Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (5): 1302-1310.doi: 10.12307/2026.301
Previous Articles Next Articles
Increased risk of osteoporotic pathological fractures associated with sterol esters: evidence from IEU-GWAS and FinnGen databases
Gao Zengjie1, 2, Pu Xiang1, Li Lailai1, Chai Yihui1, Huang Hua2, Qin Yu2
- 1School of Basic Medical Sciences, Guizhou University of Traditional Chinese Medicine, Guiyang 550024, Guizhou Province, China; 2Department of Orthopedics, Guizhou Hospital of Beijing Jishuitan Hospital, Guiyang 550017, Guizhou Province, China
-
Received:2025-01-17Accepted:2025-04-03Online:2026-02-18Published:2025-06-28 -
Contact:Pu Xiang, Professor, Doctoral supervisor, School of Basic Medical Sciences, Guizhou University of Traditional Chinese Medicine, Guiyang 550024, Guizhou Province, China -
About author:Gao Zengjie, MD candidate, School of Basic Medical Sciences, Guizhou University of Traditional Chinese Medicine, Guiyang 550024, Guizhou Province, China; Department of Orthopedics, Guizhou Hospital of Beijing Jishuitan Hospital, Guiyang 550017, Guizhou Province, China -
Supported by:Science and Technology Fund of Guizhou Provincial Health Commission, No. gzwkj2025-364 (to GZJ); Guizhou Provincial Key Laboratory Project of Miao Medicine, No. [2025]018 (to PX)
CLC Number:
Cite this article
Gao Zengjie, , Pu Xiang, Li Lailai, Chai Yihui, Huang Hua, Qin Yu. Increased risk of osteoporotic pathological fractures associated with sterol esters: evidence from IEU-GWAS and FinnGen databases[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1302-1310.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

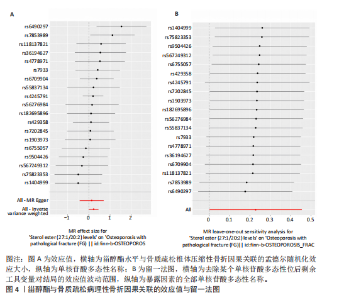
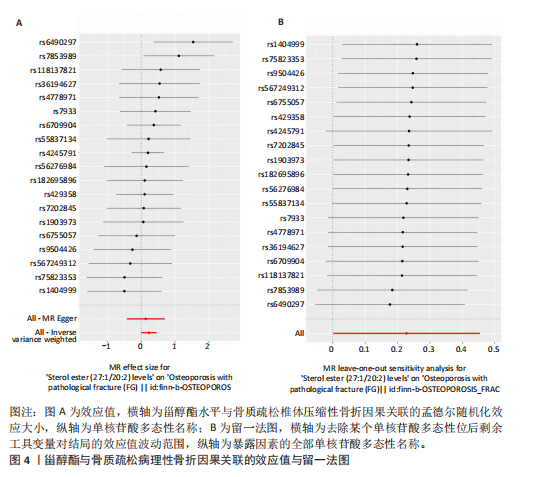
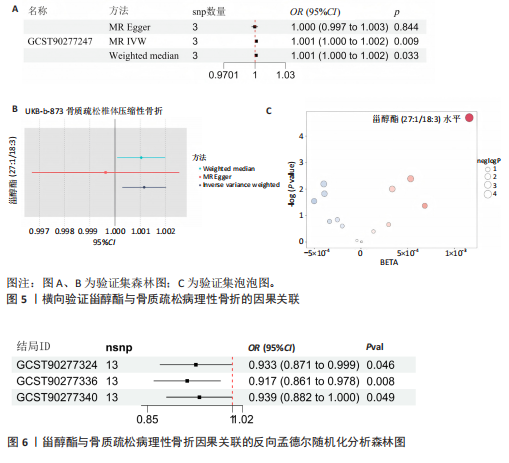
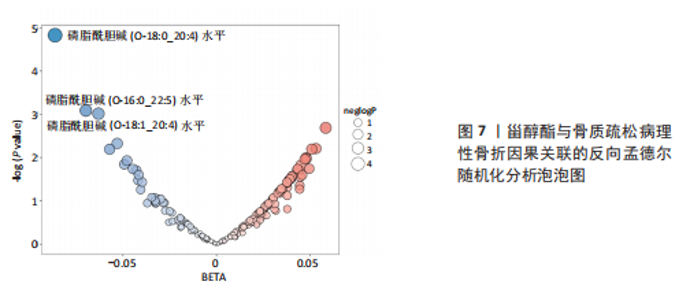
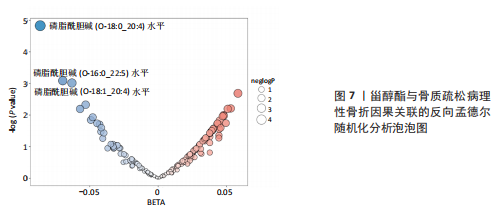
2.1 正向孟德尔随机化分析结果 逆方差加权分析结果显示,甾醇酯(27:1/20:2)水平与骨质疏松病理性骨折存在显著的因果关联(OR=1.256,95%CI:1.001-1.575,P=0.049),甾醇酯(27:1/20:2)水平每增加一个单位,骨质疏松病理性骨折的风险增加约25.55%(即1.256倍),见图2。另外,MR-Egger回归分析结果显示,二酰基甘油(18:1_18:3)、磷脂酰胆碱(O-18:0_16:1)水平与骨质疏松病理性骨折存在显著的因果关联,但逆方差加权分析结果显示磷脂酰胆碱(O-2.1 正向孟德尔随机化分析结果 逆方差加权分析结果显示,甾醇酯(27:1/20:2)水平与骨质疏松病理性骨折存在显著的因果关联(OR=1.256,95%CI:1.001-1.575,P=0.049),甾醇酯(27:1/20:2)水平每增加一个单位,骨质疏松病理性骨折的风险增加约25.55%(即1.256倍),见图2。另外,MR-Egger回归分析结果显示,二酰基甘油(18:1_18:3)、磷脂酰胆碱(O-18:0_16:1)水平与骨质疏松病理性骨折存在显著的因果关联,但逆方差加权分析结果显示磷脂酰胆碱(O-16:1_18:0)水平与骨质疏松病理性骨折不存在显著的因果关联。 2.2 正向孟德尔随机化分析的异质性和多效性 Cochran′s Q检验结果显示,甾醇酯对骨质疏松病理性骨折的工具变量中不存在异质性(P > 0.05)。Steiger检验结果P=0.025,表明工具变量选择符合预期的方向性要求。MR-Egger 检验结果P=0.014,提示不存在多效性。全局检验结果P=0.75,表明各遗传工具变量间不存在显著异质性。MR-PRESSO检验结果P=0.734),表明无显著的水平多效性或离群点干扰。综上所述,此次研究中未发现显著的水平多效性或异质性,提示研究结果稳健可靠。甾醇酯与骨质疏松病理性骨折因果关联的散点图提示研究结果方向一致,见图3A。甾醇酯与骨质疏松病理性骨折因果关联的漏斗图,见图3B。甾醇酯与骨质疏松病理性骨折关联的单核苷酸多态性效应值,见图4A。甾醇酯与骨质疏松病理性骨折因果关联的留一法图,见图4B,提示结果稳健。 更换数据库,以UKB-b-873骨质疏松椎体骨折为结局,设定在全基因组显著性水平(P < 5×10-8)下与脂质代谢物显著相关的单核苷酸多态性进行重复验证,结果显示甾醇酯是骨质疏松压缩性骨折的危险因素(OR=1.001,95%CI:1.000-1.002,P=0.009),甾醇酯每增加1单位,骨质疏松压缩性骨折的发生概率增加约0.116 1%(OR=1.001),见图5。 2.3 反向孟德尔随机化分析结果 反向孟德尔随机化分析结果显示,骨质疏松病理性骨折作为暴露因素与3种磷脂酰胆碱水平存在因果关联。在骨质疏松病理性骨折情况下,磷脂酰胆碱(O-18:0_20:4)、磷脂酰胆碱(O-16:0_22:5)与磷脂酰胆碱(O-18:1_20:4)水平均降低(OR=0.917,95%CI:0.861-0.978,P=0.008;OR=0.933,95%CI:0.871-0.999,P=0.046;OR=0.939,95%CI:0.882-0.999,P=0.049),见图6,7。"

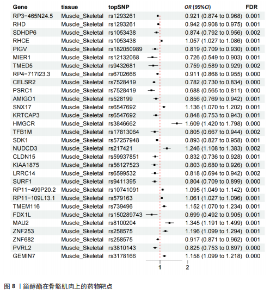
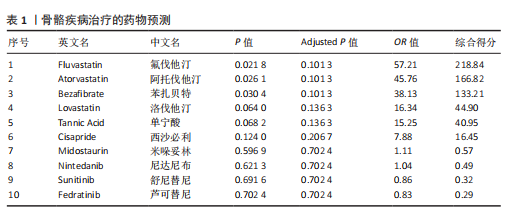
2.4 反向孟德尔随机化分析的异质性及多效性 Cochran′s Q检验结果显示不存在异质性;MR-PRESSO全局测试未发现显著的多效性偏差,表明所选工具变量有效和独立;MR-Egger检验截距P > 0.05,表明Egger截距不显著,没有证据表明存在水平多效性。 2.5 药物靶点分析 此次研究选用甾醇酯作为表型指标,借助SMR和eQTL分析方法,在骨骼肌肉组织中探寻可能影响骨骼系统的药物作用靶点。通过整合遗传学与转录组学数据,旨在揭示甾醇代谢路径中潜在的关键分子机制,为开发新型骨骼疾病治疗药物提供科学依据。药物靶点分析结果如图8所示,最显著的保护性靶点是CELSR2。通过药物数据库IDG Drug Targets 2022进行药物预测,排名前3的是氟伐他汀、阿托伐他汀、苯扎贝特,见表1。"

| [1] SING C, LIN T, BARTHOLOMEW S, et al. Global Epidemiology of Hip Fractures: Secular Trends in Incidence Rate, Post‐Fracture Treatment, and All‐Cause Mortality. J Bone Miner Res. 2023;38(8):1064-1075. [2] GOLD LS, SURI P, O’REILLY MK, et al. Mortality among older adults with osteoporotic vertebral fracture. Osteoporos Int. 2023;34(9):1561-1575. [3] SHAO L, LUO S, ZHAO Z. Lipid metabolites are associated with the risk of osteoporotic fractures. Sci Rep. 2024;14(1):19245. [4] WU M, DU Y, ZHANG C, et al. Mendelian Randomization Study of Lipid Metabolites Reveals Causal Associations with Heel Bone Mineral Density. Nutrients. 2023;15(19): 4160. [5] SFEIR JG, DRAKE MT, KHOSLA S, et al. Skeletal Aging. Mayo Clin Proc. 2022;97(6): 1194-1208. [6] GUO D, ZHAO M, XU W, et al. Dietary interventions for better management of osteoporosis: An overview. Crit Rev Food Sci Nutr. 2021;63(1):125-144. [7] CHE Y, YANG J, TANG F, et al. New Function of Cholesterol Oxidation Products Involved in Osteoporosis Pathogenesis. Int J Mol Sci. 2022;23(4):2020. [8] HUANG CY, CHENG M, WANG PH. The negative correlation between osteoporosis and hyperlipidemia: Is it real? Taiwan J Obstet Gynecol. 2020;59(3):471-472. [9] LARSSON SC, BUTTERWORTH AS, BURGESS S. Mendelian randomization for cardiovascular diseases: principles and applications. Eur Heart J. 2023;44(47): 4913-4924. [10] RICHMOND RC, SMITH GD. Mendelian Randomization: Concepts and Scope. Cold Spring Harb Perspect Med. 2021;12(1): a040501. [11] HUANG J, GUI Y, WU J, et al. Causal effects of socioeconomic traits on frailty: a Mendelian randomization study. Front Med (Lausanne). 2024;11:1344217. [12] PENG B, MENG H, GUO L, et al. Anxiety disorder and cardiovascular disease: a two‐sample Mendelian randomization study. ESC Heart Fail. 2024;11(2):1174-1181. [13] STRAUSZ T, STRAUSZ S, JONES SE, et al. A Two-Sample Mendelian Randomization Study of Neuroticism and Sleep Bruxism. J Dent Res. 2024;103(10):980-987. [14] ZHANG Y, ZHONG Z, TANG Z, et al. Insomnia and sleep duration for kidney function: Mendelian randomization study. Ren Fail. 2024;46(2):2387430. [15] GKATZIONIS A, BURGESS S, NEWCOMBE PJ. Statistical methods for cis‐Mendelian randomization with two‐sample summary‐level data. Genet Epidemiol. 2023;47(1): 3-25. [16] HU X, ZHAO J, LIN Z, et al. Mendelian randomization for causal inference accounting for pleiotropy and sample structure using genome-wide summary statistics. Proc Natl Acad Sci U S A. 2022; 119(28):e2106858119. [17] BURGESS S, SMITH GD, DAVIES NM, et al. Guidelines for performing Mendelian randomization investigations: update for summer 2023. Wellcome Open Res. 2023;4:186. [18] BOWDEN J, SMITH GD, HAYCOCK PC, et al. Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator. Genet Epidemiol. 2016;40(4): 304-314. [19] MACKAY TFC, ANHOLT RRH. Pleiotropy, epistasis and the genetic architecture of quantitative traits. Nat Rev Genet. 2024; 25(9):639-657. [20] BURGESS S, THOMPSON SG. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol. 2017;32(5):377-389. [21] CHERNY SS, FREIDIN MB, WILLIAMS FMK, et al. The analysis of causal relationships between blood lipid levels and BMD. PLoS One. 2019;14(2):e0212464. [22] DEPTA L, WHITMARSH-EVERISS T, LARAIA L. Structure, function and small molecule modulation of intracellular sterol transport proteins. Bioorg Med Chem. 2022;68: 116856. [23] LUO J, YANG H, SONG BL. Mechanisms and regulation of cholesterol homeostasis. Nat Rev Mol Cell Biol. 2019;21(4):225-245. [24] KIM H, OH B, PARK-MIN KH. Regulation of Osteoclast Differentiation and Activity by Lipid Metabolism. Cells. 2021;10(1):89. [25] 李坤.胆固醇在BMSCs成骨分化中的双重作用及机制研究[D].苏州:苏州大学, 2019. [26] DONG B, SINGH AB, FUNG C, et al. CETP inhibitors downregulate hepatic LDL receptor and PCSK9 expression in vitro and in vivo through a SREBP2 dependent mechanism. Atherosclerosis. 2014;235(2):449-462. [27] SAMMONS E, HOPEWELL JC, CHEN F, et al. Long-term safety and efficacy of anacetrapib in patients with atherosclerotic vascular disease. Eur Heart J. 2021;43(14): 1416-1424. [28] LANDRAY MJ. Randomized Evaluation of the Effects of Anacetrapib through Lipid-modification (REVEAL)-A large-scale, randomized, placebo-controlled trial of the clinical effects of anacetrapib among people with established vascular disease: Trial design, recruitment, and baseline characteristics. Am Heart J. 2017;187:182-190. [29] 饶甲环,马煜盛,龙洁旎,等.胆固醇酯转移蛋白抑制剂的研究进展[J].医学研究生学报,2019,32(7):776-779. [30] DORIGHELLO GG, ASSIS LHP, RENTZ T, et al. Novel Role of CETP in Macrophages: Reduction of Mitochondrial Oxidants Production and Modulation of Cell Immune-Metabolic Profile. Antioxidants (Basel). 2022;11(9):1734. [31] GONEN A, MILLER YI. From Inert Storage to Biological Activity—In Search of Identity for Oxidized Cholesteryl Esters. Front Endocrinol (Lausanne). 2020;11:602252. [32] ARABI SM, CHAMBARI M, BAHRAMI LS, et al. The Effect of Statin Therapy on Bone Metabolism Markers and Mineral Density: Aa GRADE-Assessed Systematic Review and Dose-Response Meta-Analysis of Randomized Controlled Trials. Adv Pharm Bull. 2024;14(3):591-603. [33] ZHENG J, BRION M, KEMP JP, et al. The Effect of Plasma Lipids and Lipid-Lowering Interventions on Bone Mineral Density: A Mendelian Randomization Study. J Bone Miner Res. 2020;35(7):1224-1235. [34] KUWAHARA M, AKASAKI Y, GOTO N, et al. Fluvastatin promotes chondrogenic differentiation of adipose-derived mesenchymal stem cells by inducing bone morphogenetic protein 2. BMC Pharmacol Toxicol. 2022;23(1):61. [35] CRISTANCHO AG, LAZAR MA. Forming functional fat: a growing understanding of adipocyte differentiation. Nat Rev Mol Cell Biol. 2011;12(11):722-734. [36] MATSUSHITA Y, ONO W, ONO N. Toward Marrow Adipocytes: Adipogenic Trajectory of the Bone Marrow Stromal Cell Lineage. Front Endocrinol (Lausanne). 2022;13: 882297. [37] LIN Z, HE H, WANG M, et al. MicroRNA-130a controls bone marrow mesenchymal stem cell differentiation towards the osteoblastic and adipogenic fate. Cell Prolif. 2019;52(6): e12688. [38] LU CC, QIN H, ZHANG ZH, et al. The association between keloid and osteoporosis: real-world evidence. BMC Musculoskelet Disord. 2021;22(1):39. [39] CHEN HM, HSU CY, PAN BL, et al. Association of Decreased Bone Density and Hyperlipidemia in a Taiwanese Older Adult Population. J Endocr Soc. 2024;8(5): bvae035. [40] ABBASLOO S, AGHAEI MEYBODI HR, FAHIMFAR N, et al. The associations of statin intake and the trabecular bone score and bone mineral density status in elderly Iranian intdiduals: a cross-sectional analysis of the Bushehr Elderly Health (BEH) program. Arch Osteoporos. 2021;16(1):144. [41] HERNÁNDEZ JL, OLMOS JM, ROMAÑA G, et al. Bone mineral density in statin users: a population-based analysis from a Spanish cohort. J Bone Miner Metab. 2013; 32(2):184-191. [42] LI W, HUANG Z, FANG W, et al. Remnant Cholesterol Variability and Incident Ischemic Stroke in the General Population. Stroke. 2022;53(6):1934-1941. [43] GONEL A, KIRHAN I, KOYUNCU I, et al. The Role of Interferences in the Increasing Incidence of Vitamin D Deficiency. Endocr Metab Immune Disord Drug Targets. 2020; 20(8):1303-1308. [44] LING Y, XU F, XIA X, et al. Vitamin D supplementation reduces the risk of fall in the vitamin D deficient elderly: An updated meta-analysis. Clin Nutr. 2021;40(11):5531-5537. [45] LI L, LIU Y, LIU X, et al. Regulatory roles of external cholesterol in human airway epithelial mitochondrial function through STARD3 signalling. Clin Transl Med. 2022; 12(6):e902. [46] JANG MY, CHUN SI, MUN CW, et al. Evaluation of Metabolomic Changes as a Biomarker of Chondrogenic Differentiation in 3D-cultured Human Mesenchymal Stem Cells Using Proton (1H) Nuclear Magnetic Resonance Spectroscopy. PLoS One. 2013; 8(10):e78325. [47] ZHAI G, RANDELL EW, RAHMAN P. Metabolomics of osteoarthritis: emerging novel markers and their potential clinical utility. Rheumatology. 2018;57(12):2087-2095. [48] YANG CD, CHUANG SC, CHENG TL, et al. An Intermediate Concentration of Calcium with Antioxidant Supplement in Culture Medium Enhances Proliferation and Decreases the Aging of Bone Marrow Mesenchymal Stem Cells. Int J Mol Sci. 2021;22(4):2095. [49] ZHAN J, LUO D, ZHAO B, et al. Polydatin administration attenuates the severe sublesional bone loss in mice with chronic spinal cord injury. Aging. 2022;14(21):8856-8875. [50] SHORE DM, REGGIO PH. The therapeutic potential of orphan GPCRs, GPR35 and GPR55. Front Pharmacol. 2015;6:69. [51] MILLER MR, ABSHIRINI M, WOLBER FM, et al. Greenshell Mussel Products: A Comprehensive Review of Sustainability, Traditional Use, and Efficacy. Sustainability. 2023;15(5):3912. [52] ODOEMELAM CS, HUNTER E, EBERL D, et al. The Role of Phorbol Diesters in Mediating Human Placental Aromatase Cytochrome P450 Activity. Appl Biosci. 2022;1(3):279-288. [53] BOZELLI JC, AZHER S, EPAND RM. Plasmalogens and Chronic Inflammatory Diseases. Front Physiol. 2021;12:730829. [54] DURKOVICOVA Z, FAKTOROVA X, JAKABOVICOVA M, et al. Molecular mechanisms in the pathogenesis of metabolically associated fatty liver disease. Bratisl Lek Listy. 2023;124(6):427-436. [55] WANG Z, WANG X, WANG Y, et al. NanoZnO-modified titanium implants for enhanced anti-bacterial activity, osteogenesis and corrosion resistance. J Nanobiotechnology. 2021;19(1):353. [56] CHAMANI S, LIBERALE L, MOBASHERI L, et al. The role of statins in the differentiation and function of bone cells. Eur J Clin Invest. 2021;51(7):e13534. [57] BAO C, WU T, ZHU S, et al. Regulation of cholesterol homeostasis in osteoporosis mechanisms and therapeutics. Clin Sci (Lond). 2023;137(15):1131-1143. [58] LIN SM, WANG JH, LIANG CC, et al. Statin Use Is Associated With Decreased Osteoporosis and Fracture Risks in Stroke Patients. J Clin Endocrinol Metab. 2018;103(9):3439-3448. [59] DE NEGRI ATANASIO G, FERRARI PF, CAMPARDELLI R, et al. Poly (Lactic-co-Glycolic Acid) Nanoparticles and Nanoliposomes for Protein Delivery in Targeted Therapy: A Comparative In Vitro Study. Polymers (Basel). 2020;12(11):2566. [60] SŁOTA D, PIĘTAK K, JAMPILEK J, et al. Polymeric and Composite Carriers of Protein and Non-Protein Biomolecules for Application in Bone Tissue Engineering. Materials (Basel). 2023;16(6):2235. |
| [1] | Zhang Qian, Huang Dongfeng. Weighted gene co-expression network analysis combined with machine learning to screen and validate biomarkers for osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1096-1105. |
| [2] | Liu Fengzhi, Dong Yuna, Tian Wenyi, Wang Chunlei, Liang Xiaodong, Bao Lin. Gene-predicted associations between 731 immune cell phenotypes and rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1311-1319. |
| [3] | Zhang Cuicui, Chen Huanyu, Yu Qiao, Huang Yuxuan, Yao Gengzhen, Zou Xu. Relationship between plasma proteins and pulmonary arterial hypertension and potential therapeutic targets [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1331-1340. |
| [4] | Zeng Hao, Sun Pengcheng, Chai Yuan, Huang Yourong, Zhang Chi, Zhang Xiaoyun. Association between thyroid function and osteoporosis: genome-wide data analysis of European populations [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1019-1027. |
| [5] | Rong Xiangbin, , Zheng Haibo, Mo Xueshen, Hou Kun, Zeng Ping, . Plasma metabolites, immune cells, and hip osteoarthritis: causal inference based on GWAS data from European populations [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1028-1035. |
| [6] | He Qiwang, , , Chen Bo, Liang Fuchao, Kang Zewei, Zhou Yuan, Ji Anxu, Tang Xialin, . Relationship between Alzheimer’s disease and sarcopenia and body mass index: analysis of GWAS datasets for European populations [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1036-1046. |
| [7] | Ding Yu, Chen Jingwen, Chen Xiuyan, Shi Huimin, Yang Yudie, Zhou Meiqi, Cui Shuai, . Circulating inflammatory proteins and myocardial hypertrophy: large sample analysis of European populations from GWAS Catalog and FinnGen databases [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1047-1057. |
| [8] | Chen Jiayong, Tang Meiling, Lu Jianqi, Pang Yan, Yang Shangbing, Mao Meiling, Luo Wenkuan, Lu Wei, Zhou Jiatan. Based on Mendelian randomization, the causal relationship between 1400 metabolites and sarcopenia and the correlation analysis of cardiovascular disease were investigated [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-11. |
| [9] | Zhang Yibo, Lu Jianqi, Mao Meiling, Pang Yan, Dong Li, Yang Shangbing, Xiao Xiang. Exploring the causal relationship between rheumatoid arthritis and coronary atherosclerosis: a Mendel randomized study involving serum metabolites and inflammatory factors [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-9. |
| [10] | Dong Tingting, Chen Tianxin, Li Yan, Zhang Sheng, Zhang Lei. Causal relationship between modifiable factors and joint sports injuries [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1953-1962. |
| [11] | Chen Shuai, Jin Jie, Han Huawei, Tian Ningsheng, Li Zhiwei . Causal relationship between circulating inflammatory cytokines and bone mineral density based on two-sample Mendelian randomization [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1556-1564. |
| [12] |
Zhao Wensheng, Li Xiaolin, Peng Changhua, Deng Jia, Sheng Hao, Chen Hongwei, Zhang Chaoju, He Chuan.
Gut microbiota and osteoporotic fractures #br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1296-1304.
|
| [13] | Ma Haoyu, Qiao Hongchao, Hao Qianqian, Shi Dongbo. Causal effects of different exercise intensities on the risk of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1305-1311. |
| [14] | Li Jiatong, Jin Yue, Liu Runjia, Song Bowen, Zhu Xiaoqian, Li Nianhu . Association between thyroid function levels and phenotypes associated with sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1312-1320. |
| [15] | Wu Guangtao, Qin Gang, He Kaiyi, Fan Yidong, Li Weicai, Zhu Baogang, Cao Ying . Causal relationship between immune cells and knee osteoarthritis: a two-sample bi-directional Mendelian randomization analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1081-1090. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||