Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (14): 2892-2898.doi: 10.12307/2025.605
Previous Articles Next Articles
Potential effects of ornidazole on intracanal vascularization in endodontic regeneration
Li Zikai, Zhang Chengcheng, Xiong Jiaying, Yang Xirui, Yang Jing, Shi Haishan
- School of Stomatology, Jinan University, Guangzhou 510632, Guangdong Province, China
-
Received:2024-04-30Accepted:2024-07-06Online:2025-05-18Published:2024-09-27 -
Contact:Shi Haishan, PhD, Associate professor, Master’s supervisor, School of Stomatology, Jinan University, Guangzhou 510632, Guangdong Province, China -
About author:Li Zikai, School of Stomatology, Jinan University, Guangzhou 510632, Guangdong Province, China -
Supported by:Basic and Applied Basic Research Project of Guangzhou Science and Technology Program, No. 202102021127 (to SHS)
CLC Number:
Cite this article
Li Zikai, Zhang Chengcheng, Xiong Jiaying, Yang Xirui, Yang Jing, Shi Haishan. Potential effects of ornidazole on intracanal vascularization in endodontic regeneration[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(14): 2892-2898.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

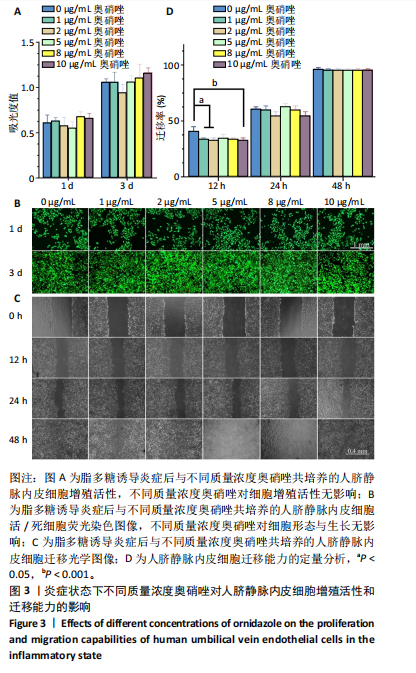
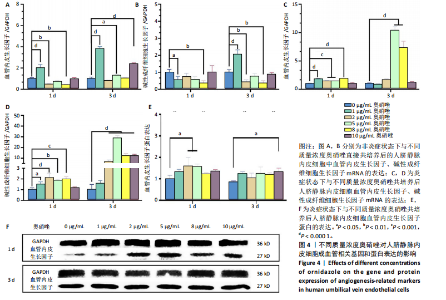
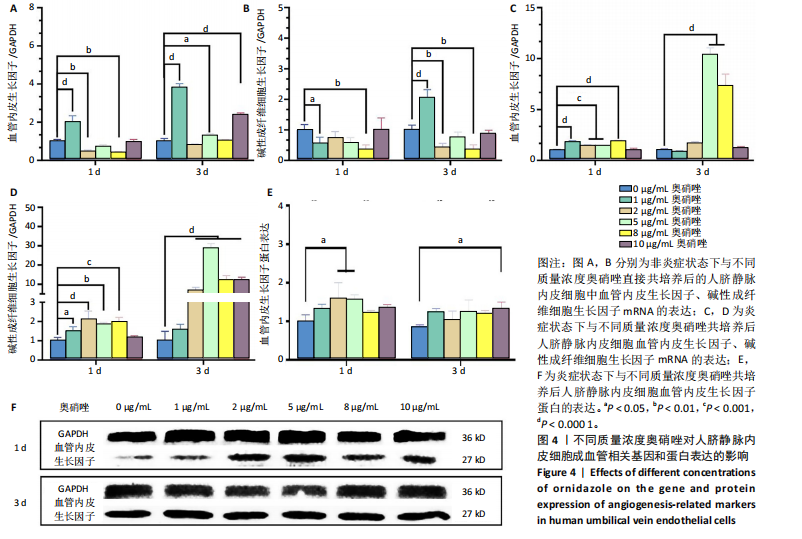
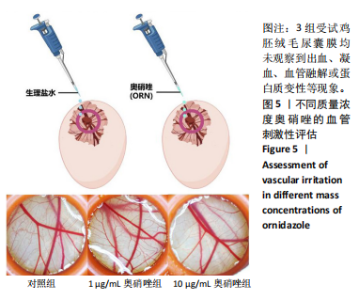
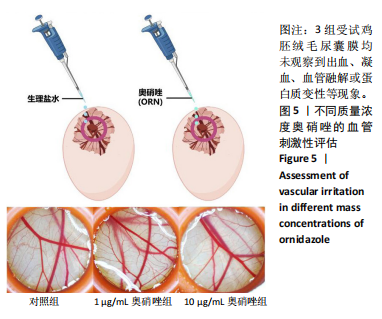
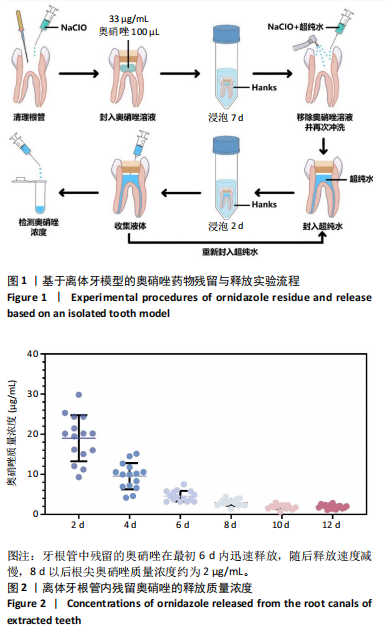
2.1 牙根管内奥硝唑的残留与释放 图2给出了牙根管内中奥硝唑的释放质量浓度。在清理、封药后,从牙根管内游离出来的残留奥硝唑质量浓度达到(19.5±5.7) μg/mL,随着时间的推移,残留奥硝唑的释放质量浓度逐渐降低,6 d后明显降至(5.5±1.3) μg/mL,在后期则维持接近2 μg/mL的释放水平。这表明即使在根管清理后仍能检测到奥硝唑的明显残留,并且这些奥硝唑会不断地释放出来持续影响后续生物学事件。 2.2 不同质量浓度奥硝唑对人脐静脉内皮细胞活性与迁移能力的影响 参考奥硝唑药物在离体牙模型中的释放水平,探讨不同质量浓度(1-10 μg/mL)奥硝唑对人脐静脉内皮细胞行为的影响。在脂多糖诱导的炎症条件下与不同质量浓度奥硝唑共培养后,人脐静脉内皮细胞随着时间推移逐渐生长。CCK-8检测结果显示,共培养1,3 d后,与对照组相比,1-10 μg/mL奥硝唑对人脐静脉内皮细胞的增殖无明显影响(P > 0.05),见图3A;活死细胞荧光染色显示各组细胞均具有良好的生长形态,细胞存活率较高,见图3B,表明1-10 μg/mL奥硝唑具有良好的细胞相容性。细胞划痕实验结果显示,不同质量浓度奥硝唑(尤其是10 μg/mL)会在一定程度上抑制人脐静脉内皮细胞在共培养初期(12 h)的迁移活动,而后期(24-72 h)的这种抑制作用基本消除,见图3C,D。 综合实验结果,整体上,1-10 μg/mL奥硝唑对人脐静脉内皮细胞的增殖活性和迁移能力无明显负面影响。 2.3 不同质量浓度奥硝唑对人脐静脉内皮细胞成血管相关基因和蛋白表达的影响 RT-qPCR检测结果显示,整体上,与不同质量浓度奥硝唑直接共培养后,人脐静脉内皮细胞中血管内皮生长因子和碱性成纤维细胞生长的mRNA表达下调(图4A,B)。直接共培养1 d,与对照组比较,1 μg/mL奥硝唑组血管内皮生长因子mRNA表达升高(P < 0.000 1),2,8 μg/mL奥硝唑组血管内皮生长因子mRNA表达降低(P < 0.01);1,8 μg/mL奥硝唑组碱性成纤维细胞生长因子mRNA表达降低(P < 0.05,P < 0.01);直接共培养3 d,与对照组比较,1 μg/mL奥硝唑组血管内皮生长因子、碱性成纤维细胞生长因子mRNA表达升高(P < 0.000 1),5,10 μg/mL奥硝唑组血管内皮生长因子mRNA表达升高(P < 0.05,P < 0.000 1),2,8 μg/mL奥硝唑组碱性成纤维细胞生长因子mRNA表达降低(P < 0.01)。 在脂多糖诱导的炎症条件下,整体上,与不同质量浓度奥硝唑直接共培养后,人脐静脉内皮细胞中血管内皮生长因子和碱性成纤维细胞生长因子mRNA表达上调(图4C,D)。共培养1 d,与对照组比较,1-8 μg/mL奥硝唑组血管内皮生长因子、碱性成纤维细胞生长因子mRNA表达均升高(P < 0.05,P < 0.01,P < 0.001,P < 0.000 1);共培养3 d,与对照组比较,5,8 μg/mL奥硝唑组血管内皮生长因子mRNA表达升高(P < 0.000 1),2-10 μg/mL奥硝唑组碱性成纤维细胞生长因子mRNA表达均升高(P < 0.000 1)。 Western blot检测结果显示,在脂多糖诱导的炎症条件下,与对照组比较,2,5 μg/mL奥硝唑组共培养1 d、10 μg/mL奥硝唑组共培养3 d血管内皮生长因子蛋白表达升高(P < 0.05),见图4E,F。 2.4 不同质量浓度奥硝唑对血管的刺激性评估 3组受试尿囊膜均未观察到出血、凝血、血管融解或蛋白质变性等现象,见图5,表明适量质量浓度的奥硝唑对血管无毒性效应,即对组织血管化无明显负面影响。"
| [1] GALLER K M, WEBER M, KORKMAZ Y, et al. Inflammatory Response Mechanisms of the Dentine-Pulp Complex and the Periapical Tissues. Int J Mol Sci. 2021;22(3):1480. [2] TATULLO M, MARRELLI M, SHAKESHEFF KM, et al. Dental pulp stem cells: function, isolation and applications in regenerative medicine. J Tissue Eng Regener Med. 2015;9(11):1205-1216. [3] LEÓN-LÓPEZ M, CABANILLAS-BALSERA D, MARTÍN-GONZÁLEZ J, et al. Prevalence of root canal treatment worldwide: A systematic review and meta-analysis. Int Endod J. 2022;55(11):1105-1127. [4] LU JM, LI ZH, WU X, et al. iRoot BP Plus promotes osteo/odontogenic differentiation of bone marrow mesenchymal stem cells via MAPK pathways and autophagy. Stem Cell Res Ther. 2019;10:1-14. [5] SIQUEIRA JF. Aetiology of root canal treatment failure: why well-treated teeth can bail. Int Endod J. 2001;34(1):1-10. [6] RODRIGUES M, KOSARIC N, BONHAM CA, et al. Wound healing: a cellular perspective. Physiol Rev. 2019;99(1):665-706. [7] HERBERT SP, STAINIER DYR. Molecular control of endothelial cell behaviour during blood vessel morphogenesis. Nat Rev Mol Cell Biol. 2011;12(9):551-564. [8] KOTTOOR J, VELMURUGAN N. Revascularization for a necrotic immature permanent lateral incisor: a case report and literature review. Int J Paediatr Dent. 2013;23(4):310-316. [9] MEHRVARZFAR P, ABBOTT PV, AKHAVAN H, et al. Modified Revascularization in Human Teeth Using an Intracanal Formation of Treated Dentin Matrix: A Report of Two Cases. J Int Soc Prev Community Dent. 2017;7(4):218-221. [10] ZHANG S, ZHANG W, LI Y, et al. Cotransplantation of human umbilical cord mesenchymal stem cells and endothelial cells for angiogenesis and pulp regeneration in vivo. Life Sci. 2020;255:117763. [11] HUANG X, LI Z, LIU A, et al. Microenvironment Influences Odontogenic Mesenchymal Stem Cells Mediated Dental Pulp Regeneration. Front Physiol. 2021;12:656588. [12] XIA K, CHEN Z, CHEN J, et al. RGD- and VEGF-Mimetic Peptide Epitope-Functionalized Self-Assembling Peptide Hydrogels Promote Dentin-Pulp Complex Regeneration. Int J Nanomed. 2020;15:6631-6647. [13] MILTIADOUS ME, FLORATOS SG. Regenerative Endodontic Treatment as a Retreatment Option for a Tooth with Open Apex - A Case Report. Braz Dent J. 2015;26(5):552-556. [14] HILKENS P, BRONCKAERS A, RATAJCZAK J, et al. The Angiogenic Potential of DPSCs and SCAPs in an <i>In Vivo</i> Model of Dental Pulp Regeneration. Stem Cells Int. 2017;2017(1):2582080. [15] DOS SANTOS LRK, PELEGRINE AA, BUENO CED, et al. Pulp-Dentin Complex Regeneration with Cell Transplantation Technique Using Stem Cells Derived from Human Deciduous Teeth: Histological and Immunohistochemical Study in Immunosuppressed Rats. Bioengineering (Basel). 2023;10(5):610. [16] DIOGUARDI M, DI GIOIA G, ILLUZZI G, et al. Inspection of the Microbiota in Endodontic Lesions. Dent J (Basel). 2019;7(2):47. [17] LACEVIC A, BILALOVIC N, KAPIC A. Bacterial aggregation in infected root canal. Bosn J Basic Med Sci. 2005;5(4):35-39. [18] ZHANG C, YANG Z, HOU B. Diverse bacterial profile in extraradicular biofilms and periradicular lesions associated with persistent apical periodontitis. Int Endod J. 2021;54(9):1425-1433. [19] KIRYU T, HOSHINO E, IWAKU M. Bacteria invading periapical cementum. J Endod. 1994;20(4):169-172. [20] ZHANG W, WANG QQ, WANG KR, et al. Construction of an ornidazole/bFGF-loaded electrospun composite membrane with a core-shell structure for guided tissue regeneration. Mater Des. 2022;221:110960. [21] SABRAH AHA, YASSEN GH, SPOLNIK KJ, et al. Evaluation of residual antibacterial effect of human radicular dentin treated with triple and double antibiotic pastes. J Endod. 2015;41(7):1081-1084. [22] DUBEY N, XU J, ZHANG Z, et al. Comparative Evaluation of the Cytotoxic and Angiogenic Effects of Minocycline and Clindamycin: An In Vitro Study. J Endod. 2019;45(7):882-889. [23] ZHAO Y, CHEN Z, HUANG P, et al. Analysis of Ornidazole injection in clinical use at post-marketing stage by centralized hospital monitoring system. Curr Med Sci. 2019;39:836-842. [24] TORT H, OKTAY EA, TORT S, et al. Evaluation of ornidazole-loaded nanofibers as an alternative material for direct pulp capping. J Drug Delivery Sci Technol. 2017;41:317-324. [25] TASANARONG P, AYUDHYA TDN, TECHANITISWAD T, et al. Reduction of viable bacteria in dentinal tubules treated with a novel medicament (Z-Mix). J Dent Sci. 2016;11(4):419-426. [26] ZHANG SY, THIEBES AL, KREIMENDAHL F, et al. Extracellular Vesicles-Loaded Fibrin Gel Supports Rapid Neovascularization for Dental Pulp Regeneration. Int J Mol Sci. 2020;21(12):4226. [27] 王玉娟,褚美芬,罗冬娇,等.不同5′-硝基咪唑类药物治疗厌氧菌性及滴虫性阴道炎临床疗效比较[J].上海医学,2006,29(6):375-378. [28] GIRAUD T, JEANNEAU C, ROMBOUTS C, et al. Pulp capping materials modulate the balance between inflammation and regeneration. Dent Mater. 2019;35(1):24-35. [29] GOLDBERG M, NJEH A, UZUNOGLU E. Is pulp inflammation a prerequisite for pulp healing and regeneration? Mediators Inflammation. 2015;2015(1):347649. [30] BINDAL P, RAMASAMY TS, KASIM NHA, et al. Immune responses of human dental pulp stem cells in lipopolysaccharide‐induced microenvironment. Cell Biol Int. 2018;42(7):832-840. [31] IOHARA K, TOMINAGA M, WATANABE H, et al. Periapical bacterial disinfection is critical for dental pulp regenerative cell therapy in apical periodontitis in dogs. Stem Cell Res Ther. 2024;15(1):17. [32] AMINOSHARIAE A, KULILD JC. Evidence-based recommendations for antibiotic usage to treat endodontic infections and pain: A systematic review of randomized controlled trials. J Am Dent Assoc. 2016;147(3):186-191. [33] JAVAN NKN, BARADARAN LM, AZIMI S. SEM study of root canal walls cleanliness after Ni-Ti rotary and hand instrumentation. Iran Endod J. 2007;2(1):5. [34] SUN NN, WANG NN, QU LN. Clinical Symptoms and Quality of Life Improvement Value of Ornidazole Mixture in Auxiliary Filling Treatment of Patients with Endodontic Disease. Contrast Media Mol Imaging. 2022;2022:7181258. [35] DU RB, BA K, YANG YX, et al. Efficacy of ornidazole for pericoronitis: a meta-analysis and systematic review. Arch Med Sci. 2024;20(1):189-195. [36] CARMELIET P. Angiogenesis in life, disease and medicine. Nature. 2005; 438(7070):932-936. [37] LUEPKE NP. Hen’s egg chorioallantoic membrane test for irritation potential. Food Chem Toxicol. 1985;23(2):287-291. [38] FENTEM JH. Book Review: Methods in Molecular Biology Volume 43: In Vitro Toxicity Testing Protocols. SAGE Publications Sage UK: London, England, 1995. [39] FERRARA N. From the discovery of vascular endothelial growth factor to the introduction of avastin in clinical trials-an interview with Napoleone Ferrara by Domenico Ribatti . Int J Dev Biol. 2011;55(4-5):383-388. [40] BREIER G, ALBRECHT U, STERRER S, et al. Expression of vascular endothelial growth factor during embryonic angiogenesis and endothelial cell differentiation. Development. 1992;114(2):521-532. [41] SAKAI VT, ZHANG Z, DONG Z, et al. SHED differentiate into functional odontoblasts and endothelium. J Dent Res. 2010;89(8):791-796. |
| [1] | Li Zikai, Zhang Chengcheng, Xiong Jiaying, Yang Xirui, Yang Jing, Shi Haishan. Potential effects of ornidazole on intracanal vascularization in endodontic regeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-7. |
| [2] | Han Haihui, Ran Lei, Meng Xiaohui, Xin Pengfei, Xiang Zheng, Bian Yanqin, Shi Qi, Xiao Lianbo. Targeting fibroblast growth factor receptor 1 signaling to improve bone destruction in rheumatoid arthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1905-1912. |
| [3] | Jing Ruyi, Chen Yingxin, Cao Lei . Prognosis of deep lamellar keratoplasty versus penetrating keratoplasty in the treatment of stromal corneal dystrophy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1626-1633. |
| [4] | Lou Guo, Zhang Min, Fu Changxi. Exercise preconditioning for eight weeks enhances therapeutic effect of adipose-derived stem cells in rats with myocardial infarction [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1363-1370. |
| [5] | Ba Yanhong, Gao Minghong, Chen Yingxin. Impact of graft thickness on corneal endothelial decompensation following simple Descemet’s stripping endothelial keratoplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1199-1207. |
| [6] | Gao Yang, Qin Hewei, Liu Dandan. ACSL4 mediates ferroptosis and its potential role in atherosclerotic cardiovascular disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1239-1247. |
| [7] | Han Haihui, Meng Xiaohu, Xu Bo, Ran Le, Shi Qi, Xiao Lianbo. Effect of fibroblast growth factor receptor 1 inhibitor on bone destruction in rats with collagen-induced arthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 968-977. |
| [8] | Fang Yuan, Qian Zhiyong, He Yuanhada, Wang Haiyan, Sha Lirong, Li Xiaohe, Liu Jing, He Yachao, Zhang Kai, Temribagen. Mechanism of Mongolian medicine Echinops sphaerocephalus L. in proliferation and angiogenesis of vascular endothelial cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7519-7528. |
| [9] | Zhao Jianwei, Li Xunsheng, Lyu Jinpeng, Zhou Jue, Jiang Yidi, Yue Zhigang, Sun Hongmei. Deer antler stem cell exosome composite hydrogel promotes the repair of burned skin [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7344-7352. |
| [10] | Pan Chun, Fan Zhencheng, Hong Runyang, Shi Yujie, Chen Hao. Effect and mechanism of polystyrene microplastics on prostate in male mice [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7353-7361. |
| [11] |
Zhou Rulin, Hu Yuanzheng, Wang Zongqing, Zhou Guoping, Zhang Baochao, Xu Qian, Bai Fanghui.
Exploration of biomarkers for moyamoya disease and analysis of traditional Chinese medicine targets#br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6927-6938.
|
| [12] | Zeng Yu, Xie Chengwei, Hong Yuanqi, Su Shenghui, Dong Xieping. In vitro angiogenesis and osteogenesis properties of copper-doped mesoporous bioactive glass [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(28): 5941-5949. |
| [13] | Li Zeming, Zhang Yuntao, Wang Maolin, Hou Yudong. Role and mechanism of hypoxia-inducible factor 1 alpha regulating bone homeostasis in oral and maxillofacial diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(26): 5680-5687. |
| [14] | Wang Lei, Wang Baiyan, Zhou Chunguang, Ren Xiaoyun, Dai Yueyou, Feng Shuying. Role of different cell-derived exosomal miRNAs in progression, diagnosis, and prognosis of gastric cancer [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(25): 5434-5442. |
| [15] | Song Qinghong, Wu Nan, Shi Yan, Cui Hongyu, Liu Fei, Liu Hanchong, Zhou Ning, Yao Bin. Angiopoietin-like protein 4 affects progression of diabetic foot by regulating fibroblast and endothelial cell functions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(25): 5396-5402. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||