Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (17): 4508-4516.doi: 10.12307/2026.090
Previous Articles Next Articles
Preventive effect of lipid-lowering drug targets on the risk of osteonecrosis: genetic information analysis based on the FinnGen and GLGC databases
Li Wei1, Chai Jinlian2, Zhang Bochun1, Li Guangzheng3, Liu Xiaochen3, Wei Chuanfu1, Chen Ning3, Luo Di1, 4, Li Gang1, 4, Liang Xuezhen1, 4
- 1First College of Clinical Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China; 2College of Pharmacy, 3College of Traditional Chinese Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China; 4Department of Orthopedic Microsurgery, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250014, Shandong Province, China
-
Received:2025-03-14Accepted:2025-06-06Online:2026-06-18Published:2025-12-04 -
Contact:Liang Xuezhen, MD, Associate professor, Master’s supervisor, First College of Clinical Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China; Department of Orthopedic Microsurgery, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250014, Shandong Province, China -
About author:Li Wei, MS candidate, First College of Clinical Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China -
Supported by:the National Natural Science Foundation of China, Nos. 82205154 (to LXZ) and 82204453 (to LG); Shandong Provincial Natural Science Foundation for the Youth, No. ZR2021QH004(to LXZ); Shandong Provincial Natural Science Foundation, No. ZR2024MH156 (to LXZ)
CLC Number:
Cite this article
Li Wei, Chai Jinlian, Zhang Bochun, Li Guangzheng, Liu Xiaochen, Wei Chuanfu, Chen Ning, Luo Di, Li Gang, Liang Xuezhen. Preventive effect of lipid-lowering drug targets on the risk of osteonecrosis: genetic information analysis based on the FinnGen and GLGC databases[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(17): 4508-4516.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
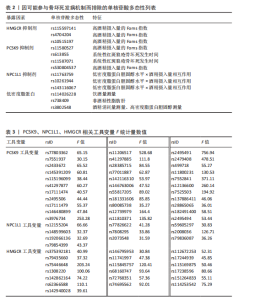
2.1 工具变量 在筛选工具变量时,研究发现部分单核苷酸多态性可能在骨坏死的发病机制中发挥作用。主要包括:高酒精摄入量的Forns指数(rs115597141、rs4704204、rs10515197、rs11580527、rs530804537)、系统性红斑狼疮骨坏死发生时间(rs613855、rs11587071)、低密度脂蛋白胆固醇水平×酒精摄入量相互作用(rs11763759、rs10261944、rs143116067)、饮酒量测量(rs114026228)、非酒精性脂肪肝(rs738409)、酒精消耗量测量、高密度脂蛋白胆固醇测量(rs3802548)。 为保证后续孟德尔随机化分析结果的准确性,这些可能干扰研究结论的单核苷酸多态性被予以排除。具体被排除的单核苷酸多态性详细信息列于表2。 最终筛选的工具变量及其F值见表3。"
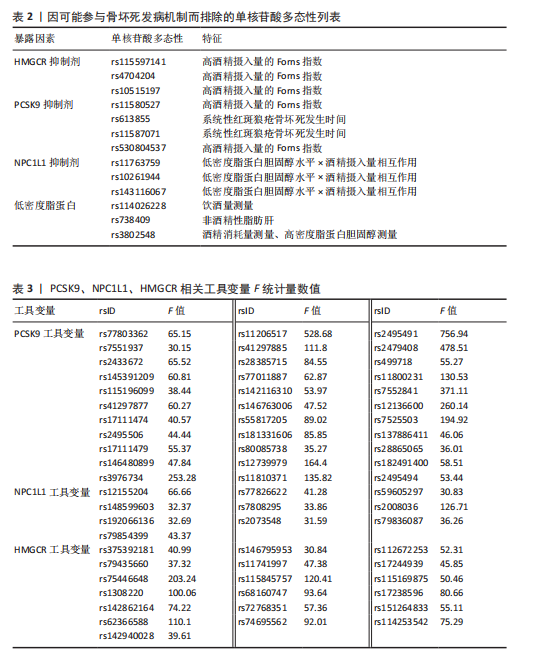

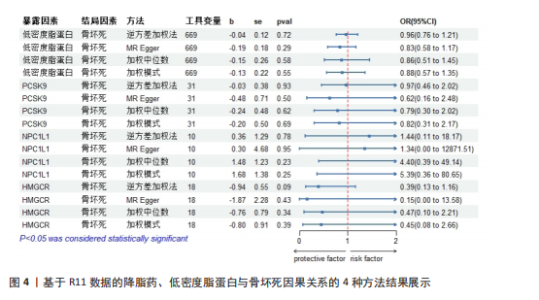
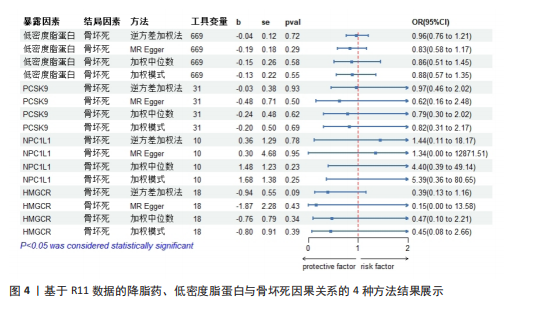
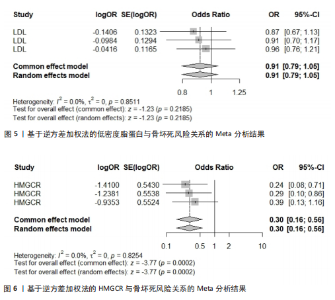
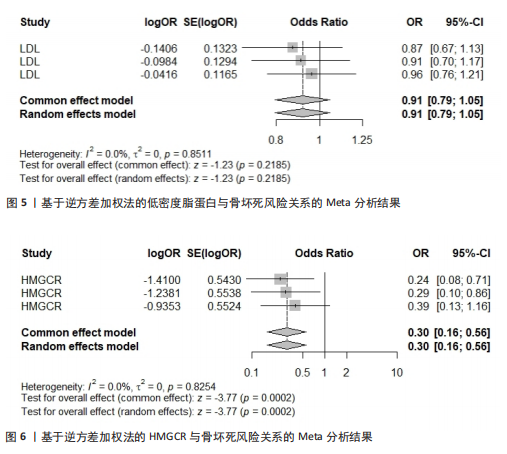
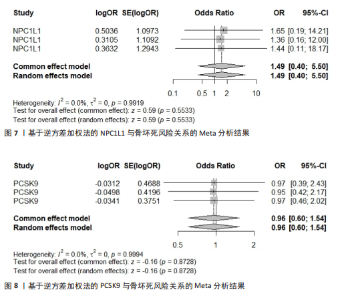
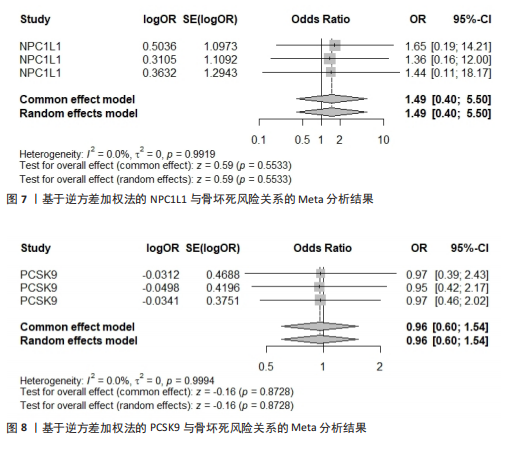
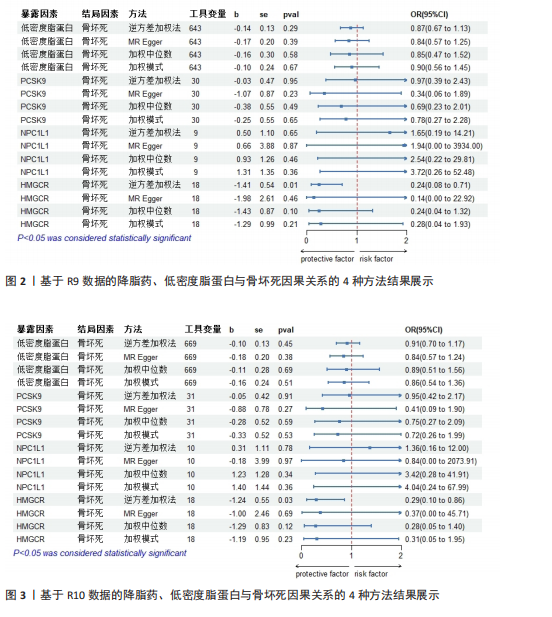
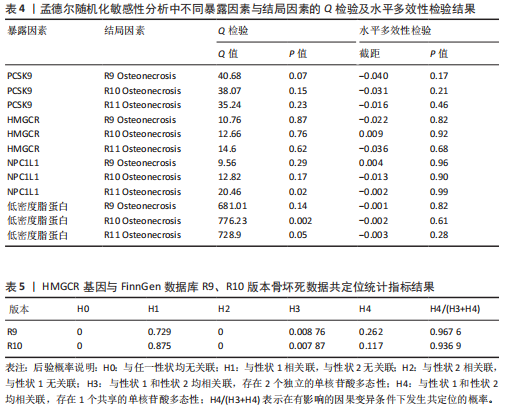
2.2 孟德尔随机化分析结果 在孟德尔随机化分析的初始阶段,研究发现逆方差加权法结果表明:HMGCR抑制与R9版本数据中的骨坏死风险显著降低存在关联(OR=0.24,95%CI:0.08-0.71;P=0.009);HMGCR抑制也与R10版本数据中的骨坏死风险降低相关(OR=0.29,95%CI:0.10-0.86;P=0.025);针对R11版本数据的分析结果显示,HMGCR抑制与骨坏死之间并不存在明显的因果关系(P=0.09 > 0.05),这一结果可能受到数据人群变动以及新纳入人群质量问题等因素的影响。 为了获得更可靠的结论,研究选择了近3个版本的骨坏死数据,并通过Meta分析方法进行整合分析,从而有效避免因人群质量变动等问题对结果产生的干扰。值得注意的是,尽管在采用其余3种分析方法时,并未得出具有统计学显著性的结果,但这些方法所得出的结果方向一致,这种一致性并非毫无意义,它从侧面反映出变量之间可能存在的潜在关联,即便在统计学意义上不显著,也为研究提供了具有价值的线索,提示在更深入的研究或更大样本量的支持下,或许能够揭示出更为明确的关系,为后续研究提供了重要的参考方向。 此外,对R9、R10和R11版本数据的分析表明,NPC1L1抑制、PCSK9抑制以及低密度脂蛋白水平与骨坏死状态之间均未呈现出明显的因果关系,见图2-4。 2.3 Meta分析结果 为了验证研究结果的稳健性,对不同版本中观察到的骨坏死逆方差加权法结果进行了Meta分析。结果显示,HMGCR抑制与疾病风险降低之间存在显著相关性(OR=0.3,95%CI:0.1-0.56,P=0.000 2)且不存在异质性(Heterogeneity:P=0.925 4)。相比之下,其他暴露因素的Meta分析结果未显示出显著性:低密度脂蛋白(OR=0.91,95%CI:0.79-1.05,P=0.218 5)、NPC1L1(OR=1.49,95%CI:0.4-5.5,P=0.553 3)、PCSK9(OR=0.96,95%CI:"
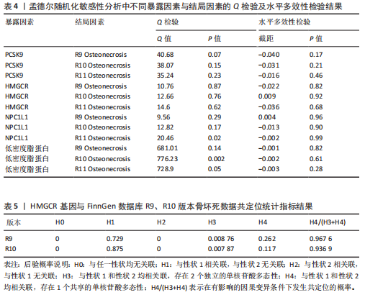
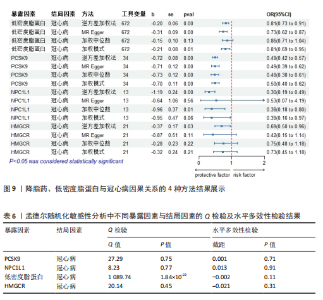
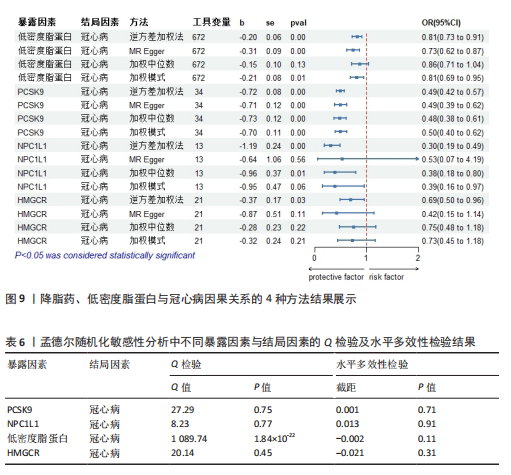
表现稳定,未出现明显的波动或差异。此外,水平多效性检验结果同样显示不存在显著的水平多效性(P > 0.05),这意味着在研究过程中,各研究的效应估计值受未测量混杂因素干扰的可能性较低,研究结果的可靠性和稳定性得到进一步保障。 在确认HMGCR与R9骨坏死之间存在因果关系的前提下,对HMGCR基因区域内低密度脂蛋白与R9骨坏死的共定位后验概率展开了深入分析。结果显示,该后验概率高达96.7%(表5)。 同样,R10骨坏死与HMGCR基因区域内低密度脂蛋白的共定位后验概率为93.7%(表5),这为HMGCR基因与R9骨坏死以及R10骨坏死之间的因果关联提供了更为坚实的支持,结果表明这种因果关联并非偶然,而是具备较高的可信度和稳定性,极大地增强了研究结论的说服力。 2.5 补充分析结果 为了验证工具变量的有效性,研究选择冠心病作为阳性对照组。研究结果表明,针对低密度脂蛋白的所有3种药物靶点和替代基因都与冠心病患病风险的降低有关,见图9和表6。这些阳性对照结果支持了该研究所选暴露工具变量的可靠性,表明这些工具变量可以在随后的孟德尔随机化分析中提供有效的因果推论。"
| [1] PAVELKA K. Osteonecrosis. Baillieres Best Pract Res Clin Rheumatol. 2000;14(2):399-414. [2] HUANG C, QING L, XIAO Y, et al. Insight into Steroid-Induced ONFH: The Molecular Mechanism and Function of Epigenetic Modification in Mesenchymal Stem Cells. Biomolecules. 2023;14(1):4. [3] WANG X, CHEN X, LU L, et al. Alcoholism and Osteoimmunology. Curr Med Chem. 2021;28(9):1815-1828. [4] KUBO Y, DRESCHER W, FRAGOULIS A, et al. Adverse Effects of Oxidative Stress on Bone and Vasculature in Corticosteroid-Associated Osteonecrosis: Potential Role of Nuclear Factor Erythroid 2-Related Factor 2 in Cytoprotection. Antioxid Redox Signal. 2021;35(5):357-376. [5] SHI W, ZHANG X, XU C, et al. Identification of Hub Genes and Pathways Associated with Oxidative Stress of Cartilage in Osteonecrosis of Femoral Head Using Bioinformatics Analysis. Cartilage. 2022;13(1):19476035221074000. [6] CHANG C, GREENSPAN A, GERSHWIN ME. The pathogenesis, diagnosis and clinical manifestations of steroid-induced osteonecrosis. J Autoimmun. 2020;110:102460. [7] BAEK SH, KIM KH, LEE WK, et al. Abnormal Lipid Profiles in Nontraumatic Osteonecrosis of the Femoral Head: A Comparison with Osteoarthritis Using Propensity Score Matching. J Bone Joint Surg Am. 2022; 104(Suppl 2):19-24. [8] LIAO Z, JIN Y, CHU Y, et al. Single-cell transcriptome analysis reveals aberrant stromal cells and heterogeneous endothelial cells in alcohol-induced osteonecrosis of the femoral head. Commun Biol. 2022;5(1):324. [9] HSU SH, JANG MH, TORNG PL, et al. Positive Association Between Small Dense Low-Density Lipoprotein Cholesterol Concentration and Biomarkers of Inflammation, Thrombosis, and Prediabetes in Non-Diabetic Adults. J Atheroscler Thromb. 2019;26(7):624-635. [10] LEUTI A, MACCARRONE M, CHIURCHIÙ V. Proresolving Lipid Mediators: Endogenous Modulators of Oxidative Stress. Oxid Med Cell Longev. 2019;2019:8107265. [11] YANG W, YIN H, WANG Y, et al. New insights into effects of Kaixin Powder on depression via lipid metabolism related adiponectin signaling pathway. Chin Herb Med. 2023; 15(2):240-250. [12] FINCH ER, PAYTON MA, JENKINS DA, et al. Fenofibrate reduces osteonecrosis without affecting antileukemic efficacy in dexamethasone-treated mice. Haematologica. 2021;106(8):2095-2101. [13] KANG P, GAO H, PEI F, et al. Effects of an anticoagulant and a lipid-lowering agent on the prevention of steroid-induced osteonecrosis in rabbits. Int J Exp Pathol. 2010;91(3):235-243. [14] ZHENG H, YE B, HUANG K, et al. Laboratory indices in patients with osteonecrosis of the femoral head: a retrospective comparative study. J Orthop Surg Res. 2023;18(1):750. [15] ZHAO SS, YIU ZZN, BARTON A, et al. Association of Lipid-Lowering Drugs With Risk of Psoriasis: A Mendelian Randomization Study. JAMA Dermatol. 2023;159(3):275-280. [16] BIRNEY E. Mendelian Randomization. Cold Spring Harb Perspect Med. 2022;12(4): a041302. [17] ISTVAN ES. Structural mechanism for statin inhibition of 3-hydroxy-3-methylglutaryl coenzyme A reductase. Am Heart J. 2002; 144(6 Suppl):S27-32. [18] SABATINE MS. PCSK9 inhibitors: clinical evidence and implementation. Nat Rev Cardiol. 2019;16(3):155-165. [19] WILLIAMS DM, FINAN C, SCHMIDT AF, et al. Lipid lowering and Alzheimer disease risk: A mendelian randomization study. Ann Neurol. 2020;87(1):30-39. [20] GRAHAM SE, CLARKE SL, WU KH, et al. The power of genetic diversity in genome-wide association studies of lipids. Nature. 2021;600(7890):675-679. [21] ZUBER V, GRINBERG NF, GILL D, et al. Combining evidence from Mendelian randomization and colocalization: Review and comparison of approaches. Am J Hum Genet. 2022;109(5):767-782. [22] LIN J, ZHOU J, XU Y. Potential drug targets for multiple sclerosis identified through Mendelian randomization analysis. Brain. 2023;146(8):3364-3372. [23] HUANG J, ZHAO X, LI X, et al. HMGCR inhibition stabilizes the glycolytic enzyme PKM2 to support the growth of renal cell carcinoma. PLoS Biol. 2021; 19(4):e3001197. [24] DAY EA, FORD RJ, SMITH BK, et al. Salsalate reduces atherosclerosis through AMPKβ1 in mice. Mol Metab. 2021;53:101321. [25] LI X, SHEN H, ZHANG M, et al. Glycolytic reprogramming in macrophages and MSCs during inflammation. Front Immunol. 2023; 14:1199751. [26] REN Z, ZHOU L. Association of statin use with osteoporosis risk: a drug-targeted Mendelian randomization study. Inflammopharmacology. 2024;32(2):1253-1261. [27] 卿尚兰,徐诣芝.他汀类药物作用于牙槽骨的研究进展[J].检验医学与临床, 2022,19(4):564-566+573. [28] 武扬,李丽.阿托伐他汀对牙周炎大鼠的影响及可能机制[J].长春中医药大学学 报,2023,39(10):1101-1105. [29] WANG XY, MA TL, CHEN KN, et al. Accumulation of LDL/ox-LDL in the necrotic region participates in osteonecrosis of the femoral head: a pathological and in vitro study. Lipids Health Dis. 2021;20(1):167. [30] WANG L, LI S, LUO H, et al. PCSK9 promotes the progression and metastasis of colon cancer cells through regulation of EMT and PI3K/AKT signaling in tumor cells and phenotypic polarization of macrophages. J Exp Clin Cancer Res. 2022;41(1):303. [31] KÖNIGSBRÜGGE O, SCHMALDIENST S, AUINGER M, et al. Antithrombotic agents for primary and secondary prevention of cardiovascular events in patients with end-stage renal disease on chronic hemodialysis. Atherosclerosis. 2020;298:1-6. [32] KIM YU, KEE P, DANILA D, et al. A Critical Role of PCSK9 in Mediating IL-17-Producing T Cell Responses in Hyperlipidemia. Immune Netw. 2019;19(6):e41. [33] PIRILLO A, CATAPANO AL, NORATA GD. Niemann-Pick C1-Like 1 (NPC1L1) Inhibition and Cardiovascular Diseases. Curr Med Chem. 2016;23(10):983-999. [34] TANG Z, JIANG L, PENG J, et al. PCSK9 siRNA suppresses the inflammatory response induced by oxLDL through inhibition of NF-κB activation in THP-1-derived macrophages. Int J Mol Med. 2012;30(4):931-938. [35] FERENCE BA, ROBINSON JG, BROOK RD, et al. Variation in PCSK9 and HMGCR and Risk of Cardiovascular Disease and Diabetes. N Engl J Med. 2016;375(22):2144-2153. [36] CAO K, ZHANG K, MA M, et al. Lactobacillus mediates the expression of NPC1L1, CYP7A1, and ABCG5 genes to regulate cholesterol. Food Sci Nutr. 2021;9(12):6882-6891. [37] ZHANG Z, QIN S, CHEN Y, et al. Inhibition of NPC1L1 disrupts adaptive responses of drug-tolerant persister cells to chemotherapy. EMBO Mol Med. 2022;14(2):e14903. [38] HAYCOCK PC, BURGESS S, WADE KH, et al. Best (but oft-forgotten) practices: the design, analysis, and interpretation of Mendelian randomization studies. Am J Clin Nutr. 2016;103(4):965-978. [39] GILL D, GEORGAKIS MK, WALKER VM, et al. Mendelian randomization for studying the effects of perturbing drug targets. Wellcome Open Res. 2021;6:16. |
| [1] | He Yixiang, Qiao Wanjia, Wang Wenji. Effectiveness and safety of tranexamic acid versus epsilon-aminocaproic acid in total hip and knee arthroplasties: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2361-2369. |
| [2] | Liu Jinlong, Abuduwupuer·Haibier, Bai Zhen, Su Danyang, Miao Xin, Li Fei, Yang Xiaopeng. Efficacy of different nonsurgical treatments for adolescent idiopathic scoliosis: a systematic review and network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2370-2379. |
| [3] | Gao Feng, Zhang Jun, Yu Wenjun, Chanyu Yujing, Zhao Le, Hu Yuting, Wang Junhua, Liu Yongfu. Effects of wrist-hand orthosis on hand dysfunction in stroke patients: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2124-2131. |
| [4] | Wang Zhenze, Liu Fende, Zhang Rui, Li Wujun. Mesenchymal stem cells in treatment of arteriosclerosis obliterans of lower extremities: systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1869-1876. |
| [5] | Guo Ying, Tian Feng, Wang Chunfang. Potential drug targets for the treatment of rheumatoid arthritis: large sample analysis from European databases [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1549-1557. |
| [6] | Wu Zhilin, , He Qin, Wang Pingxi, Shi Xian, Yuan Song, Zhang Jun, Wang Hao . DYRK2: a novel therapeutic target for rheumatoid arthritis combined with osteoporosis based on East Asian and European populations [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1569-1579. |
| [7] | Liu Hongtao, Wu Xin, Jiang Xinyu, Sha Fei, An Qi, Li Gaobiao. Causal relationship between age-related macular degeneration and deep vein thrombosis: analysis based on genome-wide association study data [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1602-1608. |
| [8] | Zheng Yin, Wu Zhenhua, Zhang Cheng, Ruan Kexin, Gang Xiaolin, Ji Hong. Safety and efficacy of immunoadsorption therapy for rheumatoid arthritis: a network meta-analysis and systematic review [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1260-1268. |
| [9] | Chen Qiang, Wu Wenjuan, Jiang Shuhua, Huang Da. Physical exercise improves physical function in burn patients: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1269-1281. |
| [10] | Leng Xiaoxuan, Zhao Yuxin, Liu Xihua. Effects of different neuromodulatory stimulation modalities on non-motor symptoms in Parkinson’s patients: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1282-1293. |
| [11] | Wen Xiaolong, Weng Xiquan, Feng Yao, Cao Wenyan, Liu Yuqian, Wang Haitao. Effects of inflammation on serum hepcidin and iron metabolism related parameters in patients with type 2 diabetes mellitus: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1294-1301. |
| [12] | Gao Zengjie, , Pu Xiang, Li Lailai, Chai Yihui, Huang Hua, Qin Yu. Increased risk of osteoporotic pathological fractures associated with sterol esters: evidence from IEU-GWAS and FinnGen databases [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1302-1310. |
| [13] | Liu Fengzhi, Dong Yuna, Tian Wenyi, Wang Chunlei, Liang Xiaodong, Bao Lin. Gene-predicted associations between 731 immune cell phenotypes and rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1311-1319. |
| [14] | Zhang Cuicui, Chen Huanyu, Yu Qiao, Huang Yuxuan, Yao Gengzhen, Zou Xu. Relationship between plasma proteins and pulmonary arterial hypertension and potential therapeutic targets [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1331-1340. |
| [15] | Jiang Yang, Peng Hao, Song Yanping, Yao Na, Song Yueyu, Yin Xingxiao, Li Yanqi, Chen Qigang. Isometric exercise reduces resting blood pressure: a meta-analysis of moderating factors and dose effects [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 975-986. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||