min,对照组平均手术时间为(35.0±3.7) min;动脉化组门静脉阻断时间为(16.7±1.9) min,肝衰竭组和对照组门静脉阻断时间为(16±0) min。 2.2 各组大鼠术后一般情况 对照组大鼠活动自如,毛发正常,进食良好,对声音刺激反应正常。动脉化组和肝衰竭组造模后18 h开始出现精神萎靡,抓取时无反应,身体蜷缩,食欲不振,毛发粗糙不整,颜色变深,嗜睡,痛觉反应迟钝或消失,尿黄,少尿,全身皮毛被汗液浸湿;部分大鼠出现神经兴奋症状,全身抽搐,个别大鼠有呕吐症状。 2.3 各组大鼠生存情况 动脉化组大多数死亡时间发生在建模后72 h内,死亡9只,存活率为70%,术中死亡1只,手术操作过程中因游离门静脉至肝总动脉损伤导致大鼠失血死亡,余8只为术后死亡。肝衰竭联合左肾切除组72 h内死亡14只,存活率为53%,全部为术后死亡。对照组72 h生存"
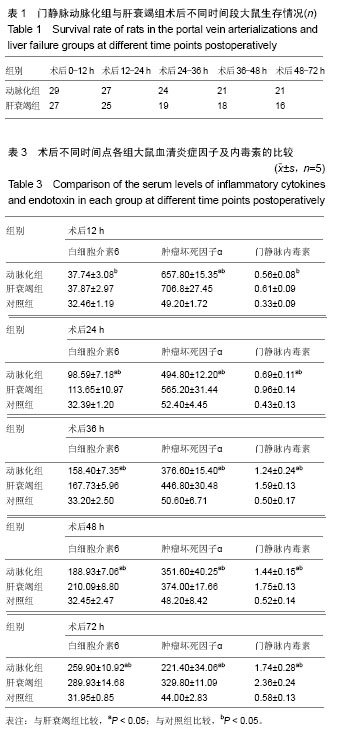

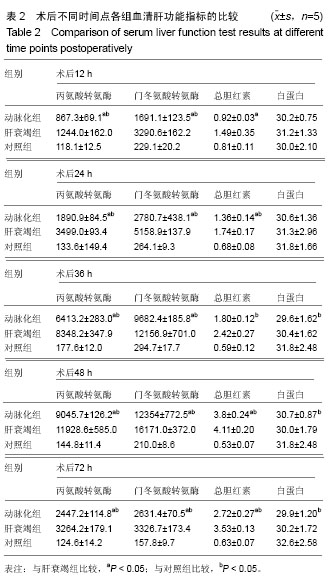
央静脉。动脉化组剖腹探查腹腔无明显积液,同种异体套管通畅在位,大体见肝脏体积稍增大,颜色较肝衰组红润,质地较脆,表面见大量瘀点;病理观察示肝细胞排列混乱,可见大量炎性细胞侵润,肝窦扩张出血并呈片状坏死,病变较肝衰竭组稍轻。 2.5 各组大鼠血清肝功能指标检测结果 对照组各时间点门冬氨酸转氨酶、丙氨酸转氨酶指标高于大鼠正常参考值,低于动脉化组和肝衰组(P < 0.05);动脉化组和肝衰竭组丙氨酸转氨酶、门冬氨酸转氨酶、总胆红素在术后12 h已开始升高,48 h达到峰值,然后开始下降,动脉化组术后各个时间点的丙氨酸转氨酶、门冬氨酸转氨酶都明显低于肝衰竭组(P < 0.05),两组不同时间点的总胆红素比较差异有显著性意义(P < 0.05);动脉化组术后36,48,72 h的白蛋白低于对照组(P < 0.05);与肝衰组比较,动脉化组不同时间点白蛋白与肝衰竭组比较无差异(P > 0.05),见表2。 2.6 各组大鼠血清炎症因子及门静脉内毒素检测结果 见表3。 白细胞介素6:对照组各时间点白细胞介素6水平无明"
| [1] 段钟平,陈煜.肝衰竭诊疗: 进展与展望[J].临床肝胆病杂志, 2012, 28(10):721-725.[2] 中华医学会感染病学分会肝衰竭与人工肝学组,中华医学会肝病学分会重型肝病与人工肝学组.肝衰竭诊治指南[J].中华临床感染病杂志,2012,5(6):321-327.[3] 叶一农,高志良.乙型肝炎肝衰竭发生机制中的三重打击[J].传染病信息,2009,22(5):276-279.[4] 中华医学会肝病学分会重型肝病与人工肝学组,中华医学会感染病学分会肝衰竭与人工肝学组.肝衰竭诊疗指南[J].中华肝脏病杂志, 2006,14(9):643-646.[5] Mabuchi A,Mullaney I,Sheard P,et al.Role of hepatic stellate cells in the early phase of liver regeneration in rat: formation of tight adhesion to parenchymal cells.Comp Hepatol.2004;3 Suppl 1:S29.[6] Cohn R,Herrod C.Some effects upon the liver of complete arterialization of its blood supply. Surgery.1952;32(2):214.[7] Fisher B,Russ C,Updegraff H.A suitable technique for total arterialization of the dog liver.Surgery.Surgery. 1954;35(6): 879-884.[8] Schleimer K,Stippel DL,Kasper HU,et al.Improved microcirculation of a liver graft by controlled portal vein arterialization.J Surg Res.2004;116(2):202-210.[9] Margarit C,Bilbao I,Charco R,et al.Auxiliary heterotopic liver transplantation with portal vein arterialization for fulminant hepatic failure.Liver Transpl.2000;6(6):805-809.[10] 刘琦,李坚,关晓东,等.入肝门静脉动脉化加门腔分流术对肝硬化大鼠血流动力学的影响[J].中华普通外科学文献(电子版),2010,4(2):16-19.[11] Schleimer K,Stippel DL,Kasper HU,et al.Auxiliary liver transplantation with flow‐regulated portal vein arterialization offers a successful therapeutic option in acute hepatic failure–investigations in heterotopic auxiliary rat liver transplantation. Transplant Int.2006;19(7): 581-588.[12] 陈永亮,黄晓强,黄志强,等.部分门静脉动脉化对大鼠肝脏血管铸型变化的影[J].中国普通外科杂志,2007,16(3):223-226.[13] Fernández OM,Ríos A,Sánchez A,et al.Pathology findings in a model of auxiliary liver transplantation with portal vein arterialization in pigs.Transplant Proc.2005;37(9):3939-3942.[14] Nardo B,Montalti R,Puviani L,et al.Portal vein oxygen supply through a liver extracorporeal device to treat acute liver failure in Swine induced by subtotal hepatectomy: preliminary data. Transplant Proc.2006;38(4):1190-1192.[15] Nardo B,Tsivian M,Neri F,et al.Extracorporeal portal vein oxygenation improves outcome of acute liver failure in swine. Transplant Proc.2008;40(6):2046-2048. [16] Tsivian M,Neri F,Prezzi D,et al.Portal vein arterialization in hepatobiliary surgery and liver transplantation.Transplantation proceedings.Elsevier.2007;39(6):1877-1878.[17] Schleimer K,Stippel DL,Kasper HU,et al.Portal vein arterialization increases hepatocellular apoptosis and inhibits liver regeneration. J Surg Res.2008;149(2):250-258.[18] Muller V,Ott R,Tannapfel A,et al.Arterialization of the portal vein in liver transplantation: a new microsurgical model in the rat. Transplantation.2001;71(7):977-981.[19] Schleimer K,Stippel DL,Kasper HU,et al.Portal hyperperfusion causes disturbance of microcirculation and increased rate of hepatocellular apoptosis: investigations in heterotopic rat liver transplantation with portal vein arterialization.Transplant Proc. 2006;38(3):725-729.[20] Seifter S,England S.Energy metabolism. In: Arias IM,et al (eds).The liver: biology and pathobiology, 3rd edn.Raven Press, New York,1994:323-364.[21] Bonnet S,Sauvanet A,Bruno O,et al.Long-term survival after portal vein arterialization for portal vein thrombosis in orthotopic liver transplantation.Gastroenterol Clin Biol.2010;34(1):23-28. [22] Pastor CM.Hepatic and splanchnic oxygen consumption during acute hypoxemic hypoxia in anesthetized pigs.Crit Care Med. 2000;28(3):765-773.[23] Stieber AC,Zetti G,Todo S,et al.The spectrum of portal vein thrombosis in liver transplantation.Ann Surg.1991;213(3):199.[24] Fan YD,Praet M,Van Huysse J,et al.Effects of portal vein arterialization on liver regeneration after partial hepatectomy in the rat.Liver Transpl.2002;8(2):146-152.[25] Kruel CRP,de Fraga RS,Dal Molin S,et al.Hepatic reperfusion in rats: a new model with portal arterialization in studying early ischemia-reperfusion injury.Transplant Proc. 2007;39(10): 3015-3018.[26] Schleimer K,Stippel DL,Kasper HU,et al.Improved microcirculation of a liver graft by controlled portal vein arterialization.J Surg Res.2004;116(2):202-210.[27] 陈永亮,黄志强,王迎宾,等.门静脉动脉化对实验性梗阻性黄疸大鼠肝细胞凋亡的影响[J].中华普通外科杂志,2000,15(6):348-351.[28] 吴均政,江艺,张小进,等.一种新的大鼠门静脉动脉化模型[J].中国组织工程研究,2011,15(15):2716-2720.[29] 李兰娟,肖党生,吴仲文,等.急性肝衰竭大鼠肠道菌群和内毒素的动态研究[J].中华肝脏病杂志,2004,12(3):167-169. [30] Takenaka K,Kanematsu T,Fukuzawa K,et al.Can hepatic failure after surgery for hepatocellular carcinoma in cirrhotic patients be prevented? World J Surg.1990;14(1):123-127.[31] Pugh RNH,Murray-Lyon IM,Dawson JL,et al.Transection of the oesophagus for bleeding oesophageal varices.Br J Surg.1973; 60(8):646-649.[32] Van Deventer SJ,Ten Cate JW,Tytgat GN.Intestinal endotoxemia. Clinical significanc. Gastroenterology.1988;94(3):825.[33] 李兰娟,肖党生,吴仲文,等.急性肝衰竭大鼠肠道菌群和内毒素的动态研究[J].中华肝脏病杂志,2004, 12(3):167-169.[34] Steuerwald NM,Foureau DM,Norton HJ,et al.Profiles of serum cytokines in acute drug-induced liver injury and their prognostic significance.PloS One.2013;8(12):e81974.[35] Chastre A,Bélanger M,Beauchesne E,et al.Inflammatory cascades driven by tumor necrosis factor-alpha play a major role in the progression of acute liver failure and its neurological complications.PloS One.2012;7(11):e49670.[36] Schwabe RF,Brenner DA.Mechanisms of liver injury. I. TNF-α-induced liver injury: role of IKK, JNK, and ROS pathways.Am J Physiol Gastrointest Liver Physiol.2006;290(4):G583-589.[37] Lai HS,Lin WH,Lai SL,et al.Interleukin-6 mediates angiotensinogen gene expression during liver regeneration.PloS One.2013;8(7):e67868.[38] Han Y,Runge MS,Brasier AR.Angiotensin II induces interleukin-6 transcription in vascular smooth muscle cells through pleiotropic activation of nuclear factor-κB transcription factors.Circ Res. 1999;84(6):695-703. |
| [1] | Jiang Xin, Qiao Liangwei, Sun Dong, Li Ming, Fang Jun, Qu Qingshan. Expression of long chain non-coding RNA PGM5-AS1 in serum of renal transplant patients and its regulation of human glomerular endothelial cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 741-745. |
| [2] | Zuo Zhenkui, Han Jiarui, Ji Shuling, He Lulu. Pretreatment with ginkgo biloba extract 50 alleviates radiation-induced acute intestinal injury in mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3666-3671. |
| [3] | Liao Yuan, Qu Mengjian, Liu Jing, Zhong Peirui, Zeng Yahua, Wang Ting, Xiao Hao, Li Lan, Liu Danni, Yang Lu, Zhou Jun. Effects of ultrashort wave on inflammatory response in rats with acute lung injury [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(2): 253-257. |
| [4] | Liao Yuan, Qu Mengjian, Liu Jing, Zhong Peirui Zeng Yahua, Wang Ting, Xiao Hao, Li Lan, Liu Danni, Yang Lu, Zhou Jun. Effects of ultrashort wave on inflammatory response in rats with acute lung injury [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(在线): 2-. |
| [5] | Zhao Xin, Shi Xin, Chen Bei, Cao Yanpeng, Chen Yaowu, Liu Xiaoren, He Yusheng, He Liyun, Li Xiying, Liu Jun. Vacuum sealing drainage enhances wound healing by up-regulating collagen type I/III ratio in rats [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(32): 5122-5127. |
| [6] |
Zhong Ping, Cui Xing.
Baicalin protects intestinal mucosal barrier and intervenes acute graft-versus-host disease by regulating autophagy [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(25): 4028-4032. |
| [7] | Li Hongzhang, Yang Kun, Liu Yuwen, Liu Pan, Qiu Bo, Zou Jie. Effect of miR-155 on acute lung injury in burned rats: changes of nuclear factor-kappa B pathway [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(2): 204-208. |
| [8] |
Xu Changbo, Yin Li, Wang Haitao, Zhang Yi .
Debridement antibiotics irrigation and implant retention for the treatment
of acute infection after total knee arthroplasty |
| [9] | Liu Shenggang, Yang Hongzhong, He Baimei. Autologous induced pluripotent stem cell transplantation for acute lung injury in rats [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(9): 1403-1409. |
| [10] | Zhang Deguo, Tan Xueying, Tang Nan, Huang Fei, Shi Guangjun. Human adipose-derived mesenchymal stem cell transplantation via the tail vein for acute liver failure in rats [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(9): 1416-1421. |
| [11] | Feng Yuan, Li Dewei, Yang Junjun. Therapeutic effects of hepatocyte transplantation via two different intrasplenic approaches in acute hepatic failure rats [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(9): 1422-1427. |
| [12] | Ma Qiuhua, Wang Yunwen, Ma Hui, Qi Jie, Zhang Qingtan. Association of polymorphisms of klotho gene with primary osteoporosis in the elderly aging above 60 years old [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(35): 5587-5591. |
| [13] | Han Quan, Xiong Jian, Wang Yanhua, Dang Yu, Zhang Peixun, Fu Zhongguo, Zhang Dianying, Wang Tianbing. Minimally invasive treatment of acute scaphoid fracture with titanium hollow compression screw [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(34): 5413-5417. |
| [14] | Wang Zhen, Zhang Xuejun, Chen Yuqing, Zhang Lei, Zhu Zunmin, Li Yulong, Huang Zhoufeng, Lian Cheng, Shi Mingyue, Zhang Hongsheng, Wang Fuxu, Wen Shupeng, Yang Jing, Zheng Meiqiong, Sun Kai. Allogeneic chimeric antigen receptor T-cell therapy for recurrent chronic myeloid leukemia in lymphoid blast crisis after allogeneic hematopoietic stem cell transplantation: a two-case report and literature review [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(33): 5263-5268. |
| [15] | Pan Lijuan, Wang Rongli. Differentiation of bone marrow mesenchymal stem cells into hepatocytes under induction by interleukin-1 beta combined with hepatocyte growth factor in vitro [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(33): 5328-5333. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||