Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (7): 1363-1370.doi: 10.12307/2025.007
Previous Articles Next Articles
Exercise preconditioning for eight weeks enhances therapeutic effect of adipose-derived stem cells in rats with myocardial infarction
Lou Guo1, Zhang Min2, Fu Changxi3
- 1Jiangsu Vocational Institute of Commerce, Nanjing 211168, Jiangsu Province, China; 2Nanjing Vocational College of Tourism, Nanjing 211100, Jiangsu Province, China; 3Department of Physical Education, Xuzhou University of Technology, Xuzhou 221008, Jiangsu Province, China
-
Received:2023-11-23Accepted:2024-01-10Online:2025-03-08Published:2024-06-27 -
Contact:Fu Changxi, Doctoral candidate, Associate professor, Department of Physical Education, Xuzhou University of Technology, Xuzhou 221008, Jiangsu Province, China -
About author:Lou Guo, Master, Lecturer, Jiangsu Vocational Institute of Commerce, Nanjing 211168, Jiangsu Province, China -
Supported by:Jiangsu Provincial Social Science Foundation Project, No. 22TYD001 (to FCX)
CLC Number:
Cite this article
Lou Guo, Zhang Min, Fu Changxi. Exercise preconditioning for eight weeks enhances therapeutic effect of adipose-derived stem cells in rats with myocardial infarction[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1363-1370.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

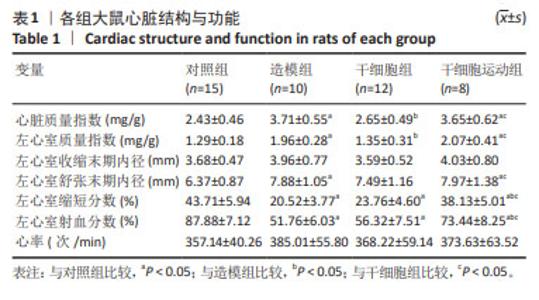
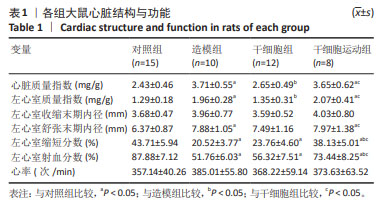
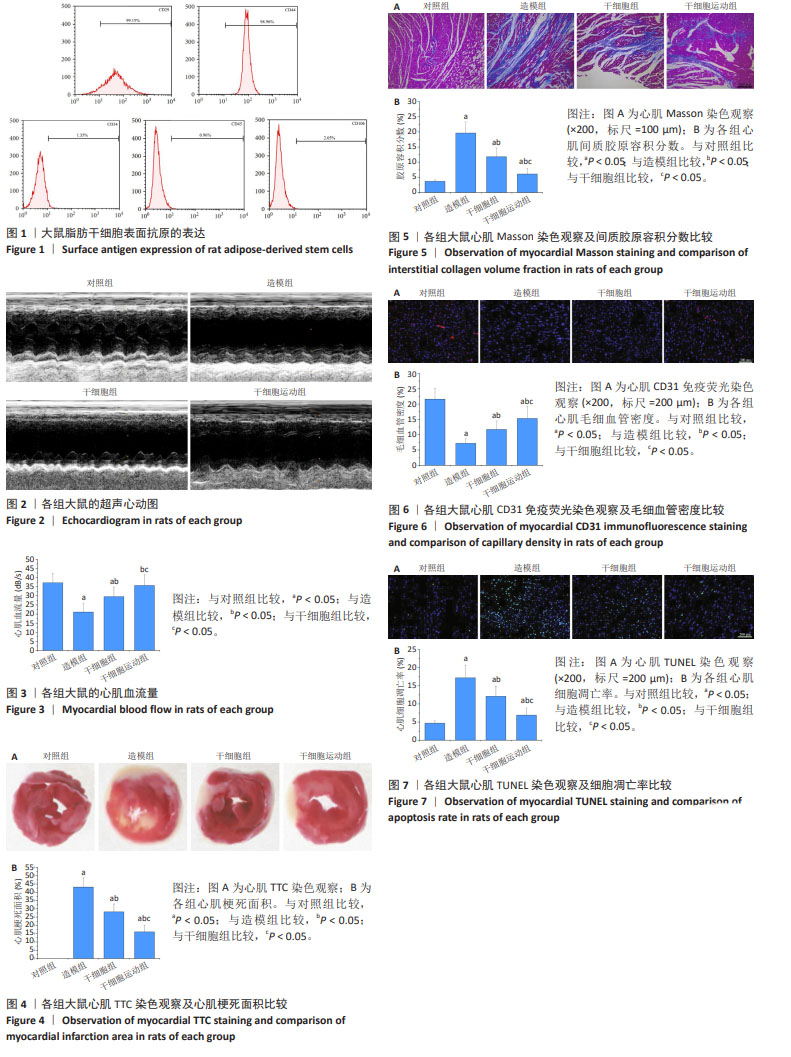
2.1 脂肪干细胞鉴定结果 利用流式细胞仪检测培养细胞表面抗原阳性表达率,结果显示,CD29和CD44(间充质干细胞标志物)高表达(CD29:99.15%;CD44:98.96%),CD34、CD45和CD106(造血干细胞表面标志物)低表达(CD34:1.35%;CD45:0.96%;CD106:2.05%),提示所培养的脂肪干细胞符合间充质干细胞特征,见图1。 2.2 心脏结构和功能 与对照组比较,造模组和干细胞运动组心脏质量指数、左心室质量指数、左心室舒张末期内径升高(P < 0.05),左心室缩短分数、左心室射血分数降低(P < 0.05)。与造模组比较,干细胞组心脏质量指数、左心室质量指数下降(P < 0.05),干细胞运动组心脏质量指数、左心室质量指数、左心室舒张末期内径无显著性变化(P > 0.05),左心室缩短分数、左心室射血分数增加(P < 0.05)。与干细胞组比较,干细胞运动组心脏质量指数、左心室质量指数、左心室舒张末期内径、左心室缩短分数、左心室射血分数升高(P < 0.05)。各组左心室收缩末期内径和心率比较均无显著性差异(P > 0.05)。见图2和表1。 "

2.3 心肌血流量 与对照组比较,造模组心肌血流量下降(P < 0.05);与造模组比较,干细胞组和干细胞运动组心肌血流量升高(P < 0.05);与干细胞组比较,干细胞运动组心肌血流量进一步改善(P < 0.05),见图3。 2.4 心肌梗死面积和间质胶原沉积 TTC是呼吸链中的质子受体,与正常组织中的脱氢酶反应而呈红色(非梗死区),而缺血组织内脱氢酶活性下降而不能与TTC反应,故呈现苍白色(梗死区),见图4A。与对照组比较,造模组心肌梗死面积升高(P < 0.05);与造模组比较,干细胞组和干细胞运动组心肌梗死面积下降(P < 0.05);与干细胞组比较,干细胞运动组心肌梗死面积进一步降低(P < 0.05),见图4B。 心肌Masson三色染色中,胶原纤维被苯胺蓝染成蓝色,肌纤维被酸性品红和丽春红染成红色,见图5A。与对照组比较,造模组心肌间质胶原容积分数增加(P < 0.05);与造模组比较,干细胞组和干细胞运动组胶原容积分数降低(P < 0.05);与干细胞组比较,干细胞运动组胶原容积分数进一步下调(P < 0.05),见图5B。 2.5 心肌毛细血管密度 CD31免疫荧光染色显示,CD31阳性细胞均呈现红色荧光,细胞核蓝染,见图6A。与对照组比较,造模组毛细血管密度降低(P < 0.05);与造模组比较,干细胞组和干细胞运动组毛细血管密度升高(P < 0.05);与干细胞组比较,干细胞运动组毛细血管密度进一步增加(P < 0.05),见图6B。 2.6 心肌细胞凋亡 TUNEL染色显示,阳性细胞呈现绿色荧光,细胞核蓝染,见图7A。与对照组比较,造模组细胞凋亡率升高(P < 0.05);与造模组比较,干细胞组和干细胞运动组细胞凋亡率降低(P < 0.05);与干细胞组比较,干细胞运动组细胞凋亡率进一步下降(P < 0.05),见图7B。 2.7 心肌蛋白表达量 干细胞移植后1 d:与对照组比较,造模组t-Akt、p-Akt、VEGF、t-eNOS和p-eNOS无显著性变化(P > 0.05);与造模组比较,干细胞组上述指标均无显著性变化(P > 0.05),干细胞运动组p-Akt蛋白表达和p-Akt/t-Akt比值上调(P < 0.05),见图8A-D。 干细胞移植后7 d:与对照组比较,造模组p-Akt、VEGF和p-eNOS蛋白表达量以及p-Akt/t-Akt和p-eNOS/t-eNOS比值下降(P < 0.05);与造模组比较,干细胞组各参数均无显著性变化(P > 0.05),干细胞运动组p-Akt、VEGF和p-eNOS蛋白表达量以及p-Akt/t-Akt和p-eNOS/t-eNOS比值升高(P < 0.05),见图9A-D。 "

| [1] DAUERMAN HL, IBANEZ B. The edge of time in acute myocardial infarction. J Am Coll Cardiol. 2021;77(15):1871-1874. [2] SAITO Y, OYAMA K, TSUJITA K, et al. Treatment strategies of acute myocardial infarction: updates on revascularization, pharmacological therapy, and beyond. J Cardiol. 2023;81(2):168-178. [3] FRANTZ S, HUNDERTMARK MJ, SCHULZ-MENGER J, et al. Left ventricular remodelling post-myocardial infarction: pathophysiology, imaging, and novel therapies. Eur Heart J. 2022;43(27):2549-2561. [4] WANG L, MA Y, JIN W, et al. Coronary microcirculation dysfunction evaluated by myocardial contrast echocardiography predicts poor prognosis in patients with ST-segment elevation myocardial infarction after percutaneous coronary intervention. BMC Cardiovasc Disord. 2022;22(1):e572. [5] CABLE J, FUCHS E, WEISSMAN I, et al. Adult stem cells and regenerative medicine-a symposium report. Ann N Y Acad Sci. 2020;1462(1):27-36. [6] DENG S, ZHOU X, GE Z, et al. Exosomes from adipose-derived mesenchymal stem cells ameliorate cardiac damage after myocardial infarction by activating S1P/SK1/S1PR1 signaling and promoting macrophage M2 polarization. Int J Biochem Cell Biol. 2019;114:105-114. [7] YANG K, SONG HF, HE S, et al. Effect of neuron-derived neurotrophic factor on rejuvenation of human adipose-derived stem cells for cardiac repair after myocardial infarction. J Cell Mol Med. 2019;23(9):5981-5993. [8] AL-GHADBAN S, BUNNELL BA. Adipose tissue-derived stem cells: immunomodulatory effects and therapeutic potential. Physiology (Bethesda). 2020;35(2):125-133. [9] PARIZADEH SM, JAFARZADEH-ESFEHANI R, GHANDEHARI M, et al. Stem cell therapy: a novel approach for myocardial infarction. J Cell Physiol. 2019;234(10):16904-16912. [10] 孙维兴,赵永超,赵然尊.间充质干细胞移植治疗心肌梗死:问题、症结及新突破[J].中国组织工程研究,2021,25(19): 3103-3109. [11] 姜俣,钱海燕.间充质干细胞治疗心肌梗死的研究进展[J].基础医学与临床, 2023,43(1):21-29. [12] 黄宏,邱伟,陈民佳,等.干细胞预处理及其保护机制的研究进展[J].中华损伤与修复杂志(电子版),2017,12(2):138-142. [13] DROWLEY L, OKADA M, BECKMAN S, et al. Cellular antioxidant levels influence muscle stem cell therapy. Mol Ther. 2010;18(10):1865-1873. [14] YOKOYAMA R, II M, MASUDA M, et al. Cardiac regeneration by statin-polymer nanoparticle-loaded adipose-derived stem cell therapy in myocardial infarction. Stem Cells Transl Med. 2019;8(10):1055-1067. [15] QIN Y, KUMAR BUNDHUN P, YUAN ZL, et al. The effect of high-intensity interval training on exercise capacity in post-myocardial infarction patients: a systematic review and meta-analysis. Eur J Prev Cardiol. 2022;29(3):475-484. [16] COLLET BC, DAVIS DR. Mechanisms of cardiac repair in cell therapy. Heart Lung Circ. 2023;32(7):825-835. [17] 张敏,娄国,付常喜.有氧运动预适应改善骨髓间充质干细胞治疗急性心肌梗死的效果[J].中国组织工程研究,2024,28(25):3988-3993. [18] GUO Y, LI Q, XUAN YT, et al. Exercise-induced late preconditioning in mice is triggered by eNOS-dependent generation of nitric oxide and activation of PKCε and is mediated by increased iNOS activity. Int J Cardiol. 2021;340:68-78. [19] LIAO Z, LI D, CHEN Y, et al. Early moderate exercise benefits myocardial infarction healing via improvement of inflammation and ventricular remodelling in rats. J Cell Mol Med. 2019;23(12):8328-8342. [20] MOAZZAMI K, LIMA BB, HAMMADAH M, et al. Association between change in circulating progenitor cells during exercise stress and risk of adverse cardiovascular events in patients with coronary artery disease. JAMA Cardiol. 2020;5(2):147-155. [21] COSMO S, FRANCISCO JC, CUNHA RC, et al. Effect of exercise associated with stem cell transplantation on ventricular function in rats after acute myocardial infarction. Rev Bras Cir Cardiovasc. 2012;27(4):542-551. [22] CHIRICO EN, DING D, MUTHUKUMARAN G, et al. Acute aerobic exercise increases exogenously infused bone marrow cell retention in the heart. Physiol Rep. 2015;3(10): e12566. [23] QUINDRY JC, FRANKLIN BA. Exercise preconditioning as a cardioprotective phenotype. Am J Cardiol. 2021;148:8-15. [24] 陈天然,潘珊珊.运动预适应:心脏康复预防与治疗的新策略[J].上海体育学院学报,2021,45(10):72-80. [25] NAKAMUTA JS, DANOVIZ ME, MARQUES FL, et al. Cell therapy attenuates cardiac dysfunction post myocardial infarction: effect of timing, routes of injection and a fibrin scaffold. PLoS One. 2009;4(6):e6005. [26] DOS SANTOS L, SANTOS AA, GONÇALVES GA, et al. Bone marrow cell therapy prevents infarct expansion and improves border zone remodeling after coronary occlusion in rats. Int J Cardiol. 2010;145(1):34-39. [27] 娄国,张艳,付常喜.内皮型一氧化氮合酶在运动预适应改善心肌缺血-再灌注损伤中的作用[J].中国组织工程研究,2024,28(8):1283-1288. [28] JI Z, WANG C, TONG Q. Role of miRNA-324-5p-modified adipose-derived stem cells in post-myocardial infarction repair. Int J Stem Cells. 2021;14(3): 298-309. [29] AN J, DU Y, LI X, et al. Myocardial protective effect of sacubitril-valsartan on rats with acute myocardial infarction. Perfusion. 2022;37(2):208-215. [30] SU HL, QIAN YQ, WEI ZR, et al. Real-time myocardial contrast echocardiography in rat: infusion versus bolus administration. Ultrasound Med Biol. 2009;35(5):748-755. [31] WU X, REBOLL MR, KORF-KLINGEBIEL M, et al. Angiogenesis after acute myocardial infarction. Cardiovasc Res. 2021;117(5):1257-1273. [32] LI J, ZHAO Y, ZHU W. Targeting angiogenesis in myocardial infarction: Novel therapeutics (Review). Exp Ther Med. 2022;23(1):e64. [33] LALU MM, MAZZARELLO S, ZLEPNIG J, et al. Safety and efficacy of adult stem cell therapy for acute myocardial infarction and ischemic heart failure (safecell heart): A systematic review and meta-analysis. Stem Cells Transl Med. 2018;7(12):857-866. [34] CLAVELLINA D, BALKAN W, HARE JM. Stem cell therapy for acute myocardial infarction: Mesenchymal stem cells and induced pluripotent stem cells. Expert Opin Biol Ther. 2023;23(10):951-967. [35] SHINMURA D, TOGASHI I, MIYOSHI S, et al. Pretreatment of human mesenchymal stem cells with pioglitazone improved efficiency of cardiomyogenic transdifferentiation and cardiac function. Stem Cells. 2011;29(2):357-366. [36] KHAN M, MEDURU S, MOHAN IK, et al. Hyperbaric oxygenation enhances transplanted cell graft and functional recovery in the infarct heart. J Mol Cell Cardiol. 2009;47(2):275-287. [37] TANG JM, WANG JN, ZHANG L, et al. VEGF/SDF-1 promotes cardiac stem cell mobilization and myocardial repair in the infarcted heart. Cardiovasc Res. 2011;91(3):402-411. [38] RETUERTO MA, BECKMANN JT, CARBRAY J, et al. Angiogenic pretreatment to enhance myocardial function after cellular cardiomyoplasty with skeletal myoblasts. J Thorac Cardiovasc Surg. 2007;133(2):478-484. [39] ALBAENI A, DAVIS JW, AHMAD M. Echocardiographic evaluation of the Athlete’s heart. Echocardiography. 2021;38(6):1002-1016. [40] 朱政,付常喜,马文超,等.有氧运动调控自发性高血压模型大鼠心脏重塑的机制[J].中国组织工程研究,2022,26(14):2231-2237. [41] GHAFOURI-FARD S, KHANBABAPOUR SASI A, HUSSEN BM, et al. Interplay between PI3K/AKT pathway and heart disorders. Mol Biol Rep. 2022;49(10):9767-9781. [42] XIANG FL, LU X, LIU Y, et al. Cardiomyocyte-specific overexpression of human stem cell factor protects against myocardial ischemia and reperfusion injury. Int J Cardiol. 2013;168(4):3486-3494. [43] BRAILE M, MARCELLA S, CRISTINZIANO L, et al. VEGF-A in cardiomyocytes and heart diseases. Int J Mol Sci. 2020;21(15):e5294. [44] ZHOU C, KUANG Y, LI Q, et al. Endothelial S1pr2 regulates post-ischemic angiogenesis via Akt/eNOS signaling pathway. Theranostics. 2022;12(11):5172-5188. [45] WANG N, ZHANG C, XU Y, et al. Berberine improves insulin-induced diabetic retinopathy through exclusively suppressing Akt/mTOR-mediated HIF-1α/VEGF activation in retina endothelial cells. Int J Biol Sci. 2021;17(15):4316-4326. [46] AZIZ NS, YUSOP N, AHMAD A. Importance of stem cell migration and angiogenesis study for regenerative cell-based therapy: A review. Curr Stem Cell Res Ther. 2020;15(3):284-299. [47] ZHAO T, ZHAO W, CHEN Y, et al. Differential expression of vascular endothelial growth factor isoforms and receptor subtypes in the infarcted heart. Int J Cardiol. 2013;167(6):2638-2645. [48] WANG HJ, RAN HF, YIN Y, et al. Catalpol improves impaired neurovascular unit in ischemic stroke rats via enhancing VEGF-PI3K/Akt and VEGF-MEK1/2/ERK1/2 signaling. Acta Pharmacol Sin. 2022;43(7):1670-1685. [49] SHIBUYA M. VEGF-VEGFR system as a target for suppressing inflammation and other diseases. Endocr Metab Immune Disord Drug Targets. 2015;15(2):135-144. [50] XU X, YE X, ZHU M, et al. FtMt reduces oxidative stress-induced trophoblast cell dysfunction via the HIF-1α/VEGF signaling pathway. BMC Pregnancy Childbirth. 2023;23(1):e131. |
| [1] | Li Zikai, Zhang Chengcheng, Xiong Jiaying, Yang Xirui, Yang Jing, Shi Haishan. Potential effects of ornidazole on intracanal vascularization in endodontic regeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(在线): 1-7. |
| [2] | Gao Yang, Qin Hewei, Liu Dandan. ACSL4 mediates ferroptosis and its potential role in atherosclerotic cardiovascular disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1239-1247. |
| [3] | Han Haihui, Meng Xiaohu, Xu Bo, Ran Le, Shi Qi, Xiao Lianbo. Effect of fibroblast growth factor receptor 1 inhibitor on bone destruction in rats with collagen-induced arthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 968-977. |
| [4] | Li Tingyue, Guo Qian, He Wenxi, Wu Jiayuan. Long noncoding RNA TP53TG1 promotes odontogenic and osteogenic differentiation of stem cells from the apical papilla [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7776-7782. |
| [5] | Li Zhe, Li Ping, Zhang Chao, Guo Guangling. A network meta-analysis of efficacy of mesenchymal stem cells from different sources in treatment of premature ovarian failure animal models [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7898-7908. |
| [6] | Yang Dingyan, Yu Zhenqiu, Yang Zhongyu. Machine learning-based analysis of neutrophil-associated potential biomarkers for acute myocardial infarction [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7909-7920. |
| [7] | Fang Yuan, Qian Zhiyong, He Yuanhada, Wang Haiyan, Sha Lirong, Li Xiaohe, Liu Jing, He Yachao, Zhang Kai, Temribagen. Mechanism of Mongolian medicine Echinops sphaerocephalus L. in proliferation and angiogenesis of vascular endothelial cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7519-7528. |
| [8] | Zhao Jianwei, Li Xunsheng, Lyu Jinpeng, Zhou Jue, Jiang Yidi, Yue Zhigang, Sun Hongmei. Deer antler stem cell exosome composite hydrogel promotes the repair of burned skin [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7344-7352. |
| [9] | Pan Chun, Fan Zhencheng, Hong Runyang, Shi Yujie, Chen Hao. Effect and mechanism of polystyrene microplastics on prostate in male mice [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7353-7361. |
| [10] | Wu Qingyun, Su Qiang. Antioxidant nanomedicine-mediated targeted therapy for myocardial ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7431-7438. |
| [11] | Tian Yushi, Fu Qiang, Li Ji . Bioinformatics identification and validation of mitochondrial genes related to acute myocardial infarction [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(31): 6697-6707. |
| [12] | Zeng Yu, Xie Chengwei, Hong Yuanqi, Su Shenghui, Dong Xieping. In vitro angiogenesis and osteogenesis properties of copper-doped mesoporous bioactive glass [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(28): 5941-5949. |
| [13] | Li Zeming, Zhang Yuntao, Wang Maolin, Hou Yudong. Role and mechanism of hypoxia-inducible factor 1 alpha regulating bone homeostasis in oral and maxillofacial diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(26): 5680-5687. |
| [14] | Wang Lei, Wang Baiyan, Zhou Chunguang, Ren Xiaoyun, Dai Yueyou, Feng Shuying. Role of different cell-derived exosomal miRNAs in progression, diagnosis, and prognosis of gastric cancer [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(25): 5434-5442. |
| [15] | Feng Qiang, Pi Yihua, Huang Huasheng, Huang Delun, Zhang Yan. Bone marrow mesenchymal stem cell transplantation for myocardial infarction in rats: effects of acute and chronic exercises [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(23): 4868-4877. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||