Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (14): 2133-2139.doi: 10.12307/2024.233
Biomechanical characteristics of orthodontic tooth movement before and after increasing alveolar bone mass with periodontally accelerated osteogenic orthodontics
Zhao Hexiang, Chen Ziyan, Wang Jing, Ge Zhenlin
- Department of Orthodontics, School of Stomatology, Lanzhou University, Lanzhou 730000, Guansu Province, China
-
Received:2023-02-17Accepted:2023-03-16Online:2024-05-18Published:2023-07-28 -
Contact:Ge Zhenlin, Professor, Department of Orthodontics, School of Stomatology, Lanzhou University, Lanzhou 730000, Guansu Province, China -
About author:Zhao Hexiang, Master candidate, Department of Orthodontics, School of Stomatology, Lanzhou University, Lanzhou 730000, Guansu Province, China
CLC Number:
Cite this article
Zhao Hexiang, Chen Ziyan, Wang Jing, Ge Zhenlin. Biomechanical characteristics of orthodontic tooth movement before and after increasing alveolar bone mass with periodontally accelerated osteogenic orthodontics[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(14): 2133-2139.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
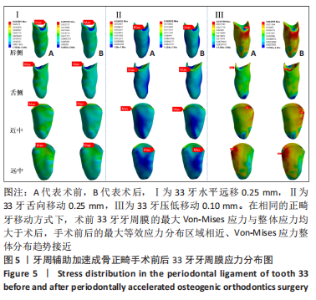
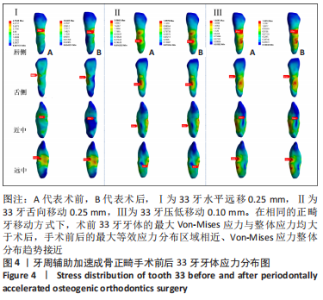
在实验Ⅰ中,33牙远中向移动0.25 mm,模型A中 33牙牙体最大Von-Mises应力值出现于33牙牙根远中面颈缘近唇侧1/3处,最大等效应力值为4.734 3 MPa;模型B中33牙牙体最大Von-Mises应力值也集中于33牙牙根远中面颈缘近唇侧1/3处,最大等效应力值为2.640 2 MPa;两者相比,模型A中33牙牙体整体应力较模型B大,两者的Von-Mises应力分布趋势接近。 在实验Ⅱ中,33牙舌向移动0.25 mm,模型A中33牙牙体的最大应力值出现于33牙牙根舌面颈1/3到中1/3,最大等效应力值为2.086 8 MPa;模型B中33牙牙体最大Von-Mises应力值也集中于33牙牙根舌面颈1/3到中1/3处,最大等效应力值为1.257 9 MPa;两者相比,模型A中33牙牙体整体应力较模型B大,两者的Von-Mises应力分布趋势接近。 在实验Ⅲ中,33牙压低移动0.10 mm,模型A中33牙牙体的最大应力值出现于33牙牙根唇侧颈1/3到中1/3区域,以及舌侧中1/3区域,最大等效应力值为1.869 5 MPa;模型B中33牙牙体最大Von-Mises应力值也出现于33牙牙根唇侧颈1/3到中1/3区域,以及舌侧中1/3区域,最大等效应力值为1.381 8 MPa;两者相比,模型A中33牙牙体整体应力较模型B大,两者的Von-Mises应力分布趋势接近。 2.2 各组模型牙周膜应力分布 在不同的正畸牙移动方式下,各组模型33牙牙周膜的Von-Mises应力分布见图5所示。"
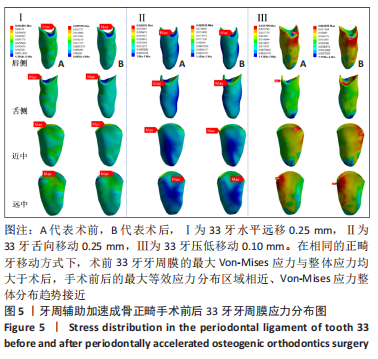

在实验Ⅰ中,33牙远中向移动0.25 mm,模型A中33牙牙周膜的最大Von-Mises应力值集中于牙周膜远中侧颈缘中1/3区域,最大等效应力值为0.046 4 MPa,33牙大面积牙周膜等效应力集中在0.010 3-0.025 8 MPa;模型B中牙周膜的最大Von-Mises应力值集中于牙周膜远中侧颈缘中1/3区域,最大等效应力值为0.025 6 MPa,33牙大面积牙周膜等效应力集中在0.005 7-0.017 1 MPa;模型A中33牙牙周膜整体应力大于模型B,两者牙周膜Von-Mises应力分布趋势接近。 在实验Ⅱ中,33牙舌向移动0.25 mm,模型A中33牙牙周膜的最大Von-Mises应力值集中于牙周膜舌侧颈缘远中区域,最大等效应力值为0.036 8 MPa,33牙大面积牙周膜等效应力集中在0.004 1-0.016 4 MPa;模型B中33牙牙周膜的最大Von-Mises应力值集中于牙周膜舌侧颈缘远中区域,最大等效应力值为0.020 3 MPa,33牙大面积牙周膜等效应力集中在0.002 3-0.009 0 MPa;模型A中33牙牙周膜整体应力较模型B大,两者牙周膜Von-Mises应力分布趋势接近。 在实验Ⅲ中,33牙压低移动0.10 mm,模型A中33牙牙周膜的最大Von-Mises应力值集中于牙周膜唇侧颈缘远中1/3区域,最大等效应力值为0.035 7 MPa,33牙大面积牙周膜等效应力集中在0.011 9-0.023 8 MPa;模型B中33牙牙周膜的最大Von-Mises应力值集中于牙周膜唇侧颈缘中1/3区域,最大等效应力值为0.024 3 MPa,33牙大面积牙周膜等效应力集中在0.008 1-0.016 2 MPa;模型A中33牙牙周膜整体应力较模型B大,两者牙周膜Von-Mises应力分布趋势接近。 2.3 各组模型牙槽骨应力分布 在不同的正畸牙移动方式下,各组模型33牙周围牙槽骨的Von-Mises应力分布见图6所示,同时为了更好地观察两组模型中33牙唇侧牙槽骨的应力情况,将33牙牙槽窝沿冠状向分开,以便对比分析其应力状况,见图7。"

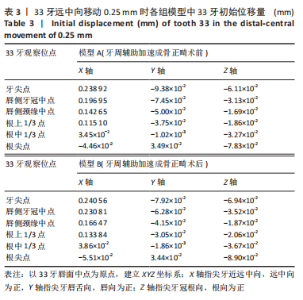
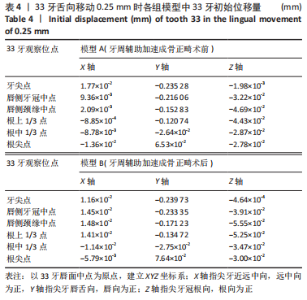
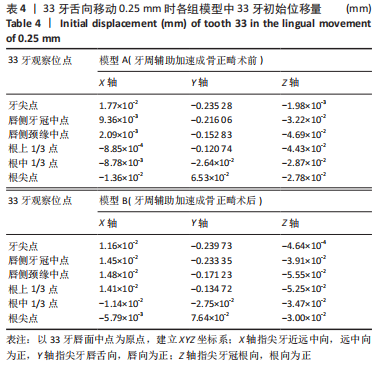
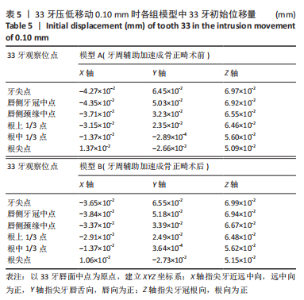
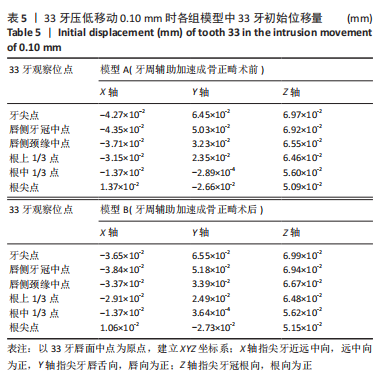
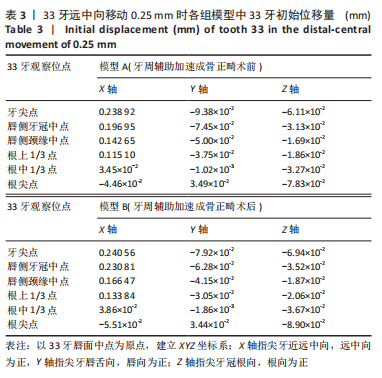
在实验Ⅰ中,33牙远中向移动0.25 mm,模型A和模型B中33牙周围牙槽骨的最大Von-Mises应力值均集中于33牙唇侧牙槽嵴顶中1/3区域,模型A中最大等效应力值为11.329 MPa,大于模型B最大等效应力值3.625 MPa;两组模型等效应力分布均呈现牙槽嵴顶处向根方逐步减小;对比A、B两组模型,模型A中33牙周围牙槽骨整体应力较模型B大。 在实验Ⅱ中,33牙舌向移动0.25 mm,模型A中33牙周围牙槽骨的最大Von-Mises应力值集中于33牙唇侧牙槽嵴顶中1/3区域,最大等效应力值为11.329 MPa;与模型A不同,模型B中33牙周围牙槽骨的最大Von-Mises应力值集中于33牙舌侧牙槽嵴顶中、远1/3交界区域,最大等效应力值为3.625 MPa,小于模型A;两组模型等效应力分布均呈现牙槽嵴顶处向根方逐步减小;对比A、B两组模型,模型A中33牙周围牙槽骨整体应力较模型B大。 在实验Ⅲ中,33牙压低移动0.10 mm,模型A中33牙周围牙槽骨的最大Von-Mises应力值集中于33牙唇侧牙槽嵴顶中1/3区域,最大等效应力值为1.948 MPa;与模型A不同,模型B中33牙周围牙槽骨的最大Von-Mises应力值集中于33牙舌侧牙槽嵴顶中1/3区域,最大等效应力值为0.807 MPa,小于模型A;两组模型等效应力分布均呈现牙槽嵴顶处向根方逐步减小;对比A、B两组模型,模型A中33牙周围牙槽骨整体应力较模型B大。 2.4 各组模型33牙初始位移分析 在实验Ⅰ中,33牙的6个观察位点在X轴、Y轴、Z轴上的初始位移量见表3,分析33牙的初始位移趋势可见,模型A与模型B牙齿移动趋势一致,33牙均表现为远中倾斜移动,并有少量舌向移动趋势,但模型B的初始位移量大于模型A。"
| [1] ANTOUN J S, MEI L, GIBBS K, et al. Effect of orthodontic treatment on the periodontal tissues. Periodontology 2000. 2017;74(1):140-157. [2] ALSINO HI, HAJEER MY, BURHAN AS, et al. The Effectiveness of Periodontally Accelerated Osteogenic Orthodontics (PAOO) in Accelerating Tooth Movement and Supporting Alveolar Bone Thickness During Orthodontic Treatment: A Systematic Review. Cureus. 2022; 14(5):e24985. [3] KAMAL A T, MALIK D, FIDA M, et al. Does periodontally accelerated osteogenic orthodontics improve orthodontic treatment outcome? A systematic review and meta-analysis. Int Orthod. 2019;17(2):193-201. [4] DOUNIS T, PITMAN LM. Decision Making for Soft and Hard Tissue Augmentation in Surgically Facilitated Orthodontics. Clin Adv Periodontics. 2020;10(1):38-41. [5] BRUGNAMI F, CAIAZZO A, MEHRA P. Can corticotomy (with or without bone grafting) expand the limits of safe orthodontic therapy? J Oral Biol Craniofac Res. 2018;8(1):1-6. [6] XU X, WU JQ, JIANG JH, et al. Periodontal Effect of Periodontally Accelerated Osteogenic Orthodontics in Skeletal Angle Class III: A Nonrandomized, Controlled Trial. Int J Periodontics Restorative Dent. 2020;40(4):e169-e177. [7] KESER E, NAINI FB. Accelerated orthodontic tooth movement: surgical techniques and the regional acceleratory phenomenon. Maxillofac Plast Reconstr Surg. 2022;44(1):1. [8] AMIT G, JPS K, PANKAJ B, et al. Periodontally accelerated osteogenic orthodontics (PAOO) - a review. J Clin Exp Dent. 2012;4(5):e292-e296. [9] VANNALA V, KATTA A, REDDY MS, et al. Periodontal Accelerated Osteogenic Orthodontics Technique for Rapid Orthodontic Tooth Movement: A Systematic Review. J Pharm Bioallied Sci. 2019;11(Suppl 2): S97-S106. [10] XUAN DY. [Strategies of periodontal surgery to promote orthodontic treatment: the clinical application of periodontally accelerated osteogenic orthodontics]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2020; 55(7):448-454. [11] Van BILSEN MW, SCHREURS R, MEULSTEE JW, et al. Evaluation of the anterior mandibular donor site one year after secondary reconstruction of an alveolar cleft: 3-dimensional analysis using cone-beam computed tomography. Br J Oral Maxillofac Surg. 2015;53(8): 719-724. [12] 雍苓,黄仕禄,刘洪,等.不同骨缺损类型牙种植体的三维有限元分析[J].医用生物力学,2016,31(2):148-153. [13] GOMEZ JP, PEÑA FM, MARTÍNEZ V, et al. Initial force systems during bodily tooth movement with plastic aligners and composite attachments: A three-dimensional finite element analysis. Angle Orthod. 2015;85(3):454-460. [14] LIANG W, RONG Q, LIN J, et al. Torque control of the maxillary incisors in lingual and labial orthodontics: a 3-dimensional finite element analysis. Am J Orthod Dentofacial Orthop. 2009;135(3):316-322. [15] JIANG T, WU RY, WANG JK, et al. Clear aligners for maxillary anterior en masse retraction: a 3D finite element study. Sci Rep. 2020;10(1): 10156. [16] 刘倩,顾泽旭,田杰,等.材料厚度对无托槽隐形矫治器固位力影响的实验研究[J].中华口腔正畸学杂志,2013,20(1):46-48. [17] HONG K, KIM WH, EGHAN-ACQUAH E, et al. Efficient Design of a Clear Aligner Attachment to Induce Bodily Tooth Movement in Orthodontic Treatment Using Finite Element Analysis. Materials (Basel). 2021;14(17):4926. [18] LIU L, SONG Q, ZHOU J, et al. The effects of aligner overtreatment on torque control and intrusion of incisors for anterior retraction with clear aligners: A finite-element study. Am J Orthod Dentofacial Orthop. 2022;162(1):33-41. [19] WILCKO WM, WILCKO T, BOUQUOT JE, et al. Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int J Periodontics Restorative Dent. 2001;21(1):9-19. [20] DARWICHE F, KHODARI E, ALJEHANI D, et al. Comparison of Effectiveness of Corticotomy-assisted Accelerated Orthodontic Treatment and Conventional Orthodontic Treatment: A Systematic Review. J Contemp Dent Pract. 2020;21(6):701-709. [21] CHEN Z, ZHOU H, ZHANG K, et al. The clinical efficacy of periodontally accelerated osteogenic orthodontics in patients with bone fenestration and dehiscence: a retrospective study. Head Face Med. 2022;18(1):40. [22] HAN Y, MIAO L, LIU J, et al. Periodontal soft tissue increase induced by periodontally accelerated osteogenic orthodontics surgery. BMC Oral Health. 2022;22(1):506. [23] MUÑOZ F, WILCKO T, ACUÑA S, et al. Periodontally Accelerated Osteogenic Orthodontics (PAOO) technique in cleft patients: A complement to orthognathic surgery in dentoalveolar expansion. A case series report. J Craniomaxillofac Surg. 2020;48(11):1028-1034. [24] AGRAWAL AA, KOLTE AP, KOLTE RA, et al. Comparative CBCT analysis of the changes in buccal bone morphology after corticotomy and micro-osteoperforations assisted orthodontic treatment - Case series with a split mouth design. Saudi Dent J. 2019;31(1):58-65. [25] BHATTACHARYA P, BHATTACHARYA H, ANJUM A, et al. Assessment of Corticotomy Facilitated Tooth Movement and Changes in Alveolar Bone Thickness - A CT Scan Study. J Clin Diagn Res. 2014;8(10):C26-C30. [26] GAO J, NGUYEN T, OBEROI S, et al. The Significance of Utilizing A Corticotomy on Periodontal and Orthodontic Outcomes: A Systematic Review and Meta-Analysis. Biology (Basel). 2021;10(8):803. [27] WILCKO MT, FERGUSON DJ, MAKKI L, et al. Keratinized Gingiva Height Increases After Alveolar Corticotomy and Augmentation Bone Grafting. J Periodontol. 2015;86(10):1107-1115. [28] WANG Y, ZHANG H, SUN W, et al. Macrophages mediate corticotomy-accelerated orthodontic tooth movement. Sci Rep. 2018;8(1):16788. [29] YASHWANT VA, BALU P, KUMAR RS, et al. Effectiveness of platelet rich fibrin versus demineralized bone xenograft in periodontally accelerated osteogenic orthodontics. Angle Orthod. 2022;92(2):180-188. [30] ZHOU Y, HE X, ZHANG D. Study of bone remodeling in corticotomy-assisted orthodontic tooth movement in rats. J Cell Biochem. 2019; 120(9):15952-15962. [31] XU X, WU JQ, JIANG JH, et al. Periodontal Effect of Periodontally Accelerated Osteogenic Orthodontics in Skeletal Angle Class III: A Nonrandomized, Controlled Trial. Int J Periodontics Restorative Dent. 2020;40(4):e169-e177. [32] MA Z, ZHU Y, ZHAN Y, et al. Periosteum coverage versus collagen-membrane coverage in periodontally accelerated osteogenic orthodontics: a randomized controlled clinical trial in Class II and Class III malocclusions. BMC Oral Health. 2022;22(1):439. [33] JIANG JH. [Application, research and prospect of periodontally accelerated osteogenic orthodontics technology]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2021;56(10):971-977. [34] WANG X, MEI M, HAN G, et al. Effectiveness of modified periodontally accelerated osteogenic orthodontics in skeletal class II malocclusion treated by a camouflage approach. Am J Transl Res. 2022;14(2):979-989. [35] XU M, SUN XY, XU JG. Periodontally accelerated osteogenic orthodontics with platelet-rich fibrin in an adult patient with periodontal disease: A case report and review of literature. World J Clin Cases. 2021;9(6): 1367-1378. [36] LIU X, CHENG Y, QIN W, et al. Effects of upper-molar distalization using clear aligners in combination with Class II elastics: a three-dimensional finite element analysis. BMC Oral Health. 2022;22(1):546. [37] 王荣,刘亦然,范勇斌,等.Bio-oss骨胶原修复牙槽骨缺损区后对牙齿移动影响的临床初探[J].口腔颌面修复学杂志,2012,13(4): 243-245. [38] KESER E, NAINI FB. Accelerated orthodontic tooth movement: surgical techniques and the regional acceleratory phenomenon. Maxillofac Plast Reconstr Surg. 2022;44(1):1. [39] QI L, GE W, CAO N, et al. Effects of autologous concentrated growth factor on gingival thickness in periodontal accelerated osteogenic orthodontics: a 6-month randomized controlled trial. BMC Oral Health. 2021;21(1):604. [40] YANG C, WANG C, DENG F, et al. Biomechanical effects of corticotomy approaches on dentoalveolar structures during canine retraction: A 3-dimensional finite element analysis. Am J Orthod Dentofacial Orthop. 2015;148(3):457-465. |
| [1] | Lu Jieming, Li Yajing, Du Peijie, Xu Dongqing. Effects of artificial turf versus natural grass on biomechanical performance of the lower limbs in young females during jump-landing [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1101-1107. |
| [2] | Su Dejun, Dong Wanpeng, Dong Yuefu, Zhang Jichao, Zhang Zhen. Design of asymmetric prosthesis and mechanical analysis of total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 510-516. |
| [3] | He Kai, Xing Wenhua, Liu Shengxiang, Bai Xianming, Zhou Chen, Gao Xu, Qiao Yu, He Qiang, Gao Zhiyu, Guo Zhen, Bao Aruhan, Li Chade. Constructing a model of degenerative scoliosis using finite element method: biomechanical analysis in etiology and treatment [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 572-578. |
| [4] | Gao Xilin, Wu Si Zhang Chao Zhu Liguo, Fu Bifeng, Wang Ping. Mechanotransduction proteins in intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 579-589. |
| [5] | Wang X, Wang Hm, Chen Sh, Feng Tx, Bu Hm, Zhu Lg, Chen Dd, Wei X. Stress and morphological characteristics of intervertebral foramen of cervical rotation-traction manipulation for treating cervical spondylotic radiculopathy: a three-dimensional finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 441-447. |
| [6] | Zhao Yuxin, Liang Liang, Jin Feng, Xu Yangyang, Kang Zhijie, Fang Yuan, He Yujie, Wang Xing, Wang Haiyan, Li Xiaohe. Establishment and stress analysis of a finite element model for adolescent cervical disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 448-454. |
| [7] | Li Zhenggang, Shang Xuehong, Wu Zhang, Li Hong, Sun Chaojun, Chen Huadong, Sun Zhe, Yang Yi. Finite element analysis of three internal fixation modalities for treatment of Pauwels type III femoral neck fractures under different loading conditions [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 455-463. |
| [8] | Liu Mengfei, Chen Gang, Shi Yihan, Zeng Lin, Jiang Kan, Yilihamujiang•Wusiman. Finite element analysis of optimization of femoral prosthesis implantation position in unicompartmental knee arthroplasty in osteoporotic patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 464-470. |
| [9] | Wang Zilong, Meng Xin, Zhang Zhiqi, Xie Yu, Meng Lingyue, Zhang Qiuxia, Kong Lingyu. Biomechanical characteristics of lower extremities during counter movement jump in male patients with functional ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 478-485. |
| [10] | Liang Jiyao, Zhou Honghai, Wei Guikang, Su Shaoting, Chen Longhao, He Xinyu, Liu Liangpu. Quantification of in vivo biomechanics and analysis of influencing factors in cervical spine fixed-point rotation manipulation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 486-492. |
| [11] | Li Zhifei, Yang Yin, Chen Hualong, Liang Qinqiu, Zhong Yuanming, Zhang Yisheng. Finite element analysis of the correlation between tilt angle of titanium cage and postoperative subsidence of titanium cage after anterior subtotal cervical corpectomy, decompression and fusion [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1313-1319. |
| [12] | Chen Mengmeng, Bao Li, Chen Hao, Jia Pu, Feng Fei, Shi Guan, Tang Hai. Biomechanical characteristics of a novel interspinous distraction fusion device BacFuse for the repair of lumbar degenerative disease [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1325-1329. |
| [13] | Liang Cheng, Zhang Linqi, Wang Guan, Li Wen, Duan Ke, Li Zhong, Lu Xiaobo, Zhuo Naiqiang. Finite element and biomechanical analysis of different implants in repair for unilateral unstable pelvic posterior ring injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1336-1341. |
| [14] | Yang Junliang, Lu Tan, Xu Biao, Jiang Yaqiong, Wang Fucheng. Three-dimensional finite element analysis of effects of partial anterior cruciate ligament rupture on knee joint stress [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1347-1353. |
| [15] | Weng Rui, Lin Dongxin, Guo Haiwei, Zhang Wensheng, Song Yuke, Lin Hongheng, Li Wenchao, Ye Linqiang. Abnormal types of intervertebral disc structure and related mechanical loading with biomechanical factors [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1436-1442. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||