Chinese Journal of Tissue Engineering Research ›› 2023, Vol. 27 ›› Issue (3): 346-353.doi: 10.12307/2023.010
Previous Articles Next Articles
Inorganic ion bionic periosteum regulates immune microenvironment to promote bone repair
Zhang Lichen, Chen Liang, Gu Yong
- First Affiliated Hospital of Soochow University, Suzhou 215031, Jiangsu Province, China
-
Received:2021-11-16Accepted:2021-12-21Online:2023-01-28Published:2022-05-19 -
Contact:Chen Liang, Chief physician, Doctoral supervisor, First Affiliated Hospital of Soochow University, Suzhou 215031, Jiangsu Province, China Gu Yong, Associate chief physician, Master’s supervisor, First Affiliated Hospital of Soochow University, Suzhou 215031, Jiangsu Province, China -
About author:Zhang Lichen, Master candidate, First Affiliated Hospital of Soochow University, Suzhou 215031, Jiangsu Province, China -
Supported by:National Natural Science Foundation of China, No. 81972078, 81772312 (to CL); Jiangsu Provincial Fund for Distinguished Young Scholars, No. BK20211504 (to GY)
CLC Number:
Cite this article
Zhang Lichen, Chen Liang, Gu Yong. Inorganic ion bionic periosteum regulates immune microenvironment to promote bone repair[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(3): 346-353.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
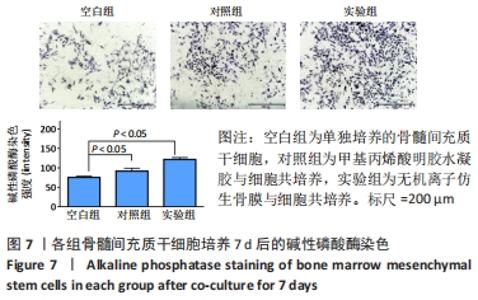
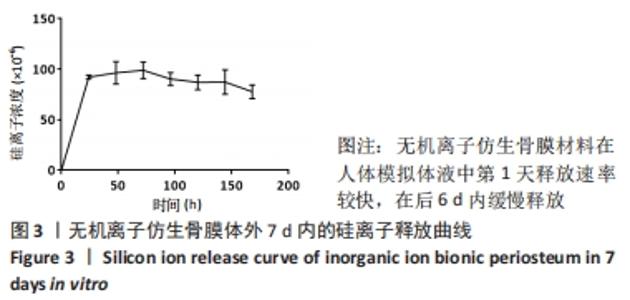
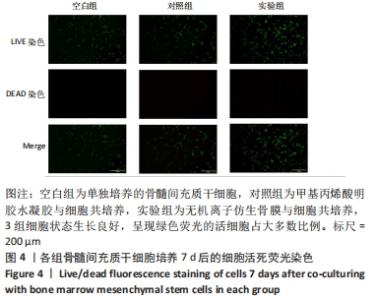
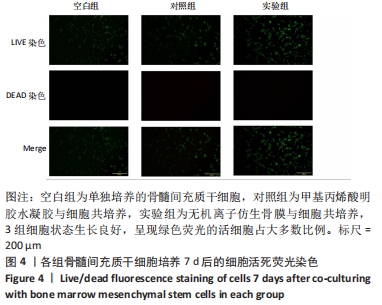
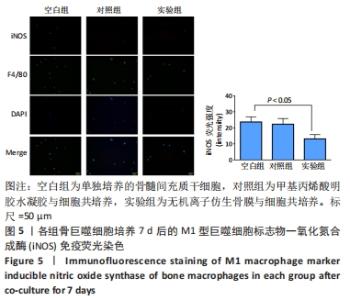
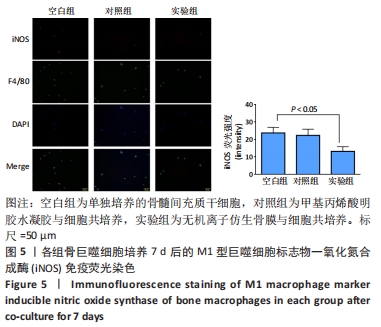
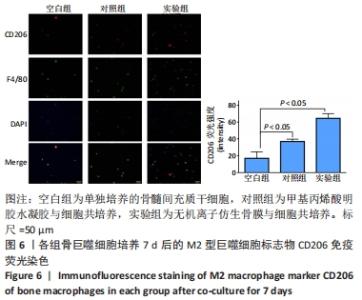
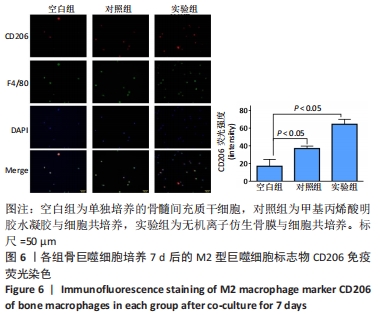
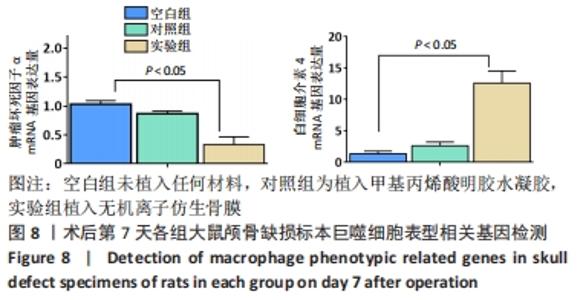
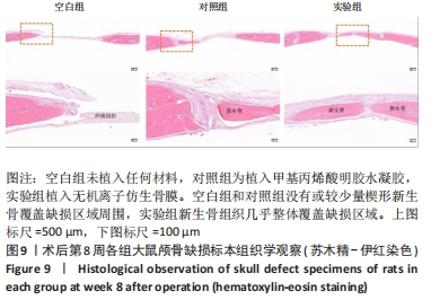
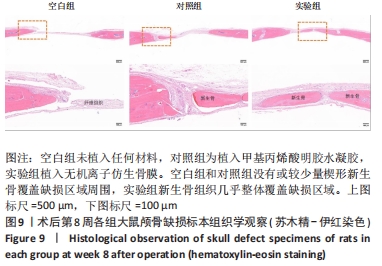
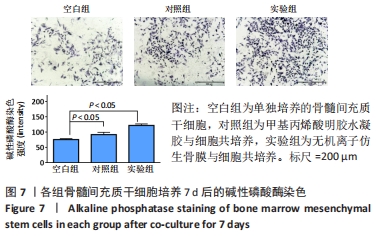
将材料与骨巨噬细胞共培养至7 d时的细胞免疫荧光结果分别见图5,6所示,两张图中荧光颜色为绿色的是巨噬细胞通标(F4/80),表明研究中骨巨噬细胞纯度较高。图5显示,呈红色的巨噬细胞M1表型(iNOS)在空白组和对照组有较高表达,实验组相对表达较少。图6显示,呈红色的巨噬细胞M2表型(CD206)在实验组表达明显较空白组和对照组高。共培养7 d后,仿生骨膜对巨噬细胞的M2极化有明显促进作用。由各组iNOS和CD206荧光半定量分析结果可见,仿生骨膜对巨噬细胞的M2极化有明显促进作用。 2.5 无机离子仿生骨膜材料的体外成骨性能 各组骨髓间充质干细胞成骨诱导培养7 d后的碱性磷酸酶染色结果,见图7,实验组染色深度明显高于空白组和对照组,证明碱性磷酸酶的表达在有仿生骨膜的实验组中更为显著。对其染色强度进行的半定量分析结果所示,碱性磷酸酶的表达在有仿生骨膜的实验组中更为显著。 "
| [1] 于明琨.自体骨移植修补颅骨缺损的材料与方法[J].中国临床康复, 2006,10(41):126-129. [2] 张贝利,张伟滨,邓廉夫.同种异体骨移植研究进展[J].国际骨科学杂志,2005,26(3):164-167. [3] BAO X, ZHU L, HUANG X, et al. 3D biomimetic artificial bone scaffolds with dual-cytokines spatiotemporal delivery for large weight-bearing bone defect repair. Sci Rep. 2017;7(1):1-13. [4] AUGUSTIN G, ANTABAK A, DAVILA S. The periosteum. Part 1: Anatomy, histology and molecular biology. Injury. 2007;38(10):1115-1130. [5] FILLINGHAM Y, JACOBS J. Bone grafts and their substitutes. Bone Joint J. 2016;98-b(1 Suppl A):6-9. [6] LI N, SONG J, ZHU G, et al. Periosteum tissue engineering-a review. Biomater Sci. 2016;4(11):1554-1561. [7] KOH TJ, DIPIETRO LA. Inflammation and wound healing: the role of the macrophage. Expert Rev Mol Med. 2011;13:e23. [8] MANTOVANI A, BISWAS SK, GALDIERO MR, et al. Macrophage plasticity and polarization in tissue repair and remodelling. J Pathol. 2013;229(2): 176-185. [9] LEE J, BYUN H, MADHURAKKAT PERIKAMANA SK, et al. Current Advances in Immunomodulatory Biomaterials for Bone Regeneration. Adv Healthc Mater. 2019;8(4):e1801106. [10] MOSSER DM, EDWARDS JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8(12):958-969. [11] JIN SS, HE DQ, LUO D, et al. A Biomimetic Hierarchical Nanointerface Orchestrates Macrophage Polarization and Mesenchymal Stem Cell Recruitment To Promote Endogenous Bone Regeneration. ACS Nano. 2019;13(6):6581-6595. [12] JI X, YUAN X, MA L, et al. Mesenchymal stem cell-loaded thermosensitive hydroxypropyl chitin hydrogel combined with a three-dimensional-printed poly(ε-caprolactone) /nano-hydroxyapatite scaffold to repair bone defects via osteogenesis, angiogenesis and immunomodulation. Theranostics. 2020;10(2):725-740. [13] LV L, XIE Y, LI K, et al. Unveiling the mechanism of surface hydrophilicity-modulated MAcrophage polarization. Adv Healthc MAter. 2018;7(19): e1800675. [14] QIAN Y, LI L, SONG Y, et al. Surface modification of nanofibrous matrices via layer-by-layer functionalized silk assembly for mitigating the foreign body reaction. Biomaterials. 2018;164:22-37. [15] CHEN Z, MAO X, TAN L, et al. Osteoimmunomodulatory properties of magnesium scaffolds coated with β-tricalcium phosphate. Biomaterials. 2014;35(30):8553-8565. [16] XIN T, MAO J, LIU L, et al. Programmed Sustained Release of Recombinant Human Bone Morphogenetic Protein-2 and Inorganic Ion Composite Hydrogel as Artificial Periosteum. ACS Appl Mater Interfaces. 2020;12(6):6840-6851. [17] GU Q, YANG H, SHI Q. Macrophages and bone inflammation. J Orthop Translat. 2017;10:86-93. [18] XIN T, GU Y, CHENG R, et al. Inorganic Strengthened Hydrogel Membrane as Regenerative Periosteum. ACS Appl Mater Interfaces. 2017;9(47):41168-41180. [19] WU L, GU Y, LIU L, et al. Hierarchical micro/nanofibrous membranes of sustained releasing VEGF for periosteal regeneration. Biomaterials. 2020;227:119555. [20] Tang J, Gu Y, ZHANG H, et al.Outer-inner dual reinforced micro/nano hierarchical scaffolds for promoting osteogenesis. Nanoscale 2019;11(34):15794-15803. [21] MILLS CD, THOMAS AC, LENZ LL, et al. Macrophage: SHIP of Immunity. Front Immunol. 2014;5:620. [22] GRANEY PL, ROOHANI-ESFAHANI SI, ZREIQAT H, et al. In vitro response of macrophages to ceramic scaffolds used for bone regeneration. J R Soc Interface. 2016;13(120):20160346. [23] GONG L, ZHAO Y, ZHANG Y, et al. The MAcrophage polarization regulates MSC osteoblast differentiation in vitro. Ann Clin Lab Sci. 2016;46:65e71. [24] HUANG Y, WU C, ZHANG X, et al. Regulation of immune response by bioactive ions released from silicate bioceramics for bone regeneration. Acta Biomater. 2018;66:81-92. [25] LI T, PENG M, YANG Z, et al. 3D-printed IFN-γ-loading calcium silicate-β-tricalcium phosphate scaffold sequentially activates M1 and M2 polarization of macrophages to promote vascularization of tissue engineering bone. Acta Biomater. 2018;71:96-107. [26] 武敬文,杨岚,李源静,等.介孔生物活性玻璃研究进展[J].生物医学工程学杂志,2018,35(4):153-156. [27] HENCH LL, SPLINTER RJ, ALLEN WC, et al. Bonding mechanisms at the interface of ceramic prosthetic materials. J Biomed Mater Res. 1971;5(6):117-141. [28] CHEN C, TANG J, GU Y, et al. Bioinspired Hydrogel Electrospun Fibers for Spinal Cord Regeneration. Adv Functl Mater. 2019;29(4). doi.org/10.1002/adfm.201806899 [29] ZHU D, SU Y, YOUNG ML, et al. Biological Responses and Mechanisms of Human Bone Marrow Mesenchymal Stem Cells to Zn and Mg Biomaterials. ACS Appl Mater Interfaces. 2017;9(33):27453-27461. [30] XI K, GU Y, TANG J, et al. Microenvironment-responsive immunoregulatory electrospun fibers for promoting nerve function recovery [published correction appears in Nat Commun. Nat Commun. 2020;11(1):4504. [31] WU T, CHENG N, XU C, et al. The effect of mesoporous bioglass on osteogenesis and adipogenesis of osteoporotic BMSCs. J Biomed MAter Res A. 2016;104(12):3004-3014. [32] MIRON RJ, SCULEAN A, SHUANG Y, et al. Osteoinductive potential of a novel biphasic calcium phosphate bone graft in comparison with autographs, xenografts, and DFDBA. Clin Oral Implants Res. 2016; 27(6):668-675. [33] BOSCH C, MELSEN B, VARGERVIK K. Importance of the critical-size bone defect in testing bone-regenerating materials. J Craniofac Surg. 1998;9(4):310-316. [34] PAJARINEN J, LIN T, GIBON E, et al. Mesenchymal stem cell-macrophage crosstalk and bone healing. Biomaterials. 2019;196:80-89. [35] GU Q, YANG H, SHI Q. Macrophages and bone inflammation. J Orthop Translat. 2017;10:86-93. [36] VASCONCELOS DP, FONSECA AC, COSTA M, et al. Macrophage polarization following chitosan implantation. Biomaterials. 2013; 34(38):9952-9959 |
| [1] | Yang Yufang, Yang Zhishan, Duan Mianmian, Liu Yiheng, Tang Zhenglong, Wang Yu. Application and prospects of erythropoietin in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1443-1449. |
| [2] | Yang Yifeng, Ye Nan, Wang Lin, Guo Shuaicheng, Huang Jian. Signaling pathway of dexmedetomidine against ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1464-1469. |
| [3] | Wang Ji, Zhang Min, Li Wenbo, Yang Zhongya, Zhang Long. Effect of aerobic exercise on glycolipid metabolism, skeletal muscle inflammation and autophagy in type 2 diabetic rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1200-1205. |
| [4] | Wang Weiqing, Zhou Yue. Chronic inflammation regulates adipose tissue fibrosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1307-1312. |
| [5] | Mu Bingtao, Yu Jingwen, Liu Chunyun, Guo Minfang, Meng Tao, Yang Pengwei, Wei Wenyue, Song Lijuan, Yu Jiezhong, Ma Cungen. Immunomodulatory effect of astragaloside IV on T cells of experimental autoimmune encephalomyelitis mice [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1057-1062. |
| [6] | Zeng Fanzhuo, Li Yuxin, Sun Jiachen, Gu Xinyang, Wen Shan, Tian He, Mei Xifan. Efficient strategies for microglia replacement in spinal cord injury models [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1007-1014. |
| [7] | Zhang Kefan, Shi Hui. Research status and application prospect of cytokine therapy for osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 961-967. |
| [8] | Zhang Ya, Mu Qiuju, Wang Zilin, Liu Hongjie, Zhu Lili. Hydrogel loaded with platelet-rich plasma promotes wound healing in diabetic rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 690-696. |
| [9] | Yang Yuqing, Chen Zhiyu. Role and application of early transient presence of M1 macrophages in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 594-601. |
| [10] | Pan Shihong, Liu Ruiduan. Mitophagy and intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(36): 5872-5876. |
| [11] | Li Yulin, Yu Haipeng, Tang Huajing, Zhang Zitong, Lin Xingnan. The mechanism, safety and application of berberine in promoting bone regeneration [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(35): 5702-5708. |
| [12] | Xie Yanli, Wei Siang, Zhang Guodong. Effects of treadmill exercise on metabolism and chronic neuroinflammation in type 1 diabetes mice of different sexes [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(35): 5577-5583. |
| [13] | Zhang Yuchang, Chen Xiang, He Bo, Li Shenghua, Mu Xiangqian, Sun Weiqiang, Zhang Li, Chen Jie. Role of inflammatory factors in diabetic ulcers and prospects of traditional Chinese medicine intervention [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(34): 5544-5551. |
| [14] | Ren Weiliang, Jiao Yongwei, Zhang Jian, Yang Liying, Yang Qi. Modulatory effect of resveratrol on oxidative stress and inflammatory factors in the joint fluid of rats with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5154-5158. |
| [15] | Hou Zengtao, Dong Zhiwei, Zhang Jinfeng, Yang Xiaohui, Fan Xiao. Platelet-rich fibrin regulates apoptosis to promote cartilage repair in rats with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(32): 5167-5171. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||