Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (28): 4587-4592.doi: 10.12307/2022.318
Application of customized orthopedic insoles in the treatment of flatfoot
Zhou Xiangying1, Zeng Qing1, Liao Zhengwen1, Lu Pengcheng1, Zou Jihua2, Li Shilin1, Huang Guozhi1, 2
- 1Department of Rehabilitation Medicine, Zhujiang Hospital of Southern Medical University, Guangzhou 510280, Guangdong Province, China; 2Medical College of Rehabilitation, Southern Medical University, Guangzhou 510280, Guangdong Province, China
-
Received:2021-02-08Accepted:2021-03-31Online:2022-10-08Published:2022-03-24 -
Contact:Huang Guozhi, Chief physician, Doctoral supervisor, Department of Rehabilitation Medicine, Zhujiang Hospital of Southern Medical University, Guangzhou 510280, Guangdong Province, China; Medical College of Rehabilitation, Southern Medical University, Guangzhou 510280, Guangdong Province, China -
About author:Zhou Xiangying, Master candidate, Department of Rehabilitation Medicine, Zhujiang Hospital of Southern Medical University, Guangzhou 510280, Guangdong Province, China -
Supported by:the National Natural Science Foundation of China (General Program), No. 81874032 , No. 82072528 (to HGZ); the National Natural Science Foundation of China (Youth Program), No. 82002380 (to ZQ)
CLC Number:
Cite this article
Zhou Xiangying, Zeng Qing, Liao Zhengwen, Lu Pengcheng, Zou Jihua, Li Shilin, Huang Guozhi. Application of customized orthopedic insoles in the treatment of flatfoot[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(28): 4587-4592.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
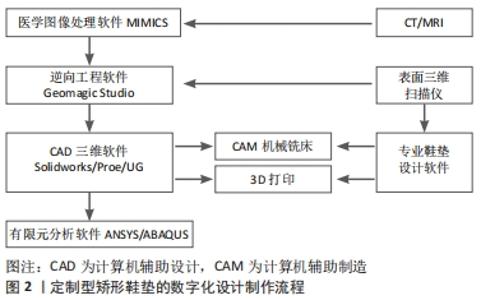
2.1 定制型矫形鞋垫治疗扁平足的设计原理 足弓是由跗骨、跖骨以及足底韧带和肌腱共同组成的复合体结构,可分为前后方向的外侧纵弓、内侧纵弓和内外方向的横弓,其中内侧纵弓包括跟骨、距骨、舟骨、3块楔形骨和1-3跖骨,其位置较高、弹性好,类似弹簧,能发生形变,将压力转换为弹性势能,再通过形变释放出去,在人体走动、跑跳的过程中起到缓冲减震和能量传递的作用[1]。正常步态周期中,在支撑相早期(足跟触地到承重期),胫骨后肌和腓肠肌等肌肉收缩,距下关节旋前,使跗骨间关节放松,有利于足迅速适应凹凸不平的地面;当足跟离地时,距下关节旋后,跗骨间关节锁定,在足底腱膜的作用下足骨紧密排列并固定,使足转变为刚性杠杆向前推进。而扁平足患者异常的足弓形态和功能干扰了足部节段性多关节连锁活动,引起局部应力增大,导致前足旋前外展、跟骨外翻[14-15]。有研究使用22具新鲜冰冻尸体进行体内实验模拟步行时足踝运动情况,证实了扁平足时跟骨相对于胫骨有更明显的外翻(11.1±2.8)°和外旋(8.1±4.0)°,正常情况下分别为(5.8±2.3)°和(2.3±1.7)°[16]。显然,这增加了踝关节的不稳定性,并通过运动链累及下肢甚至躯干生物力线偏离,而关节间的异常运动和碰撞往往会引起局部组织水肿和炎症,诱发疼痛和姿势异常[17],若这种异常受力模式长期未加以规范,还将导致软骨受损,形成难以逆转的结局。定制型矫形鞋垫旨在支撑并代偿足弓结构,限制后足活动范围,以重新建立理想的足底应力分布和纠正运动力线。 2.1.1 材料选择 热塑性聚氨酯、乙烯醋酸乙烯酯和聚乙烯是常用的矫形鞋垫制作材料。除了有研究表明材质更硬的鞋垫可以增加足底感觉输入,从而增加姿势稳定性外[18],定制矫形鞋垫材料的硬度主要影响其减震、支撑足弓效果和使用感受[19]。有学者使用数十种不同硬度的热塑性聚氨酯材料进行实验,发现优质的矫形鞋垫材料可以有效缓冲受试者在站立和行走时承受的足底压力负荷(分别为16%和19%),并指出体质量指数越高的受试者要达到最优缓冲效果所需的材料硬度越高[20]。苏宏伦等[21]比较了3种材料硬度(30,35,42度)的定制矫形鞋垫对1名扁平足儿童的矫正效果,发现在矫形鞋垫内侧纵弓高度相同的前提下,越硬的材料支撑力越好,抬高舟骨效果最明显,最能改善足弓塌陷的形态,也使足底峰值压强最大,同时由于足部活动范围受鞋垫硬度限制,硬度越高的矫形鞋垫给患者带来的不适感也越强[22]。因此要根据患者查体结果选择合适的材料,以求在支撑强度、减震能力与使用舒适感之间达到平衡。 2.1.2 形状设计 矫形鞋垫的几何形状设计比材料选择更能影响矫形鞋垫功能[23],需针对扁平足结构异常进行矫形鞋垫形状设计,主要包括以下两种:①内侧足弓支撑设计:足弓垫的拱形结构可向上托起足弓,一方面增加内侧足弓与矫形鞋垫接触面积,降低前足和足跟峰值压力,分散局部过大应力[24-25];另一方面可抬高舟骨、内侧楔骨及跟骨高度[26],帮助维持正常的足弓形态,使足弓能正常发挥作用,改善足踝关节活动度[27]。苏宏伦等[21]比较了3种高度的足弓垫设计对受试者舟骨高度和足底压力分布的影响,发现足弓垫越高抬高舟骨高度效果越明显,并提到类型①的鞋垫设计改善足底压力分布效果最明显,舒适度最高,但并未描述该类鞋垫具体的足弓高度参数。②后足深跟杯设计:向下凹陷的深跟杯可以限制距下关节过度旋前,减少后足软组织移位,使足跟脂肪垫的厚度增加[28],起到良好的缓冲减震作用,有利于减小后足跟骨应力,降低足跟峰值压力[29]。LI等[30]为16例患者设计了厚度为5 mm的尼龙材质足跟杯鞋垫,穿戴4周后患者足跟痛症状明显改善。定制扁平足矫形鞋垫多兼具两种设计,有研究表明每日坚持佩戴足弓支撑和跟杯鞋垫4 h及以上,持续8周后老年受试者站立平衡得到有效改善[31],而姿势稳定性下降也是部分扁平足患者存在的问题[32]。 2.2 定制型矫形鞋垫的设计制作过程 定制型矫形鞋垫的制作流程包括对患者的检查、诊断、患足数据采集、矫形鞋垫设计、鞋垫材料选择和制作、加工后处理、患者适配、效果监测和反馈。过去矫形鞋垫的个性化定制主要由传统手工制作完成,其使用效果明显依赖于矫形师制作水平及临床经验;如今随着各类计算机软件、相关医疗设备和3D打印等技术的发展,定制型矫形鞋垫的设计制作更趋于数字化和精确化[33],见图2。"
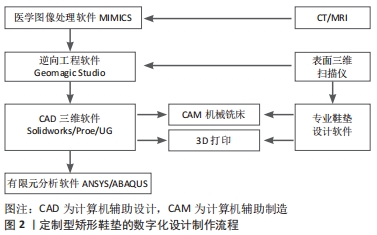

2.2.1 定制型矫形鞋垫的传统制作 传统定制型矫形鞋垫制作过程繁琐且精确度不足,患足数据采集是通过石膏模型实现的,在阴模凝固干燥的过程中矫形师需要用手控制患足姿势,以保持距下关节中立位,同时注意避免患者皮肤被灼伤,然后将阴模剪开取下,灌注石膏再次待其凝固干燥取得阳模。接着选用合适的材料,比对石膏阳模来裁剪、黏合、塑形和打磨。矫形技师需凭借个人经验和感觉来把握打磨的“度”。 2.2.2 定制型矫形鞋垫的数字化制作 数据采集和矫形鞋垫设计方法:近年来随着医疗设备和相关软件的开发,患足数据采集和矫形鞋垫设计方法有了新的改变,一类是利用患者的CT、MRI检查的原始图像数据[34],于医学图像处理软件MIMICS中重建形成STL格式的三维网格模型,再导入逆向工程软件Geomagic Studio中进行去特征、平滑和精确曲面等处理,形成足的曲面模型,再利用如Solidworks,UG等计算机辅助设计三维软件修改为矫形鞋垫实体模型[35]。甚至可以选择进一步建立有限元模型,将模型导入 ABAQUS 或ANSYS 分析软件中,赋予材料属性、网格划分、设立约束和载荷等操作,模拟在双足负重站立位下不同设计方案的矫形鞋垫对足底压力的影响[36],再依据受力分析结果选择和优化矫形鞋垫。上述设计建模方式需要熟练掌握多种软件,对临床医生或矫形师来说是新的挑战。另一类是利用三维表面扫描仪来获得足底数据,将足的体表轮廓3D模型呈现在计算机上以供查看和分析,相当于直接获得“阳模”,还可使用专用于设计矫形鞋垫的软件,与扫描仪配套使用,简化了矫形鞋垫设计过程。TELFER等[37]对使用扫描仪来观察不同负重水平下足部尺寸变化的38项研究进行了荟萃分析,认为使用扫描仪来获取足部表面轮廓数字特征是精确且可重复的。 制作:设计好的矫形鞋垫模型通过计算机数值控制(简称数控,是计算机辅助制造的核心)机械铣床以切削雕刻板材的方式耗时数分钟即可完成[38];也可使用3D打印技术以分层叠加、堆积成型的方式将其打印出来;前者常用的材料有乙烯醋酸乙烯酯和聚丙烯板材,后者常用的打印耗材包括乙烯醋酸乙烯酯线材和聚乳酸、热塑性聚氨酯等高弹性高分子塑料[20],打印工艺多使用选择性激光烧结、熔融沉积成型或立体光固化技术,选择不同的打印材料和打印参数可以获得不同硬度和结构的矫形鞋垫[20]。打印好的矫形鞋垫经过简单的打磨,再添上吸汗耐磨的衬布即可进行患者适配。但相比臻于至善的传统发泡鞋材,3D打印鞋垫的舒适度仍受限于可选择材料种类和性能,如SALLES等[39]招募38名(19对)受试者使用选择性激光烧结工艺和尼龙-12粉末分别打印两种形状的矫形鞋垫,尽管研究者出于盲法和改善舒适度的考虑,在打印好的矫形鞋垫表面添加了一层聚氨酯泡沫,但仍有 4 名受试者因鞋垫舒适度欠佳中途退出试验,而其余坚持穿戴矫形鞋垫3 个月的受试者中也有较多人表示未能完全适应鞋垫,尤其是鞋垫的足弓区域使其产生被侵入感且过于僵硬,不舒适评分最高。 2.3 定制型矫形鞋垫在不同年龄扁平足人群中的临床研究 2.3.1 定制型矫形鞋垫治疗儿童青少年扁平足 对于儿童青少年扁平足,学者们首先关注患儿是否需要进行矫形鞋垫干预。早在1957年,一项关于490名儿童足印的调查分析发现[40],10岁前大部分患儿扁平足为生理性扁平足,其患病率随年龄增长明显下降(18个月以下为97% ,10-11岁为4%)。2006年,MARTIN等[41]依据足弓形态和后足外翻角度对835名3-6岁儿童进行扁平足诊断及分型,发现柔韧性扁平足(5°≤后足外翻角≤20°)患病率为44%,病理性扁平足(后足外翻角>20°或踮脚站立时仍无足弓)患病率<1%,但接受矫形鞋垫干预的患儿占比为10%,同时发现6岁组扁平足患病率较3岁组明显下降(由54%降至24%),因此认为随着年龄增长,骨骼、肌肉、肌腱和韧带发育成熟,儿童扁平足患者的足弓结构能够恢复正常,超过90%的患儿无需接受治疗,只需观察,使用矫形鞋垫是一种过度干预。而BRESNAHAN等[42]认为儿童扁平足不应当被忽视,它不是孤立存在的,结构对线不良的足每走一步都会造成组织紧张和进一步的关节损伤,越早制定有效的治疗方案对身体其他部位损害越小。目前证据表明,对无症状扁平足儿童进行连续定期的观察是安全和适当的,对于已表现出疼痛、易疲劳、步态异常、平衡不良、运动功能障碍和活动退缩等症状的扁平足患儿,应及时接受矫形鞋垫治疗,该决定不受患儿年龄及体质量的影响[43-44]。 其次,学者们关注定制型矫形鞋垫对扁平足患儿疼痛、步态异常等临床症状的改善。HSIEH等[45]和LEE等[46]通过12周随访干预发现,定制矫形鞋垫显著减少了扁平足患儿的足部疼痛程度和频率,并改善了其平衡功能、转移能力和基本活动能力。SINHA等[47]以疼痛缓解或后足外翻改善作为随访终点(若改善不明显,最长限定2年),发现定制内侧足弓矫形鞋垫组(n=55)较对照组(n=26)明显缩短了平均随访周期(9个月 vs. 18个月,P=0.003)。GALAFATE等[48]招募了12例唐氏综合征并发双侧扁平足青少年患者,记录了他们在赤脚或穿有矫形鞋垫的鞋两种情况下的步态时空参数及骨盆和髋膝踝关节的矢状运动图,发现穿着矫形鞋垫使足部进展角显著改变,瞬时步态质量改善,而其余关节运动学及步态时域数据无明显改变。JAFARNEZHADGERO团队利用三维运动系统开展了多项试验[49-51],发现扁平足患儿穿戴定制型矫形鞋垫行走时可以差异性地改变优势侧和非优势侧踝、膝、髋关节的瞬时三维力矩[49];通过自身前后对照则发现穿戴定制型矫形鞋垫行走可减少额平面髋关节弯曲力矩的不对称,但对踝关节和膝关节的不对称无明显影响[50];另一项干预周期为4个月的随机对照试验发现,长期使用足弓支撑矫形鞋垫对踝、膝关节的旋转角度有明显影响,患儿步行过程中下肢生物力线偏移得到改善[51]。在上述接受中-长期定制型矫形鞋垫干预的试验中,患儿疼痛症状得到不同程度地改善,具有一致性趋势;而以穿戴矫形鞋垫前后行走时步态或足踝膝关节运动改变为研究终点的试验中,矫形鞋垫的瞬时有效性在不同试验中其结果存在差异,但较长时间矫形鞋垫干预对扁平足患儿的下肢生物力线亦有改善作用。此外,学者还研究了不同设计方案对平足儿童步行时足底压力的影响。BOK等[52]发现与仅穿鞋的对照组相比,定制矫形鞋垫可以显著降低患儿的前足内侧和后足处峰值压力,但不同角度刚性矫形鞋垫的效果无明显组间差异。弓太生等[53]根据6例轻度扁平足患儿的足部三维数据,分别设计了足弓高度为7,9,11 mm的矫形鞋垫模型,并选用邵氏硬度60度的乙烯醋酸乙烯酯材料定制矫形鞋垫,发现佩戴后患儿的足弓支撑力、足弓压强及足弓接触面积占比都随着足弓高度的增加而增大,且受试患儿穿戴3种矫形鞋垫测试时均无异常感和疼痛感,这可能与儿童足骨骼细小、软组织比重大、对异物更具包容性有关。 但是穿戴矫形鞋垫能否影响扁平足患儿肌骨形态结构,改变其自然病程仍是一个疑问。金宗学[54]通过肌骨超声检查发现,扁平足男童在接受矫形鞋垫干预4个月后其胫骨前肌、踇展肌横截面积增大,且其足舟骨、距骨高度增加,距舟关节角度减小,效果强于运动干预组,仅次于矫形鞋垫联合运动干预组。YOUN等[55]回顾了42例扁平足儿童长期(>4年)佩戴定制型矫形鞋垫的放射学影像结果变化,发现患儿们距骨和跟骨位置变化明显,中足和后足对齐方式趋于正常,但遗憾的是该试验缺乏对照组,无法解释该现象是否与幼儿足弓正常发育有关,且没有评估疼痛等临床症状,无法得出放射线指标的改善是否与症状的改变有关的结论。KANATLI等[56]对45例扁平足患儿进行了长期随访(24-57个月),发现定制矫形鞋垫干预组和空白对照组患儿的距骨-第一跖骨角、距跟角均有减小,而无组间差异,因此认为定制型矫形鞋垫不能改变扁平足患儿自然病程,其骨性结构的改善是足弓发育的结果。上述3个试验中患儿年龄分别为9-10岁[54]、大于6岁[55]、平均39.5个月龄(17-72个月龄)[56],患儿足部骨性结构排列均趋于改善,但得出的结论却不相同,这与CHOI等[57]的观点一致,当纳入的扁平足患儿年龄过小时会使得足弓正常发育这一因素对矫形鞋垫的治疗效果造成干扰。在0-6岁足弓发育高峰期,矫形鞋垫带来的肌骨形态结构层面的受益相比于足弓正常发育带来的影响可能是易被忽略的,因此研究纳入扁平足受试儿童年龄范围以从正常生理平足减少的年龄(10岁左右)到足部发育结束的年龄(13-15岁)为佳。 此外,在长达数年的随访试验中,矫形鞋垫的磨损情况和更换情况是否会影响穿戴效果往往被忽略。基于以上试验结果,在评估长期使用矫形鞋垫是否有助于扁平足患儿足部结构改善时应开展年龄分组更细致的临床试验,并定期检查矫形鞋垫状态,及时更换不适用的矫形鞋垫。 2.3.2 定制型矫形鞋垫治疗成人扁平足 对于成人扁平足而言,矫形鞋垫治疗不可能有助于扁平足的根治,其使用目的在于改善临床症状和降低可能的活动损伤风险。YURT等[58]将受试者分为基于计算机辅助设计/计算机辅助制造技术的数字化定制矫形鞋垫、传统定制矫形鞋垫及平鞋垫3组,并结合家庭锻炼方案,2个月后评估发现3组受试者生活质量评分均有提高,且2组定制矫形鞋垫患者疼痛症状得到有效缓解。LEE等[59]招募12名足旋前(足姿指数为6-12分)跑步爱好者,让其分别在无矫形鞋垫和穿戴传统手工定制矫形鞋垫情况下于实验室跑道奔跑,发现穿戴矫形鞋垫后踝关节跖屈力矩和跟腱负荷峰值缩小,其机制可能是矫形鞋垫通过抬高跟骨高度、减少后足外翻、避免跟腱过度拉长而减小跟腱承受的应力或剪切力,这有利于降低跟腱病发生风险。 HATFIELD等[60]招募了26例扁平足合并膝骨关节炎的老年患者,分别以穿鞋、穿外侧楔形鞋垫+鞋和穿外侧楔形附定制足弓垫+鞋3种方式行走,且3种方式行走顺序随机分配,结果发现穿外侧楔形鞋垫+鞋与只穿鞋不佩戴鞋垫相比,虽然使膝关节内收力矩减小、内侧胫股间室负荷减轻,但也导致踝关节和距下关节外翻加重,踝关节额外负担增加;而穿戴定制鞋垫行走时,在检测到膝关节内收力矩明显减小的情况下还能减轻踝关节平面外翻和前足外展,优化了瞬时步态且具有更高的即时舒适性,这意味着使用定制型矫形鞋垫能帮助扁平足合并膝骨关节炎患者减小加重膝关节或踝关节损伤的可能性。AMINIAN等[61]使用橡胶定制的楔形矫形鞋垫和乙烯醋酸乙烯酯材料的预制型矫形鞋垫进行对比,发现两者在与足的接触面积上无明显区别,但定制矫形鞋垫较预制型矫形鞋垫降低了中足压力峰值,因此推断可能是定制型矫形鞋垫的材料选择和形状设计强化足的本体感觉刺激,通过神经调节改变了肌肉收缩,达到分散足底压力的作用,而通过减小地面垂直作用力,肌肉收缩产生的动力能更有效地转化为向前的推进力,显著降低上坡和下坡行走时峰值摄氧量,减轻股直肌疲劳程度,使得人体能量利用率增高,肌肉损伤风险减小[62]。此外,有学者对定制矫形鞋垫的设计制作方案进行了创新。BARATI等[63]为患者定制了流体动力鞋垫,该款鞋垫能够在步行过程中根据压力中心的转移情况动态调整足弓高度,结果显示患者10周后在行走速度、步长和内侧纵弓移动参数上有显著改变,这可能意味着患者足功能改善,但遗憾的是该试验纳入人数仅3人。XU等[64]对佩戴3D打印矫形鞋垫的扁平足患者进行了为期8周的观察,并与预制型矫形鞋垫进行比较,发现在每天佩戴6-8 h的情况下两者均能重新分配足底压力作用,减轻不适症状,同时3D打印矫形鞋垫具有更高的舒适度。LIN等[65]纳入12例扁平足患者选用聚乙烯为他们制作3D打印矫形鞋垫,发现受试者的最大踝关节外翻力矩和最大外旋力矩分别降低了35%和16%,改变了受试者踝关节的瞬间步态。计算机辅助设计技术和3D打印相结合具有高精度结构制造的优势,有助于研究不同梯度矫形鞋垫设计的剂量-反应关系。TELFER等[66]纳入24名受试者,包括12名患者和对应的12名对照组,采集其数据进行矫形鞋垫设计,再根据该设计修改为后足角度成梯度改变的鞋垫(从6°高的内侧垫,以2°递减至平坦,再以2°递增至10°高的外侧垫),发现随足跟垫角度改变,后足外翻角度、踝关节外翻力矩和膝关节内收力矩具有线性改变,且踝关节内收角度和膝关节内收力矩存在组间差异。此外,有限元分析法通过模拟不同矫形鞋垫设计方案对扁平足的生物力学效应,为最优矫形鞋垫设计方案的选择提供了新的思路[36,67]。 与儿童组相比,成人组研究干预时间较短,观察指标以比较穿戴矫形鞋垫前后步行或活动时运动学参数的瞬时差异,以及短期干预后穿戴矫形鞋垫时患者主观感受改变为主,同时将定制型和预制型矫形鞋垫进行直接比较的文献数量较少,大部分研究者选择自身前后对照,或采用空白(仅穿鞋)及假干预(普通平坦的鞋垫)作为对照组。而在不同研究中由于患者个体情况和矫形鞋垫制作者的个人经验差异,定制型矫形鞋垫采用的材料、厚度、足弓支撑高度等设计方案并不一致,这导致某一项研究的结果并不能直接进行推广,将不同研究结果进行合并分析的可行性也较低。"

| [1] FLORES DV, MEJIA GC, FERNANDEZ HM, et al. Adult Acquired Flatfoot Deformity: Anatomy, Biomechanics, Staging, and Imaging Findings. Radiographics. 2019; 39(5):1437-1460. [2] EVANS A, ROME K. A Cochrane review of the evidence for non-surgical interventions for flexible pediatric flat feet. Eur J Phys Rehabil Med. 2011;47(1): 69-89. [3] LING S, LUI T. Posterior Tibial Tendon Dysfunction: An Overview. Open Orthop J. 2017;11:714-723. [4] SMYTH N, AIYER A, KAPLAN J, et al. Adult-acquired flatfoot deformity. Eur J Orthop Surg Traumatol. 2017;27(4):433-439. [5] WINKELMANN Z, ANDERSON D, GAMES K, et al. Risk Factors for Medial Tibial Stress Syndrome in Active Individuals: An Evidence-Based Review. J Athl Train. 2016;51(12):1049-1052. [6] KOSASHVILI Y, FRIDMAN T, BACKSTEIN D, et al. The correlation between pes planus and anterior knee or intermittent low back pain. Foot Ankle Int. 2008; 29(9):910-913. [7] KHAMIS A, YIZHAR A. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture.2007;25(1):127-134. [8] ELATAAR F, ABDELMAJEED S, ABDELLATIF N, et al. Core muscles’ endurance in flexible flatfeet: A cross - sectional study. J Musculoskelet Neuronal Interact. 2020;20(3):404-410. [9] MENZ H, DUFOUR A, RISKOWSKI J, et al. Foot posture, foot function and low back pain: the Framingham Foot Study. Rheumatology (Oxford). 2013;52(12):2275-2282. [10] ROSS M, SMITH M, PLINSINGA M, et al. Self-reported social and activity restrictions accompany local impairments in posterior tibial tendon dysfunction: a systematic review. J Foot Ankle Res. 2018;11:49-60. [11] 胡智宏,叶倩,孔叶平.矫形鞋垫的作用机制及临床研究进展[J].中国康复, 2016,31(3):229-231. [12] BANWELL H, THEWLIS D, MACKINTOSH S. Adults with flexible pes planus and the approach to the prescription of customised foot orthoses in clinical practice: A clinical records audit. Foot (Edinb). 2015;25(2):101-109. [13] 张新语,邢新阳,霍洪峰.矫正鞋垫的设计原理与生物力学功能[J].中国组织工程研究,2020,24(23):3744-3750. [14] DECESAR N, SHAKOOR D, ROBERTS L, et al. Hindfoot alignment of adult acquired flatfoot deformity: A comparison of clinical assessment and weightbearing cone beam CT examinations. Foot Ankle Surg. 2018;25(6):790-797. [15] SHIN H, LEE J, KIM E, et al. Flatfoot deformity affected the kinematics of the foot and ankle in proportion to the severity of deformity. Gait Posture. 2019;72:123-128. [16] WATANABE K, KITAOKA H, FUJII T, et al. Posterior tibial tendon dysfunction and flatfoot: Analysis with simulated walking. Gait Posture. 2013;37(2):264-268. [17] HÖSL M, BÖHM H, MULTERER C, et al. Does excessive flatfoot deformity affect function? A comparison between symptomatic and asymptomatic flatfeet using the Oxford Foot Model. Gait Posture. 2014;39(1):23-28. [18] IGLESIAS M, BECERRO D, PALACIOS P. Impact of soft and hard insole density on postural stability in older adults. Geriatr Nurs. 2012;33(4): 264-271. [19] GERRARD J, BONANNO D, WHITTAKER G, et al. Effect of different orthotic materials on plantar pressures: a systematic review. J Foot Ankle Res. 2020;13(1): 35. [20] CHATZISTERGOS P, NAEMI R, HEALY A, et al. Subject Specific Optimisation of the Stiffness of Footwear Material for Maximum Plantar Pressure Reduction. Ann Biomed Eng. 2017;45(8):1929-1940. [21] 苏宏伦,郭俊超,莫中军,等.个性化扁平足矫形鞋垫的生物力学研究[J].医用生物力学,2016,31(6):490-494. [22] SHEYKHI-DOLAGH R, SAEEDI H, FARAHMAND B, et al. The influence of foot orthoses on foot mobility magnitude and arch height index in adults with flexible flat feet. Prosthet Orthot Int. 2015;39(3):190-196. [23] CHEUNG J, ZHANG M. Parametric design of pressure-relieving foot orthosis using statistics-based finite element method. Med Eng Phys. 2008;30(3):269-277. [24] TANG S, CHEN C, WU C, et al. The effects of total contact insole with forefoot medial posting on rearfoot movement and foot pressure distributions in patients with flexible flatfoot. Cli Neurol Neurosurg. 2015;129:8-11. [25] JIN H, XU R, WANG S, et al. Use of 3D-Printed Heel Support Insoles Based on Arch Lift Improves Foot Pressure Distribution in Healthy People. Med Sci Monit. 2019;25:7175-7181. [26] CHOI J, LEE D, KIM S, et al. Does the long-term use of medial arch support insole induce the radiographic structural changes for pediatric flexible flat foot? — A prospective comparative study. Foot Ankle Surg. 2019;26(4):449-454. [27] HAN K, BAE K, LEVINE N, et al. Biomechanical Effect of Foot Orthoses on Rearfoot Motions and Joint Moment Parameters in Patients with Flexible Flatfoot. Med Sci Monit. 2019;25:5920-5928. [28] OHUCHI H, CHAVEZ J, ALVAREZ C. Changes in calcaneal pitch and heel fat pad thickness in static weight bearing radiographs while wearing shoes with arch support and heel cup orthotics. Asia Pac J Sports Med Arthro Rehabil Technol. 2019;17:21-24. [29] PERHAMRE S, LUNDIN F, KLÄSSBO M, et al. A heel cup improves the function of the heel pad in Sever’s injury: effects on heel pad thickness, peak pressure and pain. Scand J Med Sci Sports. 2012;22(4): 516-522. [30] LI L, YANG L, YU F, et al. 3D printing individualized heel cup for improving the self-reported pain of plantar fasciitis. J Transl Med. 2018;16(1):167. [31] CHEN T, CHOU L, TSAI M, et al. Effectiveness of a heel cup with an arch support insole on the standing balance of the elderly. Clin Interv Aging. 2014;9:351-356. [32] KOSHINO Y, SAMUKAWA M, CHIDA S, et al. Postural Stability and Muscle Activation Onset during Double- to Single-Leg Stance Transition in Flat-Footed Individuals. J Sports Sci Med. 2020;19(4):662-669. [33] 曹萍,吴小高.3D打印技术在矫形鞋垫中的应用进展[J].中国康复理论与实践,2015,21(7):753-756. [34] PAUL S, SIVARASU S, MATHEW L. Customized Foot Orthosis Development by 3D Reconstruction of the CT Images[. Engineering. 2012;4(10):692-695. [35] SARIKHANI A, MOTALEBIZADEH A, ASIAEI S, et al. Studying Maximum Plantar Stress per Insole Design Using Foot CT-Scan Images of Hyperelastic Soft Tissues. Appl Bionics Biomech. 2016;2016:8985690. [36] 章浩伟,杨俊彦,刘颖,等.伴有足中关节炎的扁平足患者矫正鞋垫的生物力学研究[J].中国生物医学工程学报,2020,39(3):327-334. [37] TELFER S, WOODBURN J. The use of 3D surface scanning for the measurement and assessment of the human foot. J Foot Ankle Res. 2010;3(1):19. [38] HUANG C, LEE M, CHANG C. Computer-Aided Design and Manufacturing of Customized Insoles. IEEE Comput Graph Appl. 2011;31(2):74-79. [39] SALLES A, GYI D. An evaluation of personalised insoles developed using additive manufacturing. J Sports Sci. 2013;31(4):442-450. [40] MORLEY A. Knock-knee in children. BMJ. 1957;2(5051):976-979. [41] MARTIN P, RAINER K, THOMAS L, et al. Prevalence of flat foot in preschool-aged children. Pediatrics. 2006;118(2):634-639. [42] BRESNAHAN PJ, JUANTO MA. Pediatric Flatfeet—A Disease Entity That Demands Greater Attention and Treatment. Front Pediatr. 2020;8(19):1-9. [43] CARR J, YANG S, LATHER L. Pediatric Pes Planus: A State-of-the-Art Review. Pediatrics. 2016;137(3):e20151230. [44] DARS S, UDEN H, KUMAR S, et al. When, why and how foot orthoses (FOs) should be prescribed for children with flexible pes planus: A Delphi survey of podiatrists. Peer J. 2018;6:e4667. [45] HSIEH R, PENG H, LEE W. Short-term effects of customized arch support insoles on symptomatic flexible flatfoot in children: A randomized controlled trial. Medicine (Baltimore). 2018;97(20):e10655. [46] LEE H, LIM K, YOO J, et al. Effect of Custom-Molded Foot Orthoses on Foot Pain and Balance in Children With Symptomatic Flexible Flat Feet. Ann Rehabil Med. 2015;39(6):905-913. [47] SINHA S, SONG H, KIM H, et al. Medial arch orthosis for paediatric flatfoot. J Orthop Surg. 2013;21(1):37-43. [48] GALAFATE D, POURNAJAF S, CONDOLUCI C, et al. Bilateral Foot Orthoses Elicit Changes in Gait Kinematics of Adolescents with Down Syndrome with Flatfoot. Int J Environ Res Public Health. 2020;17(14):1-9. [49] JAFARNEZHADGERO A, SHAD M, MAJLESI M. Effect of foot orthoses on the medial longitudinal arch in children with flexible flatfoot deformity: A three-dimensional moment analysis. Gait Posture. 2017;55:75-80. [50] JAFARNEZHADGERO A, MADADI SM, FERBER R. The effect of foot orthoses on joint moment asymmetry in male children with flexible flat feet. J Bodyw Mov Ther. 2018;22(1):83-89. [51] JAFARNEZHADGERO A, MADADI-SHAD M, ALAVI-MEHR S, et al. The long-term use of foot orthoses affects walking kinematics and kinetics of children with flexible flat feet: A randomized controlled trial PLoS One. 2018;13(10):e205187. [52] BOK S, LEE H, KIM B, et al. The Effect of Different Foot Orthosis Inverted Angles on Plantar Pressure in Children with Flexible Flatfeet. PLoS One. 2016;11(7): e159831. [53] 弓太生,韩珵琨,汤运启,等.扁平足儿童足弓支撑垫的设计与研究[J].中国皮革,2018,47(3):38-41. [54] 金宗学.矫形鞋垫和运动干预对9-10岁男童扁平足矫正效果及其机制[D].北京:北京体育大学,2018. [55] YOUN K, AHN S, KIM B, et al. Long-Term Effect of Rigid Foot Orthosis in Children Older Than Six Years With Flexible Flat Foot. Ann Rehabil Med. 2019;43(2):224-229. [56] KANATLı U, AKTAS E, YETKIN H. Do corrective shoes improve the development of the medial longitudinal arch in children with flexible flat feet? J Orthop Sci. 2016;21(5):662-666. [57] CHOI J, HONG W, SUH J, et al. The long-term structural effect of orthoses for pediatric flexible flat foot: A systematic review. Foot Ankle Surg. 2020;26(2):181-188. [58] YURT Y, ŞENER G, YAKUT Y. The effect of different foot orthoses on pain and health related quality of life in painful flexible flat foot: a randomized controlled trial. Eur J Phys Rehabil Med. 2019;55(1):95-102. [59] LEE K, LING S, YUNG P. Controlled trial to compare the Achilles tendon load during running in flatfeet participants using a customized arch support orthoses vs an orthotic heel lift. BMC Musculoskelet Disord. 2019;20(1):535. [60] HATFIELD G, COCHRANE C, TAKACS J, et al. Knee and ankle biomechanics with lateral wedges with and without a custom arch support in those with medial knee osteoarthritis and flat feet. J Orthop Res. 2016;34(9):1597-1605. [61] AMINIAN G, SAFAEEPOUR Z, FARHOODI M, et al. The effect of prefabricated and proprioceptive foot orthoses on plantar pressure distribution in patients with flexible flatfoot during walking. Prosthet Orthot Int. 2013;37(3):227-232. [62] HUANG Y, KIM K, SONG C, et al. How Arch Support Insoles Help Persons with Flatfoot on Uphill and Downhill Walking. J Healthc Eng. 2017;2017:9342789. [63] BARATI K, SAEEDI H, HAJIAGHAEI B, et al. The effect of hydrodynamic insole on foot kinematics in individuals with flexible flatfoot: Case series using a single-subject design. Proc Inst Mech Eng H. 2019; 233(4):407-413. [64] XU R, WANG Z, REN Z, et al. Comparative Study of the Effects of Customized 3D printed insole and Prefabricated Insole on Plantar Pressure and Comfort in Patients with Symptomatic Flatfoot. Med Sci Monit. 2019;25:3510-3519. [65] LIN K, HU C, YANG W, et al. Biomechanical Evaluation and Strength Test of 3D-Printed Foot Orthoses. Appl Bionics Biomech. 2019;2019:4989534. [66] TELFER S, ABBOTT M, STEULTJENS M, et al. Dose response effects of customised foot orthoses on lower limb kinematics and kinetics in pronated foot type. J Biomech. 2013;46(9):1489-1495. [67] SU S, MO Z, GUO J, et al. The Effect of Arch Height and Material Hardness of Personalized Insole on Correction and Tissues of Flatfoot. J Healthc Eng. 2017; 2017:8614341. [68] TANG C, NG KH, LAI J. Adult flatfoot. BMJ. 2020;368:m295. [69] GIJON-NOGUERON G, PALOMO-TOUCEDO I, GIL-TINOCO A, et al. Effect produced on ground reaction forces by a prefabricated, weight-bearing and non-weight-bearing foot orthosis in the treatment of pronated foot: Pilot study. Medicine (Baltimore). 2018;97(22):e10960. [70] KHODAEI B, SAEEDI H, JALALI M, et al. Comparison of plantar pressure distribution in CAD-CAM and prefabricated foot orthoses in patients with flexible flatfee. Foot (Edinb). 2017;33:76-80. [71] COBB S, TIS L, JOHNSON J. The Effect of 6 Weeks of Custom-molded Foot Orthosis Intervention on Postural Stability in Participants With ≥ 7 Degrees of Forefoot Varus. Clin J Sport Med. 2006;16(4):312-322. [72] TAHMASEBI R, KARIMI MT, SATVATI B, et al. Evaluation of standing stability in individuals with flatfeet. Foot Ankle Spec. 2015;8(3):168-174. |
| [1] | Pan Baoshun, Fang Zhen, Gao Mingjie, Fang Guiming, Chen Jinshui. Design for posterior atlantoaxial internal fixation system with fusion cage based on imaging data [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1372-1376. |
| [2] | Jing Jinpeng, Zhang Yue, Liu Xiaomin, Liu Yi. Traditional Chinese medicine injection for promoting blood circulation in prevention of deep vein thrombosis after orthopedic surgery: network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1467-1476. |
| [3] | Liu Gang, Ma Chao, Wang Le, Zeng Jie, Jiao Yong, Zhao Yi, Ren Jingpei, Hu Chuanyu, Xu Lin, Mu Xiaohong. Ankle-foot orthoses improve motor function of children with cerebral palsy: a Meta-analysis based on 12 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1299-1304. |
| [4] | Li Shuo, Su Peng, Zhang Li, Wu Qiulong, Hu Xiangyu, Lai Yuliang. Positive effect of supracondylar femoral osteotomy on the correction of knee varus based on three-dimensional reconstruction and finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 858-863. |
| [5] | Zhou Jianguo, Liu Shiwei, Yuan Changhong, Bi Shengrong, Yang Guoping, Hu Weiquan, Liu Hui, Qian Rui. Total knee arthroplasty with posterior cruciate ligament retaining prosthesis in the treatment of knee osteoarthritis with knee valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 892-897. |
| [6] | Song Yan, Zheng Kun, Wei Haoxin, Lu Dezhi, Xu Yuanjing, Wang Xiaowen, Wang Jinwu. reliability of flat feet evaluated by foot posture index and its application in three-dimensional printing insoles [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 344-349. |
| [7] | Zou Mengyao, Wang Junhua, Qin Pengfei, Zhong Weihua. Knowledge graph analysis of virtual reality technology in stroke treatment [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(26): 4224-4233. |
| [8] | Li Zhishuai, Zhang Hongqian, Liu Jianquan, Zhang Hankun, Li Li. Visualization analysis of current research hotspots on rehabilitation treatment after anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(26): 4234-4241. |
| [9] | Wang Hongyang, Li Xiaofeng, Zhou Zhuren, Li Hanpin, Cong Rijiao, Li Jianping. Antibody detection and cross-matching results in patients with ineffective platelet transfusion in Shenyang region [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(24): 3875-3879. |
| [10] | Tang Jixiang, Jing Lin, Zhang Hongmei, Yan Qi, Pan Li. Early and midterm effects of lower limb force line correction after mobile-bearing unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(18): 2834-2838. |
| [11] | Chen Xianxiang, Liao Shijie, Li Boxiang, Li Chong, Huang Qian, Lin Chengsen, Liu Yun, Lu Rongbin, Ding Xiaofei. Characteristics and application on animal models of different species of Perthes disease [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(18): 2922-2929. |
| [12] | You Kun, Liu Yuanxin. Protective effect of exercise preconditioning on lung injury induced by hypobaric hypoxia in rats based on the nuclear factor E2-related factor 2/antioxidant response element signal pathway [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(17): 2702-2707. |
| [13] | Zheng Kun, Xu Yuanjing, Yu Wenqiang, Ren Fuchao, Deng Qian, Wang Jinwu, Dai Kerong. Application of three-dimensional printing medical-industrial outpatient clinics in digital medical education [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(15): 2317-2322. |
| [14] | Wang Susu, Li Lifeng, Zhang Yimin. Visualization analysis on research progress and hotspots of exercise therapy for sarcopenia in older adults in recent decade [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(14): 2223-2230. |
| [15] | Wang Shuyun, Xie Junhui, Yu Xuefeng. Effect and mechanism of mesenchymal stem cells in the treatment of diabetic nephropathy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(1): 148-152. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||