Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (14): 2899-2906.doi: 10.12307/2025.617
Previous Articles Next Articles
Correlation between muscle synergy characteristics of the affected leg and gait stability during walking in patients undergoing anterior cruciate ligament reconstruction
Wei Mengli1, 2, Zhong Yaping1, 2, Yu Tingting1, Tan Xilin1, Cao Sijia1
- 1Sports Big Data Research Center of Wuhan Sports University, Wuhan 430079, Hubei Province, China; 2Hubei Sports and Health Innovation and Development Research Center, Wuhan 430079, Hubei Province, China
-
Received:2024-05-13Accepted:2024-07-06Online:2025-05-18Published:2024-09-27 -
Contact:Zhong Yaping, PhD, Professor, Doctoral supervisor, Sports Big Data Research Center of Wuhan Sports University, Wuhan 430079, Hubei Province, China;Hubei Sports and Health Innovation and Development Research Center, Wuhan 430079, Hubei Province, China -
About author:Wei Mengli, PhD candidate, Sports Big Data Research Center of Wuhan Sports University, Wuhan 430079, Hubei Province, China; Hubei Sports and Health Innovation and Development Research Center, Wuhan 430079, Hubei Province, China -
Supported by:Late-stage Key Project of the National Social Science Foundation of China, No. 22FTYA001 (to ZYP); Decision-making Consultation Research Project of General Administration of Sport of China, No. 2023-B-19 (to ZYP); Hubei Provincial Higher Education Reform Project, No. 2022395 (to ZYP)
CLC Number:
Cite this article
Wei Mengli, Zhong Yaping, Yu Tingting, Tan Xilin, Cao Sijia. Correlation between muscle synergy characteristics of the affected leg and gait stability during walking in patients undergoing anterior cruciate ligament reconstruction[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(14): 2899-2906.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
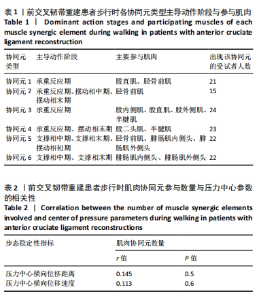
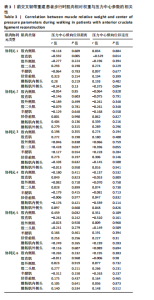
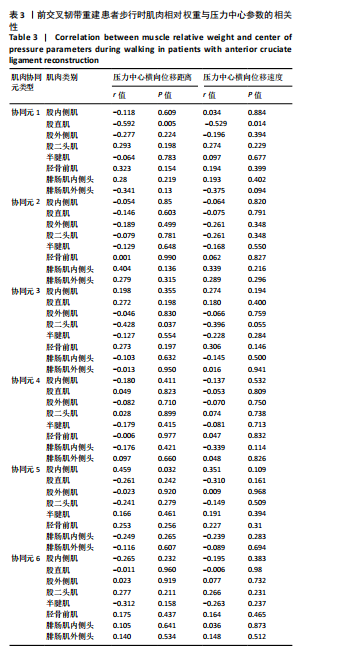
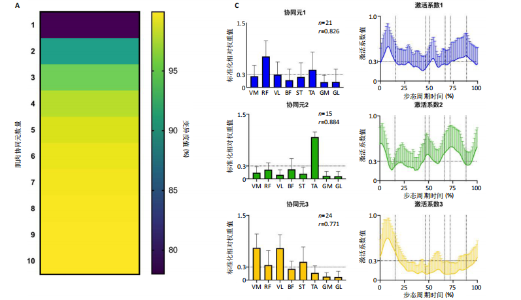
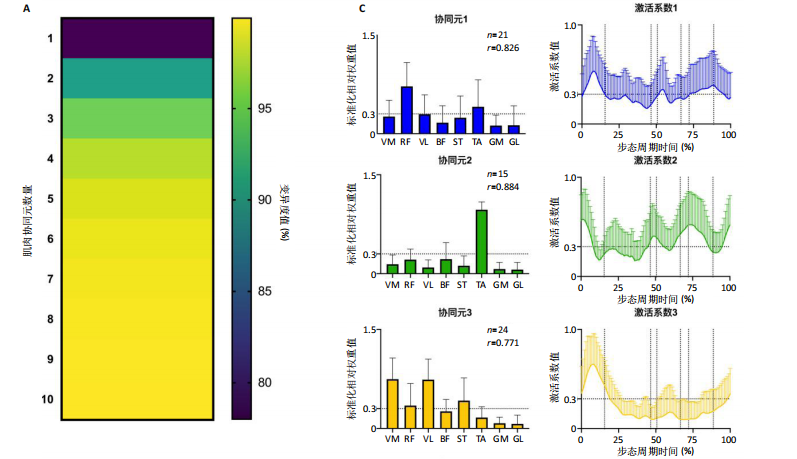
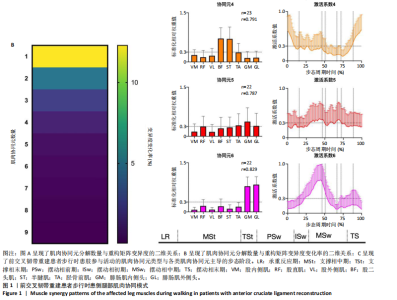
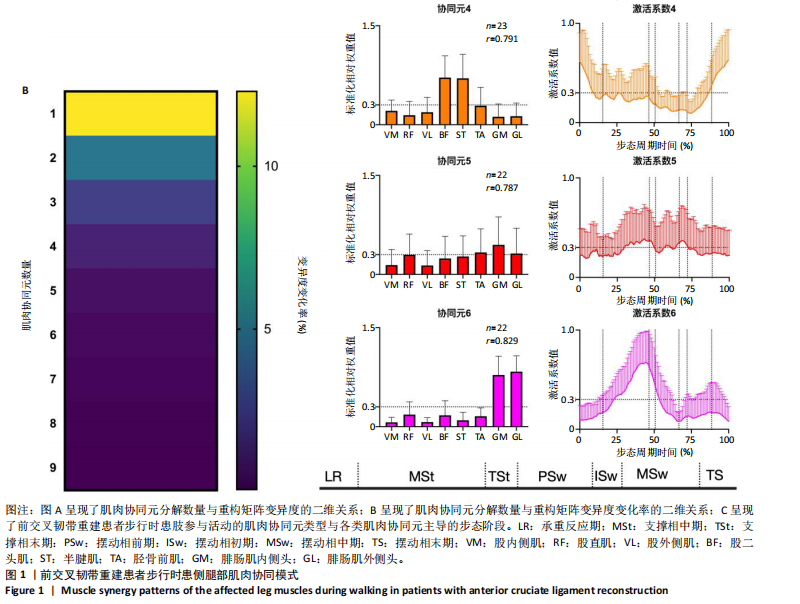
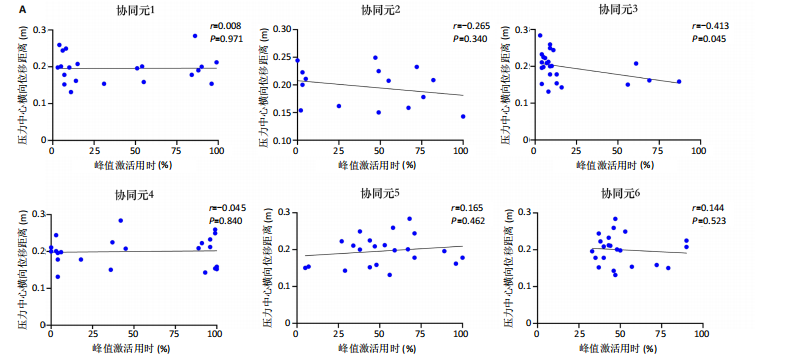
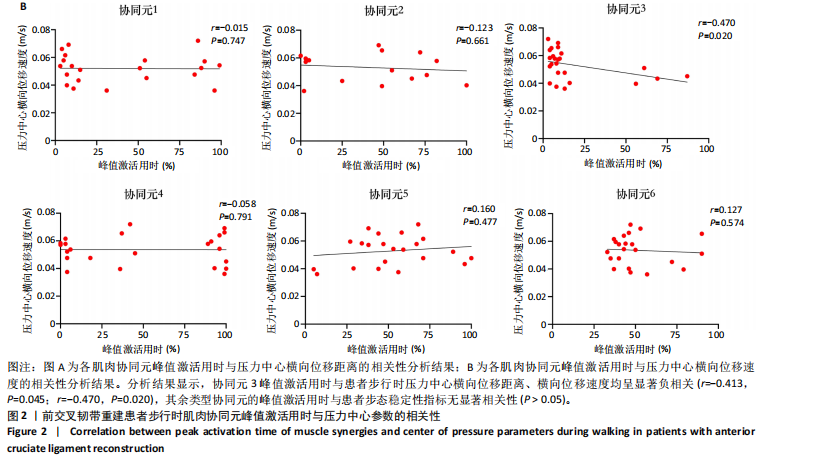
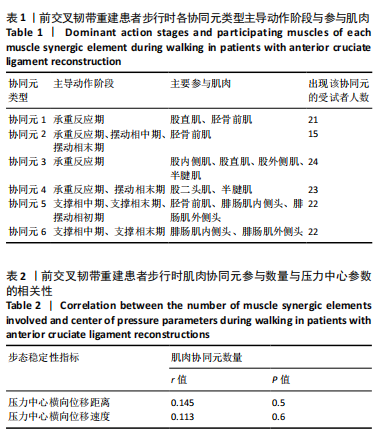
2.1 参与者数量分析 24例受试者在测试过程中均未发生不良事件,全部纳入结果分析。 2.2 前交叉韧带重建患者步行时患侧腿部肌肉协同元参与数量与步态稳定性相关性分析 对每位前交叉韧带重建患者的患肢腿部肌电信号矩阵进行非负矩阵分解,计算了1-10协同元解析数量对应的重构矩阵变异度,确定患侧腿肌肉协同元的参与数量,见图1A,B。随后,基于皮尔森相关系数计算,评估了解析出的肌肉协同元向量相似度,合并相似度高于0.6的肌肉协同元,以区分解析出的肌肉协同元类型。基于上述处理工作,解构出了前交叉韧带重建患者步行时患侧腿肌肉协同模式图,见图1C。此次累计解析出6类肌肉协同元参与患者步态活动,各协同元主要参与肌肉与主导动作阶段见图1C、表1。将各受试者患侧腿参与的肌肉协同元数量与步态稳定性指标进行相关性分析发现,下肢肌肉协同元参与数量与患者步行时压力中心横向位移距离、压力中心横向位移速度均无显著相关性(r=0.145,P=0.5;r=0.113,P=0.6),见表2。"
|
[1] LU W, LIU D, CAI Z, et al. Protocol: Internal brace augmentation reconstruction versus standard anterior cruciate ligament reconstruction: a randomised controlled clinical trial study protocol. BMJ Open. 2023;13(12):e065254. [2] DUONG TD, TRAN DT, DO BNT, et al. All-inside arthroscopic anterior cruciate ligament reconstruction with internal brace Ligament Augmentation using semitendinosus tendon autograft: A case series. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2022;29:15-21. [3] BLECHA K, NUELLE CW, SMITH PA, et al. Efficacy of prophylactic knee bracing in sports. J Knee Surg. 2022;35(3):242-248. [4] LYNCH AD, CHMIELEWSKI T, BAILEY L, et al. Current concepts and controversies in rehabilitation after surgery for multiple ligament knee injury. Curr Rev Musculoskelet Med. 2017;10:328-345. [5] OTZEL DM, CHOW JW, TILLMAN MD. Long-term deficits in quadriceps strength and activation following anterior cruciate ligament reconstruction. Phys Ther Sport. 2015;16(1):22-28. [6] GARCIA SA, CURRAN MT, PALMIERI-SMITH RM. Longitudinal assessment of quadriceps muscle morphology before and after anterior cruciate ligament reconstruction and its associations with patient-reported outcomes. Sports Health. 2020;12(3):271-278. [7] LEPLEY LK, DAVI SM, BURLAND JP, et al. Muscle atrophy after ACL injury: implications for clinical practice. Sports Health. 2020;12(6):579-586. [8] TZAGARAKIS GN, TSIVGOULIS SD, PAPAGELOPOULOS PJ, et al. Influence of acute anterior cruciate ligament deficiency in gait variability. J Int Med Res. 2010;38(2):511-525. [9] KARIMIJASHNI M, SARVESTANI FK, YOOSEFINEJAD AK. The effect of contralateral knee neuromuscular exercises on static and dynamic balance, knee function, and pain in athletes who underwent anterior cruciate ligament reconstruction: a single-blind randomized controlled trial. J Sport Rehabil. 2023;32(5):524-539. [10] LEGNANI C, VENTURA A, MANGIAVINI L, et al. Management of medial femorotibial knee osteoarthritis in conjunction with anterior cruciate ligament deficiency: technical note and literature review. J Clinical Med. 2024;13(11):3143. [11] CURADO J, HULET C, HARDY P, et al. Very long-term osteoarthritis rate after anterior cruciate ligament reconstruction: 182 cases with 22-year’follow-up. Orthop Traumatol Surg Res. 2020;106(3):459-463. [12] SENORSKI EH, SUNDEMO D, SVANTESSON E, et al. Preoperative and intraoperative predictors of long-term acceptable knee function and osteoarthritis after anterior cruciate ligament reconstruction: an analysis based on 2 randomized controlled trials. Arthroscopy. 2019; 35(2):489-499. [13] ADRAVANTI P, BUDHIPARAMA NC, BEREND KR, et al. ACL-deficient knee and unicompartmental OA: state of the art. J ISAKOS. 2017;2(3):162-170. [14] HART JM, KO J WK, KONOLD T, et al. Sagittal plane knee joint moments following anterior cruciate ligament injury and reconstruction: a systematic review. Clin Biomech. 2010;25(4):277-283. [15] SHARIFI M, SHIRAZI-ADL A, MAROUANE H. Computational stability of human knee joint at early stance in Gait: Effects of muscle coactivity and anterior cruciate ligament deficiency. J Biomech. 2017;63:110-116. [16] SHIRAZI-ADL A, SHARIFI M. Knee flexion angle and muscle activations control the stability of an anterior cruciate ligament deficient joint in gait. J Biomech. 2021;117:110258. [17] VERNOOIJ CA, GUILLAUME R, ERIC B, et al. The effect of aging on muscular dynamics underlying movement modes changes. Front Aging Neurosci. 2016;8(12):309-321. [18] HOOPER DM, MORRISSEY MC, DRECHSLER WI, et al. Gait analysis 6 and 12 months after anterior cruciate ligament reconstruction surgery. Clin Orthop Relat Res. 2002;10(403):168-178. [19] AN EGMOND N, STOLWIJK N, VAN HEERWAARDEN R, et al. Gait analysis before and after corrective osteotomy in patients with knee osteoarthritis and a valgus deformity. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2904-2913. [20] HATAMZADEH M, HASSANNEJAD R, SHARIFNEZHAD A. A new method of diagnosing athlete’s anterior cruciate ligament health status using surface electromyography and deep convolutional neural network. Biocybern Biomed Eng. 2019;40(1):65-76. [21] VISSCHER RMS, SANSGIRI S, FRESLIER M, et al. Towards validation and standardization of automatic gait event identification algorithms for use in paediatric pathological populations. Gait Posture. 2021;86:64-69. [22] 畠中泰彦.姿势•动作•步态分析[M].北京:北京科学技术出版社,2021:21-23. [23] 魏梦力,钟亚平,周易文,等.单侧前交叉韧带重建患者步行双侧下肢肌肉协同模式差异[J].中国康复理论与实践,2024,30(1):95-104. [24] DUTTA A, KHATTAR B, BANERJEE A. Nonlinear analysis of electromyogram following gait training with myoelectrically triggered neuromuscular electrical stimulation in stroke survivors. Eurasip J Adv Sig Pr. 2012;2012(1):153-161. [25] KOBLBAUER IF, VAN KS, VERHAGEN EA, et al. Kinematic changes during running-induced fatigue and relations with core endurance in novice runners. J Sci Med Sport. 2014;17(4):419-424. [26] LEE DD, SEUNG HS. Learning the parts of objects by non-negative matrix factorization. Nature. 1999;401(675):788-791. [27] ALLEN JL, KESAR TM, TING LH. Motor module generalization across balance and walking is impaired after stroke. J Neurophysiol. 2019; 122(1):277-289. [28] ROH J, RYMER WZ, BEER RF. Robustness of muscle synergies underlying three-dimensional force generation at the hand in involved humans. J Neurophysiol. 2012;107(8):2123-2142. [29] BANKS CL, PAI MM, MCGUIRK TE, et al. Methodological Choices in Muscle Synergy Analysis Impact Differentiation of Physiological Characteristics Following Stroke. Front Comput Neurosci. 2017;11:1-12. [30] LI ZHICAI, ZHAO XINYU, WANG ZIYAO, et al. A hierarchical classification of gestures under two force levels based on muscle synergy. Biomed Signal Process Control. 2022;77:1-13. [31] YOKOYAMA H, OGAWA T, KAWASHIMA N, et al. Distinct sets of locomotor modules control the speed and modes of human locomotion. Sci Rep. 2016;6(1):1-14. [32] KIM M, KIM Y, KIM H, et al. Specific muscle synergies in national elite female ice hockey players in response to unexpected external perturbation. J Sports Sci. 2018;36(3):319-325. [33] 熊启亮.婴幼儿膝爬运动功能发育状态对肌肉收缩及关节运动协同模式的影响[D].重庆:重庆大学,2019:45-46. [34] HAJILOO B, ANBARIAN M, ESTAEILI H, et al. The effects of fatigue on synergy of selected lower limb muscles during running. J Biomech. 2020;103(4):1-6. [35] STEELE KM, ROZUMALSKI A, SCHWARTZ MH. Muscle synergies and complexity of neuromuscular control during gait in cerebral palsy. Dev Med Child Neurol. 2016;57(12):1176-1182. [36] SHAHARUDIN S, AGRAWAL S. Muscle synergies during incremental rowing VO2max test of collegiate rowers and untrained subjects. Br J Sports Med. 2015;56(9):980-989. [37] BERCHUCK M, ANDRIACCHI TP, BACH BR, et al. Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am. 1990;2(6):871-877. [38] SAITO A, TOMITA A, ANDO R, et al. Muscle synergies are consistent across level and uphill treadmill running. Sci Rep. 2018;8(1):1-10. [39] GILANI K., MOHAMMADIPOUR F, AMIRSEYFADDINI M. Comparison of maximum angles of knee varus and flexion in the stance phase of walking on a treadmill with different inclinations between female athletes with genu valgum and healthy knees. J Res Rehabil Sci. 2020; 16(1):142-150. |
| [1] | Shaban Amiri Nzelekela, Yang Lianbo, Li Peng. Objective accuracy of six degree of freedom gait analysis system in evaluating the severity of knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(27): 5890-5896. |
| [2] | Wang Xia, Xue Boshi, Yang Chen, Zhou Zhipeng, Zheng Liangliang. Influence of neuromuscular function on the risk of biomechanical injury in landing manoeuvres in patients undergoing anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(26): 5556-5562. |
| [3] | Liu Jing, Xu Chunxin, Lu Yangyang, Qu Qinquan, Zhu Qi, Guo Yulan, Shen Min. Correlation of gait parameters and muscle parameters with imaging in adolescent idiopathic scoliosis patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4477-4485. |
| [4] | Chen Wenhan, Men Jie, Yang Wei, Zhao Xiaoyu. Effect of vibration therapy combined with suspension training on movement and knee joint function after anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(11): 2225-2230. |
| [5] | He Rongzhen, Ying Lyufang, He Xingwen, Chen Chuanshun, Yin Yuesong, Zhang Kexiang, Wang Zili. Effect of ginsenoside Rg1 on muscle degeneration after massive rotator cuff injury in mice [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5136-5140. |
| [6] | Zhu Chenchen, Yin Yuan, Zhou Yingji, Ma Tingting, Su Liyao, Zhang Ming. Effects of body mass index on plantar pressure [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(18): 2808-2813. |
| [7] | Chen Modi, Sun Qibo, Xu Tianyu, Tai Guoliang, Zhao Yuxiang, Pan Zhaohui. Biomechanics of reconstruction of total calcaneus defect using fibular flap based on finite element method [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(12): 1805-1809. |
| [8] | Gu Xu, Zheng Xin, Shi Sifeng, Lu Renxiang, Cao Jie, Li Hongwei. Stability of early gait after unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(12): 1875-1879. |
| [9] | Zhong Jiamin, Huang Zhaoxin, Li Longxue, Qu Tongtong, Liu Zhuang, Fu Yifeng, Xiao Xiaofei. Effects of visual factors on balance function in young adults [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1245-1249. |
| [10] | Yu Wenqiang, Ren Fuchao, Shi Guohong, Xu Yuanjing, Liu Tongyou, Xie Youzhuan, Wang Jinwu, . Methods and application of gait analysis of lower limbs after stroke [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1257-1263. |
| [11] | Li Shihao, Li Qi, Li Zhen, Zhang Yuanyuan, Liu Miaomiao, Ouyang Yi, Xu Weiguo. Plantar pressure and gait analysis in patients with anterior cruciate ligament injury and reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 626-631. |
| [12] | Yang Qiang, Huang Jian. Measurement research method and measurement equipment for knee-spine syndrome [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(29): 4751-4756. |
| [13] | Liu Xinhao, Ma Xinran, Yang Shengyong, Wang Yanyu, Ma Shujie. Influence of Tuina manipulation on walking dysfunction in rats with sciatic nerve injury [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(26): 4101-4106. |
| [14] | Jin Naying, Wu Jiabao, Li Yuyue, Li Yingjie, Zhou Li, Li Zongheng, Zhang Yong. Gait analysis for hemiplegic patients with cerebral infarction based on RSSCAN gait system [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(23): 3609-3615. |
| [15] | Liu Gang, Ma Chao, Wang Le, Zeng Jie, Jiao Yong, Zhao Yi, Ren Jingpei, Hu Chuanyu, Xu Lin, Mu Xiaohong. Ankle-foot orthoses improve motor function of children with cerebral palsy: a Meta-analysis based on 12 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1299-1304. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||