Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (33): 5364-5369.doi: 10.12307/2022.711
Previous Articles Next Articles
Oblique lumbar interbody fusion combined with lateral plate versus combined with pedicle screw fixation via the posterior approach for lumbar degenerative diseases: a six-month follow-up
Lang Zhao, Ge Tenghui, Wu Jingye, Zhang Ning, Tian Wei, Sun Yuqing
- Department of Spine Surgery, Beijing Jishuitan Hospital, Beijing 100035, China
-
Received:2021-09-04Accepted:2021-10-28Online:2022-11-28Published:2022-03-31 -
Contact:Sun Yuqing, MD, Chief physician, Associate professor, Department of Spine Surgery, Beijing Jishuitan Hospital, Beijing 100035, China -
About author:Lang Zhao, MD, Associate chief physician, Department of Spine Surgery, Beijing Jishuitan Hospital, Beijing 100035, China
CLC Number:
Cite this article
Lang Zhao, Ge Tenghui, Wu Jingye, Zhang Ning, Tian Wei, Sun Yuqing. Oblique lumbar interbody fusion combined with lateral plate versus combined with pedicle screw fixation via the posterior approach for lumbar degenerative diseases: a six-month follow-up[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(33): 5364-5369.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
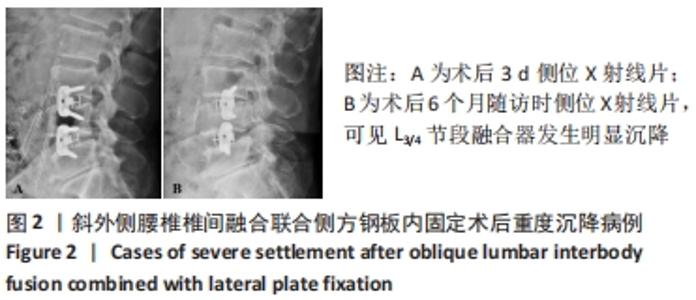
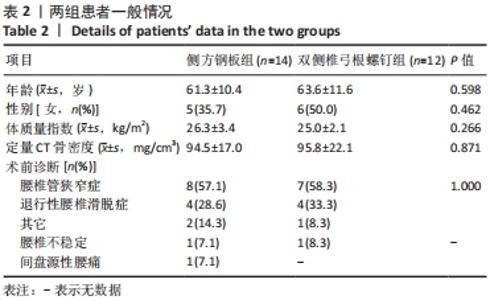
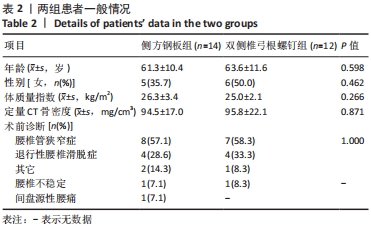
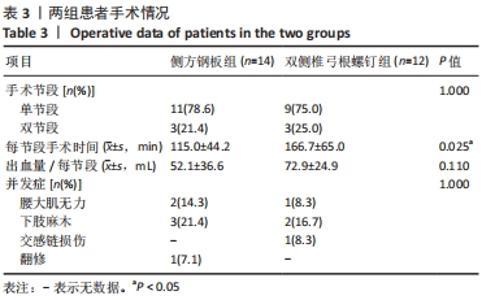
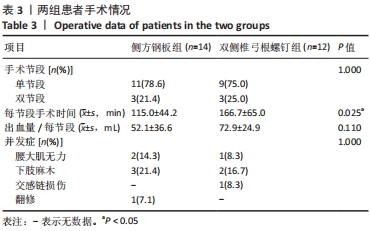
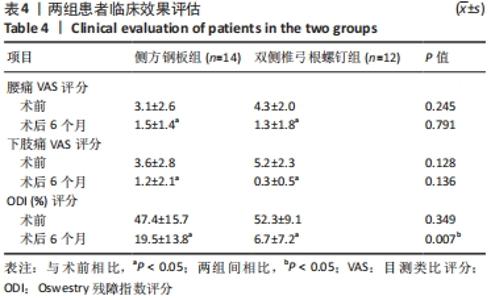
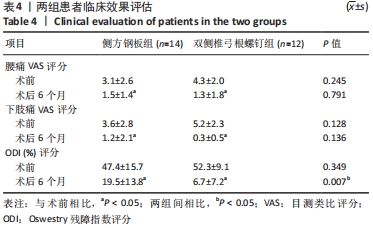
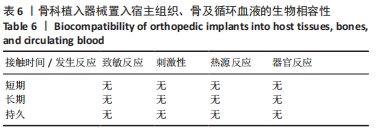
2.5 影像学结果 侧方钢板组17个手术节段中4个位于L3/4,13个位于L4/5;双侧椎弓根螺钉组15个手术节段中4个位于L3/4,11个位于L4/5。两组间融合器高度及长度差异无显著性意义。侧方钢板组融合器前凸角度(8.8±3.7)°显著小于双侧椎弓根螺钉组(14.0±2.9)°。术前及术后3 d两组椎间隙高度差异无显著性意义,术后6个月侧方钢板组椎间隙高度显著小于双侧椎弓根螺钉组(P=0.044)。术前、术后3 d及术后6个月两组间节段性脊柱前凸角差异无显著性意义。术后3 d相比术前,两组椎间隙高度和节段性脊柱前凸角均有显著性提高;术后6个月相比术后3 d,两组的椎间隙高度均出现显著性丢失(P < 0.05),侧方钢板组的节段性脊柱前凸角出现显著性改变(P < 0.05)。虽然术后6个月融合器沉降率两组间差异无显著性意义,但侧方钢板组融合器重度沉降2例,占12%,见图2;而双侧椎弓根螺钉组无重度沉降病例。"
| [1] HAH R, KANG HP. Lateral and Oblique Lumbar Interbody Fusion-Current Concepts and a Review of Recent Literature. Curr Rev Musculoskelet Med. 2019;12(3):305-310. [2] LI R, LI X, ZHOU H, et al. Development and Application of Oblique Lumbar Interbody Fusion. Orthop Surg. 2020;12(2):355-365. [3] LI JX, PHAN K, MOBBS R. Oblique Lumbar Interbody Fusion: Technical Aspects, Operative Outcomes, and Complications. World Neurosurg. 2017; 98:113-123. [4] PHAN K, MAHARAJ M, ASSEM Y, et al. Review of early clinical results and complications associated with oblique lumbar interbody fusion (OLIF). J Clin Neurosci. 2016;31:23-29. [5] LI HM, ZHANG RJ, SHEN CL. Radiographic and Clinical Outcomes of Oblique Lateral Interbody Fusion Versus Minimally Invasive Transforaminal Lumbar Interbody Fusion for Degenerative Lumbar Disease. World Neurosurg. 2019; 122:e627-e638. [6] SATO J, OHTORI S, ORITA S, et al. Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J. 2017;26(3):671-678. [7] ZHANG QY, TAN J, HUANG K, at al. Minimally invasive transforaminal lumbar interbody fusion versus oblique lateral interbody fusion for lumbar degenerative disease: a meta-analysis. BMC Musculoskelet Disord. 2021;22(1):802. [8] MALHAM GM, ELLIS NJ, PARKER RM, et al. Maintenance of Segmental Lordosis and Disk Height in Stand-alone and Instrumented Extreme Lateral Interbody Fusion (XLIF) . Clin Spine Surg. 2017;30(2):E90-E98. [9] CARLSON BB, SAVILLE P, DOWDELL J, et al. Restoration of lumbar lordosis after minimally invasive transforaminal lumbar interbody fusion: a systematic review. Spine J. 2019;19(5):951-958. [10] MARCHI L, ABDALA N, OLIVEIRA L, et al. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 2013;19(1):110-118. [11] TEMPEL ZJ, GANDHOKE GS, BOLINGER BD, et al. Vertebral body fracture following stand-alone lateral lumbar interbody fusion (LLIF): report of two events out of 712 levels. Eur Spine J. 2015;24 Suppl 3:409-413. [12] ABE K, ORITA S, MANNOJI C, et al. Perioperative Complications in 155 Patients Who Underwent Oblique Lateral Interbody Fusion Surgery: Perspectives and Indications From a Retrospective, Multicenter Survey. Spine (Phila Pa 1976). 2017;42(1):55-62. [13] BOCAHUT N, AUDUREAU E, POIGNARD A, et al. Incidence and impact of implant subsidence after stand-alone lateral lumbar interbody fusion. Orthop Traumatol Surg Res. 2018;104(3):405-410. [14] LIU X, MA J, PARK P, et al. Biomechanical comparison of multilevel lateral interbody fusion with and without supplementary instrumentation: a three-dimensional finite element study. BMC Musculoskelet Disord. 2017;18(1): 63. [15] REIS MT, REYES PM BSE, ALTUN I, et al. Biomechanical evaluation of lateral lumbar interbody fusion with secondary augmentation. J Neurosurg Spine. 2016;25(6):720-726. [16] ZHANG Z, FOGEL GR, LIAO Z, et al. Biomechanical Analysis of Lateral Lumbar Interbody Fusion Constructs with Various Fixation Options: Based on a Validated Finite Element Model. World Neurosurg. 2018;114:e1120-e1129. [17] CHEN E, XU J, YANG S, et al. Cage Subsidence and Fusion Rate in Extreme Lateral Interbody Fusion with and without Fixation. World Neurosurg. 2019; 122:e969-e977. [18] PALEPU V, HELGESON M, MOLYNEAUX-FRANCIS M, et al. The effects of bone microstructure on subsidence risk for ALIF, LLIF, PLIF, and TLIF spine cages. J Biomech Eng. 2018. [Epub ahead of print]. doi: 10.1115/1.4042181. [19] MACKI M, ANAND SK, SURAPANENI A, et al. Subsidence Rates After Lateral Lumbar Interbody Fusion: A Systematic Review. World Neurosurg. 2019;122:599-606. [20] WALKER CT, FARBER SH, COLE TS, et al. Complications for minimally invasive lateral interbody arthrodesis: a systematic review and meta-analysis comparing prepsoas and transpsoas approaches. J Neurosurg Spine. 2019; 1-15. [Epub ahead of print]. doi: 10.3171/2018.9.SPINE18800. [21] SPIESSBERGER A, ARVIND V, DIETZ N, et al. A Comparison of Complications and Clinical and Radiologic Outcome Between the Mini-open Prepsoas and Mini-open Transpsoas Approaches for Lumbar Interbody Fusion: A Meta-Analysis. Clin Spine Surg. 2020;33(7):271-279. [22] BEUTLER WJ, PEPPELMAN WC JR. Anterior lumbar fusion with paired BAK standard and paired BAK Proximity cages: subsidence incidence, subsidence factors, and clinical outcome. Spine J. 2003;3(4):289-293. [23] SCHIFFMAN M, BRAU SA, HENDERSON R, et al. Bilateral implantation of low-profile interbody fusion cages: subsidence, lordosis, and fusion analysis. Spine J. 2003;3(5):377-387. [24] TEMPEL ZJ, GANDHOKE GS, OKONKWO DO, et al. Impaired bone mineral density as a predictor of graft subsidence following minimally invasive transpsoas lateral lumbar interbody fusion. Eur Spine J. 2015;24 Suppl 3: 414-419. [25] TEMPEL ZJ, MCDOWELL MM, PANCZYKOWSKI DM, et al. Graft subsidence as a predictor of revision surgery following stand-alone lateral lumbar interbody fusion. J Neurosurg Spine. 2018;28(1):50-56. [26] FOGEL GR, PARIKH RD, RYU SI, et al. Biomechanics of lateral lumbar interbody fusion constructs with lateral and posterior plate fixation: laboratory investigation. J Neurosurg Spine. 2014;20(3):291-297. [27] TENDER GC. Caudal vertebral body fractures following lateral interbody fusion in nonosteoporotic patients. Ochsner J. 2014;14(1):123-130. [28] LE TV, BAAJ AA, DAKWAR E, et al. Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine (Phila Pa 1976). 2012;37(14):1268-1273. [29] CHOI JY, SUNG KH. Subsidence after anterior lumbar interbody fusion using paired stand-alone rectangular cages. Eur Spine J. 2006;15(1):16-22. [30] DUA K, KEPLER CK, HUANG RC, et al. Vertebral body fracture after anterolateral instrumentation and interbody fusion in two osteoporotic patients. Spine J. 2010;10(9):e11-e15. [31] LE TV, SMITH DA, GREENBERG MS, et al. Complications of lateral plating in the minimally invasive lateral transpsoas approach. J Neurosurg Spine. 2012;16(3):302-307. |
| [1] | Wei Bing, Chang Shan. Finite element analysis of different angles of nail placement in sagittal plane of spinal fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 864-869. |
| [2] | Song Yuxin, Zhang Tongtong, Niu Jianxiong, Wang Zengping, Wen Jie, Zhang Qunli, Xue Wen, Liu Lin. Precise screw placement of 3D printing model and orthopedic robot in spinal deformity [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 904-907. |
| [3] | Yang Jun, Yang Qun, Zhang Rui, Jiang Chang. A novel slidable pedicle screw-rod system for lumbar tuberculosis: promoting bone graft fusion by producing stress stimulation to fused segment [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 914-918. |
| [4] | Guo Xiaohui, Song Xizheng, Xiang Hanrui, Kang Zhaorong, Li Daming, Kang Yu, Hu Jun, Sheng Kai. External spinal fixation elastic stress in the treatment of jumping spinal fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 919-923. |
| [5] | Xu Wei, Li Zhifei, Wan Tong, Yu Weibo, Zhang Yisheng, Zhou Jinyan, Bu Xianzhong, Zhong Yuanming. Application of height adjustable titanium fusion cage in endoscopic lumbar fusion [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(33): 5335-5341. |
| [6] | Li Lu, Tang Wen. Screw placement in posterior route pedicle on subaxial cervical spine: how to improve the therapeutic effect with the development of artificial intelligence [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 474-479. |
| [7] | Cai Feng, Yu Bo, Zeng Duo, Chen Qincan, Liao Qi. Cortical bone trajectory in elderly patients with osteoporosis of lumbar disease [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 403-407. |
| [8] | Feng Shuo, Liu Bo, He Da. Effects of robot-assisted percutaneous minimally invasive pedicle screw placement in oblique lumbar interbody fusion [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 408-413. |
| [9] | Lin Shu, Hu Jiang, Wan Lun, Tang Liuyi, Wang Yue, Yu Yang. Orthopedic robot-assisted cortical bone trajectory screw internal fixation for the treatment of lumbar degenerative diseases [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(15): 2356-2360. |
| [10] | Yuan Cuihua, Lin Wang, Jiang Yao, Liu Chengzhao. Screw track in computer navigation-assisted percutaneous hollow pedicle screw placement [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(12): 1861-1865. |
| [11] | Hou Guangyuan, Zhang Jixue, Zhang Zhijun, Meng Xianghui, Duan Wen, Gao Weilu. Bone cement pedicle screw fixation and fusion in the treatment of degenerative spinal disease with osteoporosis: one-year follow-up [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 878-883. |
| [12] | Guo Haiwei, Xie Jiahao, Lin Yanping, Wang Yufeng, Yang Qingqi. Effects and safety of fenestrated and conventional pedicle screw combined with cement-augmentation in osteoporotic vertebral fixation: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(30): 4891-4899. |
| [13] | Zhong Yuanming, Wan tong, Zhong Xifeng, Wu Zhuotan, He Bingkun, Wu Sixian. Efficacy and safety of three-dimensional model assisted screw placement technique and traditional screw placement technique in the treatment of spinal deformity: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(30): 4900-4906. |
| [14] | Hu Jing, Xiang Yang, Ye Chuan, Han Ziji. Three-dimensional printing assisted screw placement and freehand pedicle screw fixation in the treatment of thoracolumbar fractures: 1-year follow-up [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3804-3809. |
| [15] | Zou Shouping, Lu Daoyun, Ye Li. Minimally invasive percutaneous pedicle screw technique for thoracolumbar fractures: biomechanical changes of the spine during 6-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3865-3869. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||