[1] 董振宇,安春青,李建江,等.侧路融合术治疗退变性腰椎侧凸的临床疗效分析[J].中国矫形外科杂志,2016,24(3):274-277.
[2] XU L, SUN X , HUANG S, et al. Degenerative lumbar scoliosis in Chinese Han population: prevalence and relationship to age, gender, bone mineral density, and body mass index. Eur Spine. 2013;22(6):1326 -1331.
[3] DE VRIES AA, MULLENDER MG, PLUYMAKERS WJ, et al. Spinal decompensation in degenerative lumbar scoliosis. Eur Spine J. 2010; 19(9):1540-1544.
[4] PELLISE F, VILA-CASADEMUNT A, FERRER M, et al. Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J. 2015;24(1):3-11.
[5] FERRERO E, OULDSLIMANE M, GILLE O, et al. Sagittal spinopelvic alignment in 654 degenerative spondylolisthesis. Eur Spine J. 2015; 24(6):1219-1227.
[6] LIU H, LI S, ZHENG Z, et al. Pelvic retroversion is the key protective mechanism of L4-5 degenerative spondylolisthesis. Eur Spine J. 2015; 24(6):1204-1211.
[7] SCHWAB FJ, BLONDEL B, BESS S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine. 2013;38(13):E803-812.
[8] BESS S, SCHWAB F, LAFAGE V, et al. Classifications for adult spinal deformity and use of the scoliosis research society Schwab adult spinal deformity classification. Neurosurg Clin N Am. 2013;24(2):185-193.
[9] ZHU Z, XU L, ZHU F, et al. Sagittal alignment of spine and pelvis in asymptomatic adults: norms in Chinese populations. Spine. 2014;39(1): E1-6.
[10] 李危石,费晗,陈仲强,等. 退变性腰椎侧凸患者腰椎前凸矫正程度与疗效的关系[J]. 中国脊柱脊髓杂志,2016,26(10):912-918.
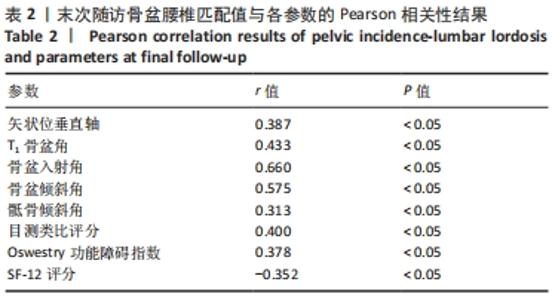
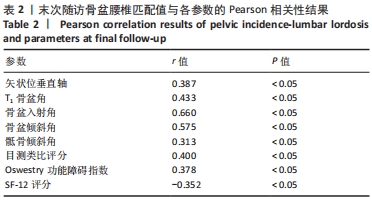
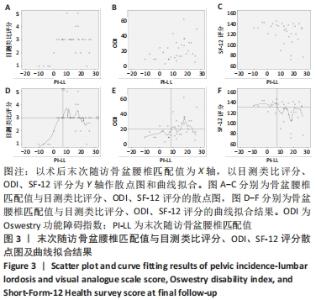
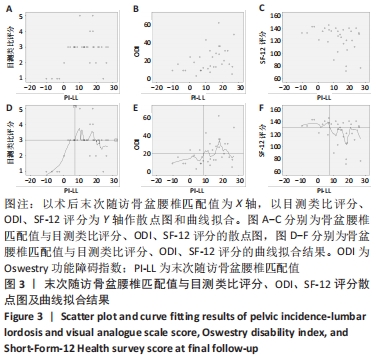
[11] 孙祥耀,张希诺,海涌.退变性脊柱侧凸术后骨盆投射角与腰椎前凸角匹配程度与临床疗效的关系[J]. 中国骨与关节杂志,2017,6(1): 20-26.
[12] 曹海云,邹吉锋.后路手术治疗腰椎退变性侧凸50例分析[J].中国矫形外科杂志,2017,25(13):1239-1242.
[13] 费晗,李危石,孙卓然,等.退变性腰椎侧凸脊柱-骨盆矢状位影像学特点[J].中国脊柱脊髓杂志,2015,25(6):528-532+540.
[14] LEGAYE J, DUVAL-BEAUPÈRE G, HECQUET J, et al. Pelvic incidence: a fundamental pelvicparameter for three-dimensional regulation of spinal sagittal curves. Eur Spine. 1998;7(2):99-103.
[15] 乔军,邱勇,朱锋,等.T1骨盆角与退变性脊柱侧凸患者脊柱-骨盆矢状面平衡以及生活质量的相关性分析[J].中国脊柱脊髓杂志, 2014,24(8):686-690.
[16] 刘辰君,朱震奇,段硕,等.退变性胸腰交界区后凸及其矢状位平衡代偿机制的影像学分析[J].中国脊柱脊髓杂志,2018,28(2):158-163.
[17] RYAN D, PROTOPSALTIS T, AMES C, et al. T1 pelvic angle(TPA) effectively evaluates sagittal deformity and assesses radiographical surgical outcomes longitudinally. Spine. 2014;39(15):1203-1210.
[18] 赵耀,漆龙涛,李淳德,等.骨盆腰椎匹配值与成人退变性脊柱侧凸畸形术后疗效的相关性研究[J].中国脊柱脊髓杂志,2016,26(8): 701-708.
[19] MAC-THIONG JM, BERTHONNAUD E, DIMAR JR, et al. Sagittal alignment of the spine and pelvis during growth. Spine. 2004;29(5):1642-1647.
[20] BARREY C, JUND J, NOSEDA O, et al. Sagittal balance of thepelvis-spine complex and lumbar degenerative diseases: a comparative study about 85 cases. Eur Spine J. 2007;16(9):1459-1467.
[21] 王兆宁,郑立峰,陈岩,等.退变性腰椎滑脱患者脊柱-骨盆矢状位参数及小关节的研究[J].现代生物医学进展,2017,17(35):6882-6886.
[22] AOKI Y, NAKAJIMA A, TAKAHASHI H, et al. Influence of pelvic incidence-lumbar lordosis mismatch on surgical outcomes of short-segment transforaminal lumbar interbody fusion. BMC Musculoskelet Disord. 2015;16:213.
[23] HA KY, JANG WH, KIM YH, et al. Clinical relevance of the SRS-Schwab classification for degenerative lumbar scoliosis. Spine. 2016;41(5): E282-288.
[24] NEAL CJ, MCCLENDON J, HALPIN R, et al. Predicting ideal spinopelvic balance in adult spinal deformity. J Neurosurg Spine. 2011;15(1):82-91.
[25] YAMADA K, ABE Y, YANAGIBASHI Y, et al. Mid- and long-term clinical outcomes of corrective fusion surgery which did not achieve sufficient pelvic incidence minus lumbar lordosis value for adult spinal deformity. Scoliosis. 2015;10(Suppl 2):S17
[26] INAMI S, MORIDAIRA H, TAKEUCHI D, et al. Optimum pelvic incidence minus lumbar lordosis value can be determined by individual pelvic incidence. Eur Spine J. 2016;25(11):3638-3643.
[27] 朱锋,鲍虹达,邱勇,等.比较经椎弓根与Smith-Peterson截骨对退变性侧后凸畸形冠矢状面平衡重建的影响[J].中华骨科杂志, 2014,34(4):347-354.
[28] 王岩.对脊柱畸形截骨矫治及退变性脊柱畸形治疗的认识 [J].中国脊柱脊髓杂志,2011,21(9):706-707.
[29] 王乃国,王以朋,邱贵兴,等.短节段融合对退变性腰椎侧凸邻近节段椎间角的影响[J].中华外科杂志,2010,48(7):506-510.
[30] HIOKI A, MIYAMOTO K, KODAMA H, et al. Two -lev-el posterior lumbar interbody fusion for degenerative disc disease: improved clinical outcome with restoration of lumbar lordosis. Spine J. 2005;5(6):600-607.
|