Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (12): 1879-1885.doi: 10.3969/j.issn.2095-4344.3769
Previous Articles Next Articles
A 5-year follow-up on sagittal alignment and radiological outcomes of consecutive three-level anterior cervical discectomy and fusion and hybrid surgery
Ma Long, Tan Xiaoxin, Sun Guoshao
- Pingdingshan First People’s Hospital, Pingdingshan 467000, Henan Province, China
-
Received:2020-04-16Revised:2020-04-23Accepted:2020-06-03Online:2021-04-28Published:2020-12-25 -
Contact:Ma Long, Associate chief physician, Pingdingshan First People’s Hospital, Pingdingshan 467000, Henan Province, China -
About author:Ma Long, Master, Associate chief physician, Pingdingshan First People’s Hospital, Pingdingshan 467000, Henan Province, China
CLC Number:
Cite this article
Ma Long, Tan Xiaoxin, Sun Guoshao. A 5-year follow-up on sagittal alignment and radiological outcomes of consecutive three-level anterior cervical discectomy and fusion and hybrid surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1879-1885.
share this article
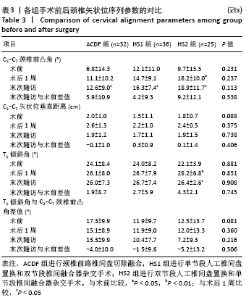
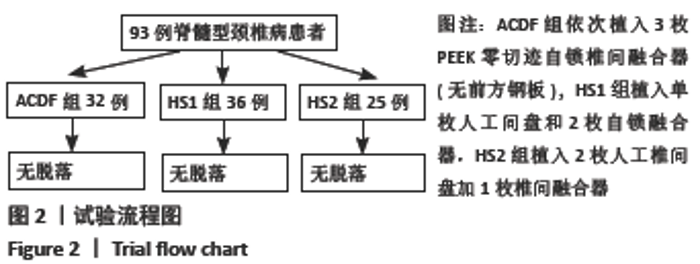
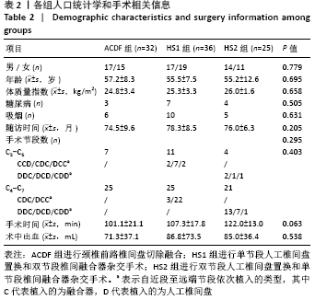
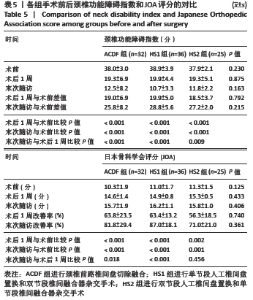
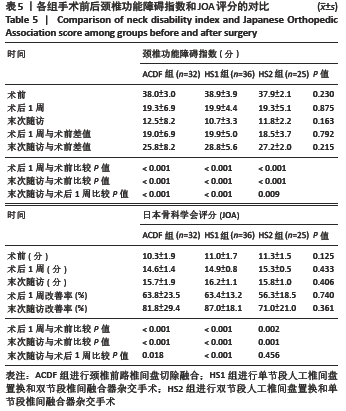
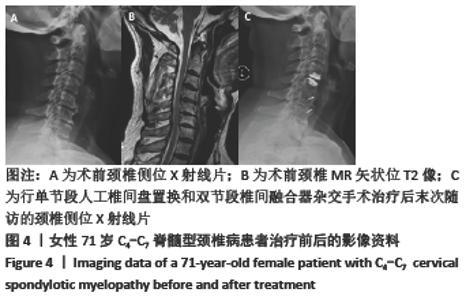
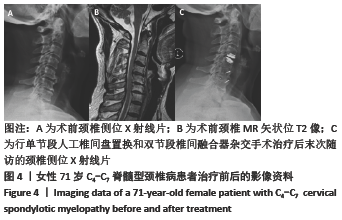
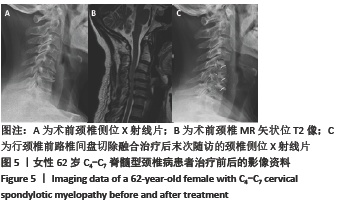
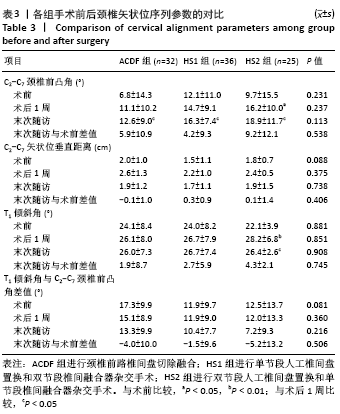
2.4 各组影像学参数测量结果 2.4.1 颈椎矢状位序列 术前、术后1周和末次随访时,3组间C2-C7颈椎前凸角比较差异无显著性意义(P > 0.05);3组术后的C2-C7颈椎前凸角均较术前有程度的增加。HS1组术前的C2-C7矢状位垂直距离、T1倾斜角与C2-C7颈椎前凸角差值小于ACDF组(P < 0.05),术后1周及末次随访组间比较差异无显著性意义(P > 0.05);3组术后1周的C2-C7矢状位垂直距离、T1倾斜角与C2-C7颈椎前凸角差值与末次随访比较差异无显著性意义(P > 0.05)。HS2组术后1周及末次随访的T1倾斜角均较术前有改善(P < 0.05),ACDF组、HS1组组内手术前后的T1倾斜角比较差异无显著性意义(P > 0.05),3组间T1倾斜角比较差异无显著性意义(P > 0.05)。3组间所有矢状位参数末次随访相对术前的改变值比较差异无显著性意义(P > 0.05)。具体结果见表3。 "
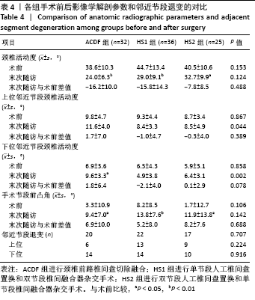
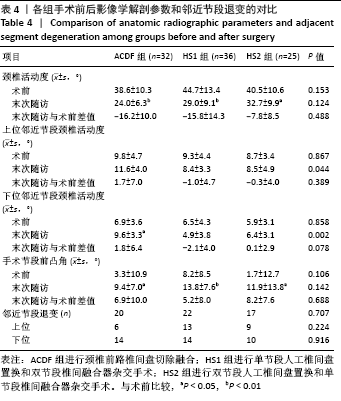
2.4.2 颈椎解剖参数和影像学并发症 术前和末次随访时,3组间颈椎活动度及其改变值比较差异无显著性意义(P > 0.05);末次随访时,3组的颈椎活动度均较术前减少(P < 0.05)。术前,3组间上位和下位邻近节段颈椎活动度比较差异无显著性意义(P > 0.05);末次随访时,HS1组、HS2组上位和下位邻近节段颈椎活动度小于ACDF组(P < 0.05)。术前及末次随访时,3组间手术节段前凸角比较差异无显著性意义(P > 0.05);末次随访时,3组的手术节段前凸角均较术前改善(P < 0.05)。具体结果见表4。 3组间邻近节段退变总体发生率比较差异无显著性意义(P > 0.05),上位和下位节段邻近节段退变发生率比较差异无显著性意义(P > 0.05),见表4。 "
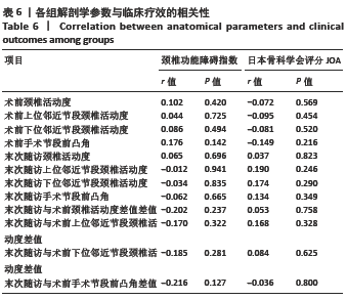
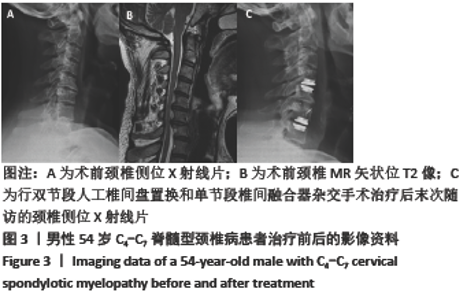
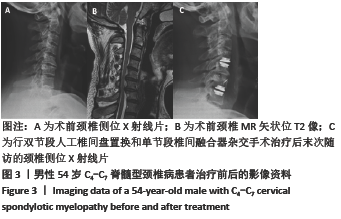
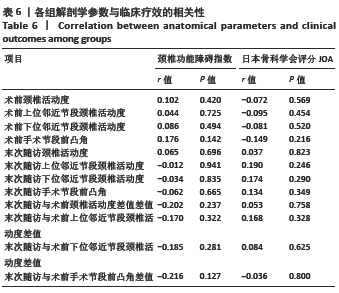
2.6 颈椎解剖学参数与临床疗效的相关性 因3组影像学参数和临床疗效的异质性较小,故将3组数据合并,分析颈椎解剖学参数和颈椎功能障碍指数与JOA评分的相关性。表6显示,解剖学参数在术前、末次随访及其变化值与同时期颈椎功能障碍指数与JOA评分均无明确相关性(P > 0.05)。此外,将患者随访末次分为无邻近节段退变(34例)和出现邻近节段退变(59例)两组,两组颈椎功能障碍指数和JOA评分比较差异无显著性意义(P=0.151,0.121)。根据T1倾斜角与C2-C7颈椎前凸角差值分为末次平衡组(79例)和失衡组(14例),两组患者颈椎功能障碍指数和JOA评分比较差异无显著性意义(P=0.403,0.484)。 2.7 不良反应 ACDF组中仅1例患者因重度压迫和临床疗效改善不明显,再次行后路单开门颈椎管扩大成形术,而HS1组和HS2组中均无二次手术病例。3组患者中所有椎间融合器植入间隙在末次随访时获得100%融合。然而行TDR的所有节段中,HS1组中2个节段(2/36)和HS2组中1个节段(1/50)在末次随访出现锁死、颈椎活动度消失。 "
| [1] BASQUES BA, LOUIE PK, MORMOL J, et al. Multi- versus single-level anterior cervical discectomy and fusion: comparing sagittal alignment, early adjacent segment degeneration, and clinical outcomes. Eur Spine J. 2018;27(11):2745-2753. [2] AMES CP, BLONDEL B, SCHEER JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976). 2013;38(22 Suppl 1):S149-S160. [3] KÖNIG SA, RANGUIS S, SPETZGER U. Hybrid Solutions for the Surgical Treatment of Multilevel Degenerative Cervical Disk Disease. Surg J (N Y). 2015;1(1):e16-e22. [4] JIANG L, TAN M, DONG L, et al. Comparison of Anterior Decompression and Fusion With Posterior Laminoplasty for Multilevel Cervical Compressive Myelopathy: A Systematic Review and Meta-Analysis. J Spinal Disord Tech. 2015;28(8):282-290. [5] PIMENTA L, MCAFEE PC, CAPPUCCINO A, et al. Superiority of multilevel cervical arthroplasty outcomes versus single-level outcomes: 229 consecutive PCM prostheses. Spine (Phila Pa 1976). 2007;32(12):1337-1344. [6] KANG L, LIN D, DING Z, et al. Artificial disk replacement combined with midlevel ACDF versus multilevel fusion for cervical disk disease involving 3 levels. Orthopedics. 2013;36(1):e88-e94. [7] GRASSO G. Clinical and radiological features of hybrid surgery in multilevel cervical degenerative disc disease. Eur Spine J. 2015;24 Suppl 7:842-848. [8] LI Y, SHEN H, KHAN KZ, et al. Comparison of Multilevel Cervical Disc Replacement and Multilevel Anterior Discectomy and Fusion: A Systematic Review of Biomechanical and Clinical Evidence. World Neurosurg. 2018;116: 94-104. [9] ALHASHASH M, SHOUSHA M, BOEHM H. Adjacent Segment Disease After Cervical Spine Fusion: Evaluation of a 70 Patient Long-Term Follow-Up. Spine (Phila Pa 1976). 2018;43(9):605-609. [10] XIONG Y, XU L, YU X, et al. Comparison of 6-year Follow-up Result of Hybrid Surgery and Anterior Cervical Discectomy and Fusion for the Treatment of Contiguous Two-segment Cervical Degenerative Disc Diseases. Spine (Phila Pa 1976). 2018;43(20):1418-1425. [11] AMES CP, SMITH JS, EASTLACK R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine. 2015; 23(6):673-683. [12] DI MARTINO A, PAPALIA R, ALBO E, et al. Cervical spine alignment in disc arthroplasty: should we change our perspective? Eur Spine J. 2015;24 Suppl 7:810-825. [13] JI GY, OH CH, SHIN DA, et al. Artificial Disk Replacement Combined With Fusion Versus 2-Level Fusion in Cervical 2-Level Disk Disease With a 5-Year Follow-up. Clin Spine Surg. 2017;30(5):E620-E627. [14] CHEN H, LIU H, MENG Y, et al. Short-Term Outcomes of Anterior Fusion-Nonfusion Hybrid Surgery versus Posterior Cervical Laminoplasty in the Treatment of Multilevel Cervical Spondylotic Myelopathy. World Neurosurg. 2018;116:e1007-e1014. [15] HUANG Y, LAN Z, XU W. Analysis of sagittal alignment parameters following anterior cervical hybrid decompression and fusion of multilevel cervical Spondylotic myelopathy. BMC Musculoskelet Disord. 2019;20(1):1. [16] LEE SH, SON DW, LEE JS, et al. Differences in Cervical Sagittal Alignment Changes in Patients Undergoing Laminoplasty and Anterior Cervical Discectomy and Fusion. Neurospine. 2018;15(1):91-100. [17] SAKAI K, YOSHII T, HIRAI T, et al. Impact of the surgical treatment for degenerative cervical myelopathy on the preoperative cervical sagittal balance: a review of prospective comparative cohort between anterior decompression with fusion and laminoplasty. Eur Spine J. 2017;26(1):104-112. [18] SHI JS, LIN B, XUE C, et al. Clinical and radiological outcomes following hybrid surgery in the treatment of multi-level cervical spondylosis: over a 2-year follow-up. J Orthop Surg Res. 2015;10:185. [19] LU VM, ZHANG L, SCHERMAN DB, et al. Treating multi-level cervical disc disease with hybrid surgery compared to anterior cervical discectomy and fusion: a systematic review and meta-analysis. Eur Spine J. 2017;26(2):546-557. [20] SASSO RC, ANDERSON PA, RIEW KD, et al. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am. 2011; 93(18):1684-1692. [21] BARBAGALLO GM, ASSIETTI R, CORBINO L, et al. Early results and review of the literature of a novel hybrid surgical technique combining cervical arthrodesis and disc arthroplasty for treating multilevel degenerative disc disease: opposite or complementary techniques? Eur Spine J. 2009;18 Suppl 1:29-39. [22] HEY HW, HONG CC, LONG AS, et al. Is hybrid surgery of the cervical spine a good balance between fusion and arthroplasty? Pilot results from a single surgeon series. Eur Spine J. 2013;22(1):116-122. [23] HWANG SH, KAYANJA M, MILKS RA, et al. Biomechanical comparison of adjacent segmental motion after ventral cervical fixation with varying angles of lordosis. Spine J. 2007;7(2):216-221. [24] MATSUMOTO M, TOYAMA Y, ISHIKAWA M, et al. Increased signal intensity of the spinal cord on magnetic resonance images in cervical compressive myelopathy. Does it predict the outcome of conservative treatment? Spine (Phila Pa 1976). 2000;25(6):677-682. [25] JACK A, HARDY SG, NATARAJ A. Adjacent Segment Pathology: Progressive Disease Course or a Product of Iatrogenic Fusion? Can J Neurol Sci. 2017; 44(1):78-82. [26] MALDONADO CV, PAZ RD, MARTIN CB. Adjacent-level degeneration after cervical disc arthroplasty versus fusion. Eur Spine J. 2011;20 Suppl 3:403-407. [27] LOUIE PK, PRESCIUTTI SM, IANTORNO SE, et al. There is no increased risk of adjacent segment disease at the cervicothoracic junction following an anterior cervical discectomy and fusion to C7. Spine J. 2017;17(9): 1264-1271. [28] SPANOS SL, SIASIOS ID, DIMOPOULOS VG, et al. Correlation of Clinical and Radiological Outcome After Anterior Cervical Discectomy and Fusion With a Polyetheretherketone Cage. J Clin Med Res. 2018;10(3):268-276. [29] YANG X, BARTELS R, DONK R, et al. The association of cervical sagittal alignment with adjacent segment degeneration. Eur Spine J.2019.doi: 10.1007/s00586-019-06157-0. [30] AMENT JD, YANG Z, NUNLEY P, et al. Cost Utility Analysis of the Cervical Artificial Disc vs Fusion for the Treatment of 2-Level Symptomatic Degenerative Disc Disease: 5-Year Follow-up. Neurosurgery. 2016;79(1): 135-145. [31] QURESHI SA, MCANANY S, GOZ V, et al. Cost-effectiveness analysis: comparing single-level cervical disc replacement and single-level anterior cervical discectomy and fusion: clinical article. J Neurosurg Spine. 2013; 19(5):546-554. |
| [1] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [2] | Jiang Yong, Luo Yi, Ding Yongli, Zhou Yong, Min Li, Tang Fan, Zhang Wenli, Duan Hong, Tu Chongqi. Von Mises stress on the influence of pelvic stability by precise sacral resection and clinical validation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1318-1323. |
| [3] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [4] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [5] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [6] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [7] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [8] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [9] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [10] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [11] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [12] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [13] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [14] | Zhang Shangpu, Ju Xiaodong, Song Hengyi, Dong Zhi, Wang Chen, Sun Guodong. Arthroscopic suture bridge technique with suture anchor in the treatment of acromioclavicular dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1417-1422. |
| [15] | Liang Yan, Zhao Yongfei, Xu Shuai, Zhu Zhenqi, Wang Kaifeng, Liu Haiying, Mao Keya. Imaging evaluation of short-segment fixation and fusion for degenerative lumbar scoliosis assisted by highly selective nerve root block [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1423-1427. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||