Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (6): 833-839.doi: 10.12307/2023.779
Previous Articles Next Articles
Effects of endoscopic foraminoplasty and laminoplasty on biomechanical properties of intervertebral disc and isthmus
Zhang Rui1, 2, Wang Kun1, 2, Shen Zicong1, Mao Lu1, 2, Wu Xiaotao1, 2
- 1School of Medicine, Southeast University, Nanjing 210009, Jiangsu Province, China; 2Department of Orthopedics, Zhongda Hospital, Southeast University, Nanjing 210009, Jiangsu Province, China
-
Received:2022-11-18Accepted:2023-01-04Online:2024-02-28Published:2023-07-11 -
Contact:Wu Xiaotao, MD, Professor, Chief physician, School of Medicine, Southeast University, Nanjing 210009, Jiangsu Province, China; Department of Orthopedics, Zhongda Hospital, Southeast University, Nanjing 210009, Jiangsu Province, China Mao Lu, MD, Associate chief physician, School of Medicine, Southeast University, Nanjing 210009, Jiangsu Province, China; Department of Orthopedics, Zhongda Hospital, Southeast University, Nanjing 210009, Jiangsu Province, China -
About author:Zhang Rui, Master candidate, School of Medicine, Southeast University, Nanjing 210009, Jiangsu Province, China; Department of Orthopedics, Zhongda Hospital, Southeast University, Nanjing 210009, Jiangsu Province, China Wang Kun, MD, Attending physician, School of Medicine, Southeast University, Nanjing 210009, Jiangsu Province, China; Department of Orthopedics, Zhongda Hospital, Southeast University, Nanjing 210009, Jiangsu Province, China
CLC Number:
Cite this article
Zhang Rui, Wang Kun, Shen Zicong, Mao Lu, Wu Xiaotao. Effects of endoscopic foraminoplasty and laminoplasty on biomechanical properties of intervertebral disc and isthmus[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 833-839.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
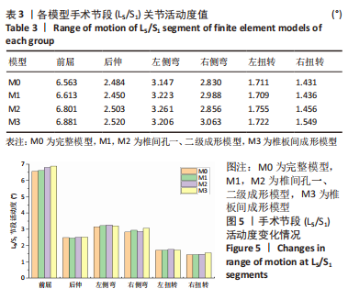
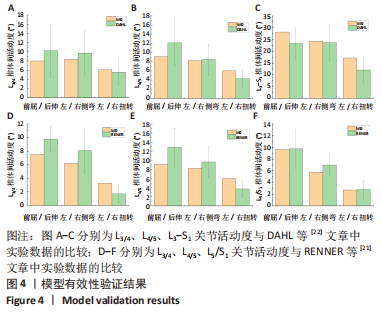
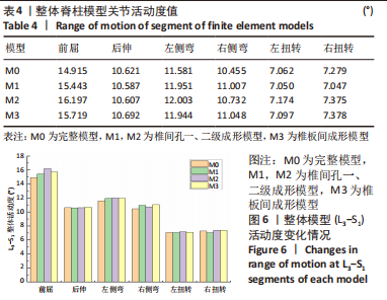
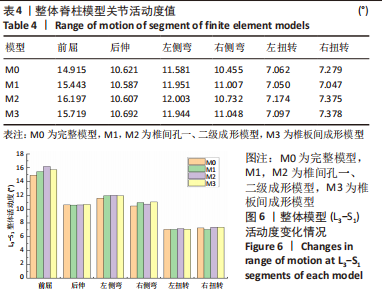
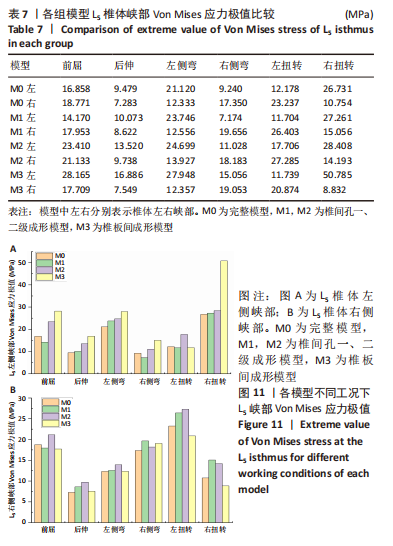
2.2 各组模型手术节段(L5/S1)和整体脊柱模型关节活动度值比较 在400 N垂直向下力和8 N?m力矩载荷下,由表3和图5可观察到,在手术节段(L5/S1)关节处,椎间孔一级成形模型M1在前屈、后伸、左侧弯、右侧弯、左扭转和右扭转工况下的L5/S1段关节活动度均值较模型M0分别增加了0.76%,-1.39%,2.41%,3.80%,-0.08%,0.36%;椎间孔二级成形模型M2在前屈、后伸、左侧弯、右侧弯、左扭转和右扭转工况下的L5/S1段关节活动度均值较模型M0分别增加了3.63%,-0.76%,3.61%,0.90%,2.62%,1.73%,椎板间成形模型M3在前屈、后伸、左侧弯、右侧弯、左扭转和右扭转工况下较模型M0分别增加4.84%,1.44%,1.86%,8.23%,0.64%,8.26%。"
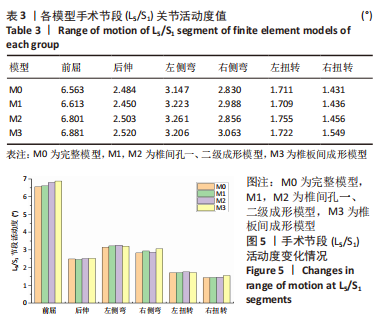
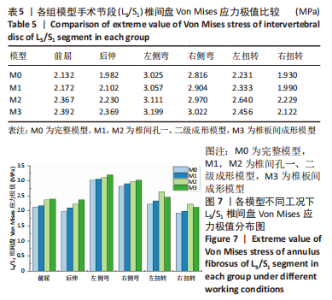
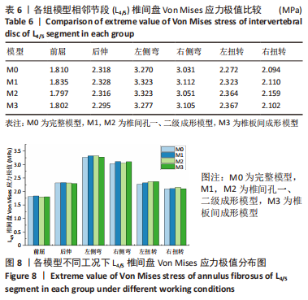
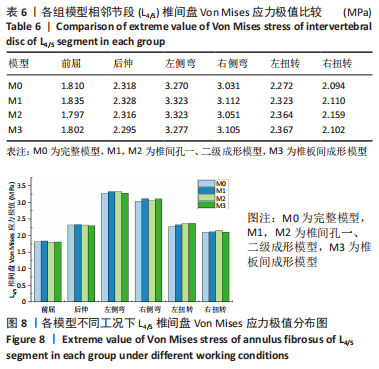
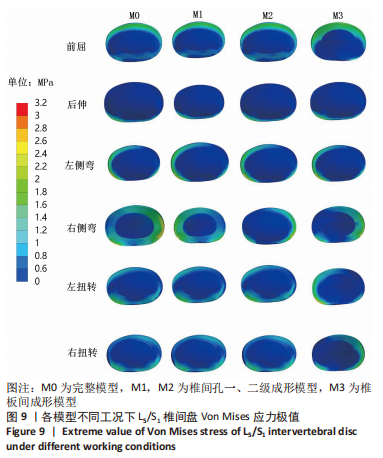
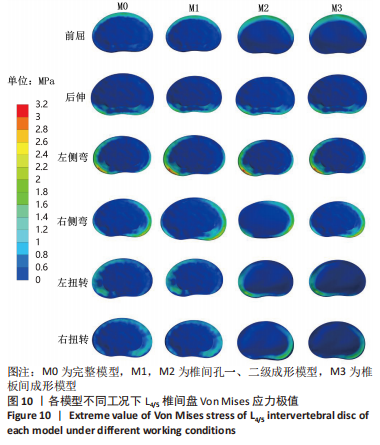
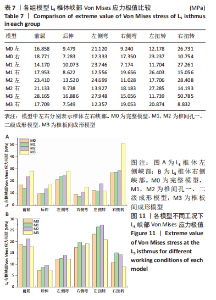
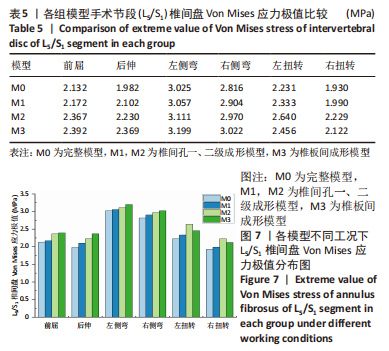
一级椎间孔成形术对脊柱手术节段和整体脊柱的活动度变化影响较小,活动度变化百分比均低于5%;二级椎间孔成形在手术节段活动度变化不明显,整体活动度在前屈时轻度增加;椎板间成形术的手术节段右侧弯和右扭转的活动度轻度增加,整体模型关节活动度在前屈和右侧弯时轻度增加,整体腰骶模型及各节段之间维持稳定状态。 2.3 各组模型手术节段(L5/S1)椎间盘和相邻节段(L4/5)椎间盘Von Mises 应力极值比较 由表5和图7可见,在手术节段(L5/S1),椎间孔一、二级成形模型M1和M2中椎间盘Von Mises 应力极值在前屈、后伸、左侧弯、右侧弯、左扭转和右扭转时分别较M0模型增加1.88%,6.06%,1.07%,3.14%,4.57%,3.13%和11.06%,12.50%,2.84%,5.50%,18.32%,15.48%;椎板间成形模型M3在前屈、后伸、左侧弯、右侧弯、左扭转和右扭转时分别较M0模型增加12.22%,19.54%,5.75%,7.34%,10.05%,9.97%。"
| [1] GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; 388(10053):1545-1602. [2] HARTVIGSEN J, HANCOCK MJ, KONGSTED A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356-2367. [3] WEBER H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976). 1983;8(2):131-140. [4] BENOIST M. The natural history of lumbar disc herniation and radiculopathy. Joint Bone Spine. 2002;69(2):155-160. [5] DEYO RA, MIRZA SK. CLINICAL PRACTICE. Herniated Lumbar Intervertebral Disk. N Engl J Med. 2016;374(18):1763-1772. [6] CHEN BL, GUO JB, ZHANG HW, et al. Surgical versus non-operative treatment for lumbar disc herniation: a systematic review and meta-analysis. Clin Rehabil. 2018;32(2):146-160. [7] KAMBIN P, SAMPSON S. Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results. Clin Orthop Relat Res. 1986;(207):37-43. [8] KAMBIN P. Arthroscopic microdiskectomy. Mt Sinai J Med. 1991;58(2): 159-164. [9] YEUNG AT. Minimally Invasive Disc Surgery with the Yeung Endoscopic Spine System (YESS). Surg Technol Int. 1999;8:267-277. [10] HOOGLAND T, SCHUBERT M, MIKLITZ B, et al. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976). 2006;31(24):E890-E897. [11] 李长青,周跃,王建,等.经皮椎间孔内窥镜下靶向穿刺椎间盘切除术治疗腰椎间盘突出症[J].中国脊柱脊髓杂志,2013,23(3):193-197. [12] 张西峰,张琳.脊柱内镜技术的历史、现状与发展[J].中国疼痛医学杂志,2015,21(2):81-85. [13] 李振宙,吴闻文,侯树勋,等.经皮腰椎间孔成形内窥镜下椎间盘切除术治疗腰椎间盘突出症的疗效观察[J].中国脊柱脊髓杂志, 2008,18(10): 752-756+801. [14] LI ZZ, HOU SX, SHANG WL, et al. Percutaneous lumbar foraminoplasty and percutaneous endoscopic lumbar decompression for lateral recess stenosis through transforaminal approach: Technique notes and 2 years follow-up. Clin Neurol Neurosurg. 2016;143:90-94. [15] 蓝彬,柳达,周广平,等.腰椎间孔成形技术在脊柱内镜手术应用中的研究进展[J].实用骨科杂志,2018,24(5):434-437. [16] NIE H, ZENG J, SONG Y, et al. Percutaneous Endoscopic Lumbar Discectomy for L5-S1 Disc Herniation Via an Interlaminar Approach Versus a Transforaminal Approach: A Prospective Randomized Controlled Study With 2-Year Follow Up. Spine (Phila Pa 1976). 2016; 41 Suppl 19:B30-B37. [17] CHOI KC, KIM JS, RYU KS, et al. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: transforaminal versus interlaminar approach. Pain Physician. 2013;16(6):547-556. [18] CHOI G, LEE SH, RAITURKER PP, et al. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery. 2006;58(1 Suppl):ONS59-68; discussion ONS59-68. [19] CHEN KT, JABRI H, LOKANATH YK, et al. The evolution of interlaminar endoscopic spine surgery. J Spine Surg. 2020;6(2):502-512. [20] CAO L, LIU Y, MEI W, et al. Biomechanical changes of degenerated adjacent segment and intact lumbar spine after lumbosacral topping-off surgery: a three-dimensional finite element analysis. BMC Musculoskelet Disord. 2020;21(1):104. [21] RENNER SM, NATARAJAN RN, PATWARDHAN AG, et al. Novel model to analyze the effect of a large compressive follower pre-load on range of motions in a lumbar spine. J Biomech. 2007;40(6):1326-1332. [22] DAHL MC, ELLINGSON AM, MEHTA HP, et al. The biomechanics of a multilevel lumbar spine hybrid using nucleus replacement in conjunction with fusion. Spine J. 2013;13(2):175-183. [23] SHI Y, XIE YZ, ZHOU Q, et al. The biomechanical effect of the relevant segments after facet-disectomy in different diameters under posterior lumbar percutaneous endoscopes: a three-dimensional finite element analysis. J Orthop Surg Res. 2021;16(1):593. [24] VADAPALLI S, SAIRYO K, GOEL VK, et al. Biomechanical rationale for using polyetheretherketone (PEEK) spacers for lumbar interbody fusion-A finite element study. Spine (Phila Pa 1976). 2006;31(26): E992-E998. [25] 闫家智,吴志宏,汪学松,等.腰椎三维有限元模型建立和应力分析[J].中华医学杂志,2009,89(17):1162-1165. [26] TEZUKA F, SAKAI T, ABE M, et al. Anatomical considerations of the iliac crest on percutaneous endoscopic discectomy using a transforaminal approach. Spine J. 2017;17(12):1875-1880. [27] CHOI KC, PARK CK. Percutaneous Endoscopic Lumbar Discectomy for L5-S1 Disc Herniation: Consideration of the Relation between the Iliac Crest and L5-S1 Disc. Pain Physician. 2016;19(2):E301-E308. [28] WANG Z, CHEN Z, WU H, et al. Treatment of high-iliac-crest L5-S1 lumbar disc herniation via a transverse process endoscopic transforaminal approach. Clin Neurol Neurosurg. 2020;197:106087. [29] CHEN KT, TSENG C, SUN LW, et al. Technical Considerations of Interlaminar Approach for Lumbar Disc Herniation. World Neurosurg. 2021;145:612-620. [30] DENIS F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983; 8(8):817-831. [31] SPINA NT, MORENO GS, BRODKE DS, et al. Biomechanical effects of laminectomies in the human lumbar spine: a finite element study. Spine J. 2021;21(1):150-159. [32] SHIRAZI-ADL A. Finite-element evaluation of contact loads on facets of an L2-L3 lumbar segment in complex loads. Spine (Phila Pa 1976). 1991;16(5):533-541. [33] PAHOLPAK P, DEDEOGULLARI E, LEE C, et al. Do modic changes, disc degeneration, translation and angular motion affect facet osteoarthritis of the lumbar spine. Eur J Radiol. 2018;98:193-199. [34] 余洋,谢一舟,石银,等. 三维有限元法分析腰椎不同尺寸关节突成形后相关节段的生物力学特征[J].中国组织工程研究,2021, 25(33):5288-5293. [35] 张晗硕,丁宇,蒋强,等.脊柱内镜下椎板开窗减压与单侧入路双侧减压治疗腰椎管狭窄症的生物力学稳定性及有限元分析[J].中国组织工程研究,2023,27(13):1981-1986. [36] AOKI Y, TAKAHASHI H, NAKAJIMA A, et al. Prevalence of lumbar spondylolysis and spondylolisthesis in patients with degenerative spinal disease. Sci Rep. 2020;10(1):6739. |
| [1] | Wang Qiang, Li Shiyun, Xiong Ying, Li Tiantian. Biomechanical changes of the cervical spine in internal fixation with different anterior cervical interbody fusion systems [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 821-826. |
| [2] | Wei Yuanbiao, Lin Zhan, Chen Yanmei, Yang Tenghui, Zhao Xiao, Chen Yangsheng, Zhou Yanhui, Yang Minchao, Huang Feiqi. Finite element analysis of effects of sagittal cervical manipulation on intervertebral disc and facet joints [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 827-832. |
| [3] | Kang Zhijie, Cao Zhenhua, Xu Yangyang, Zhang Yunfeng, Jin Feng, Su Baoke, Wang Lidong, Tong Ling, Liu Qinghua, Fang Yuan, Sha Lirong, Liang Liang, Li Mengmeng, Du Yifei, Lin Lin, Wang Haiyan, Li Xiaohe, Li Zhijun. Finite element model establishment and stress analysis of lumbar-sacral intervertebral disc in ankylosing spondylitis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 840-846. |
| [4] | Zhang Min, Peng Jing, Zhang Qiang, Chen Dewang. Mechanical properties of L3/4 laminar decompression and intervertebral fusion in elderly osteoporosis patients analyzed by finite element method [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 847-851. |
| [5] | Xue Xiaofeng, Wei Yongkang, Qiao Xiaohong, Du Yuyong, Niu Jianjun, Ren Lixin, Yang Huifeng, Zhang Zhimin, Guo Yuan, Chen Weiyi. Finite element analysis of osteoporosis in proximal femur after cannulated screw fixation for femoral neck fracture [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 862-867. |
| [6] | Huang Peizhen, Dong Hang, Cai Qunbin, Lin Ziling, Huang Feng. Finite element analysis of anterograde and retrograde intramedullary nail for different areas of femoral shaft fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 868-872. |
| [7] | Wang Mingming, Zhang Zhong, Sun Jianhua, Zhao Gang, Song Hua, Yan Huadong, Lyu Bin. Finite element analysis of three different minimally invasive fixation methods for distal tibial fractures with soft tissue injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 879-885. |
| [8] | Hou Zexin, Xu Benke, Dai Yuan, He Chuan, Zhang Chaoju, Li Xiaolin. Finite element analysis of the mechanism of dorsiflexion injury of wrist joint in elderly people after falls [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 886-890. |
| [9] | Ning Tianliang, Wang Kun, Wang Lingbiao, Han Pengfei. Finite element analysis on correction effect of varus foot orthosis based on the three-point force principle [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 891-899. |
| [10] | Zhang Lili, Zhang Xinglai, Zhang Jie, Zheng Jiejiao. Effect of visual feedback on landing biomechanics in chronic ankle instability patients [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 900-904. |
| [11] | Liu Changzhen, Liu Xin, Li Yuefei, Wang Jianye, Feng Zhimeng, Sun Zhaozhong. Imaging landmarks of one-hole split endoscope in the treatment of upper lumbar intervertebral disc herniation under the guidance of three-dimensional reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 939-944. |
| [12] | Zhang Qianlong, Maihemuti•Yakufu, Song Chenhui, Liu Xiuxin, Ren Zheng, Liu Yuzhe, Muyashaer•Abudushalamu, Sajidan•Aikebaier, Ran Jian. Finite element analysis of the effect of the distribution position and content of bone cement on the stress and displacement of reverse femoral intertrochanteric fracture [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 336-340. |
| [13] | Chen Yuanyuan, Wang Wei, Zhao Lu, Annikaer·Aniwaer, Nijati·Turson. Finite element analysis of the influence of scaffold materials on the fixed restoration of edentulous maxillary implants under two designs [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 411-418. |
| [14] | Zhang Guorui, Zhang Kunwu, Chen Wenyuanfeng, Liu Yining, Li Duhong, Zhang Xinzhu, Cao Baocheng. Effect of different stretching lengths of lingual movable wing on the adduction of mandibular anterior teeth: a biomechanical study [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(2): 247-251. |
| [15] | . Changes in Lumbosacral Sagittal Plane Parameters of L5/S1 Disc Herniation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(在线): 1-6. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||