[1] VAN DE WALL BJM, OCHEN Y, BEERES FJP, et al. Response to Yin et al regarding: “Conservative vs. operative treatment for humeral shaft fractures: a meta-analysis and systematic review of randomized clinical trials and observational studies”. J Shoulder Elbow Surg. 2021; 30(1):e32-e33.
[2] MAES V, PUTZEYS G. One-year follow-up after treatment of proximal and/or middle one-third humeral shaft fractures with a helical plate: healing rates, complications and functional outcome measures. BMC Musculoskelet Disord. 2021;22(1):890.
[3] VAN DE WALL BJM, BAUMGÄRTNER R, HOUWERT RM, et al. MIPO versus nailing for humeral shaft fractures: a meta-analysis and systematic review of randomised clinical trials and observational studies. Eur J Trauma Emerg Surg. 2022;48(1):47-59.
[4] 征华勇,高杰,郭永智,等.前外侧入路微创接骨板接骨术治疗肱骨中下段骨折的临床疗效[J].中华创伤杂志,2021,37(6):549-554.
[5] XUE Z, JIANG C, HU C, et al. Effects of different surgical techniques on mid-distal humeral shaft vascularity: open reduction and internal fixation versus minimally invasive plate osteosynthesis. BMC Musculoskelet Disord. 2016;17(1):370.
[6] MAHABIER KC, VAN LIESHOUT EM, VAN DER SCHAAF BC, et al. Reliability and Reproducibility of the OTA/AO Classification for Humeral Shaft Fractures. J Orthop Trauma. 2017;31(3):e75-e80.
[7] BEERES FJ, DIWERSI N, HOUWERT MR, et al. ORIF versus MIPO for humeral shaft fractures: a meta-analysis and systematic review of randomized clinical trials and observational studies. Injury. 2021;52(4): 653-663.
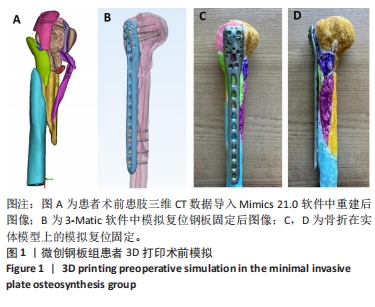
[8] HU C, QIU B, CEN C, et al. 3D printing assisted MIPO for treatment of complex middle-proximal humeral shaft fractures. BMC Musculoskelet Disord. 2024;25(1):93.
[9] 陈飞锋,陈丽娜,孟祥博,等.肱骨干骨折术后肘关节功能障碍康复及预后分析[J].浙江创伤外科,2022,27(5):837-838.
[10] NICOLACI G, MAES V, LOLLINO N, et al. How to treat proximal and middle one-third humeral shaft fractures: the role of helical plates. Musculoskelet Surg. 2023;107(2):231-238.
[11] WANG Q, HU J, GUAN J, et al. Proximal third humeral shaft fractures fixed with long helical PHILOS plates in elderly patients: benefit of pre-contouring plates on a 3D-printed model-a retrospective study. J Orthop Surg Res. 2018;13(1):203.
[12] GARCÍA-VIRTO V, SANTIAGO-MANIEGA S, LLORENTE-PERIS A, et al. MIPO helical pre-contoured plates in diaphyseal humeral fractures with proximal extension. Surgical technique and results. Injury. 2021; 52 Suppl 4:S125-S130.
[13] DENIES E, NIJS S, SERMON A, et al. Operative treatment of humeral shaft fractures. Comparison of plating and intramedullary nailing. Acta Orthop Belg. 2010;76(6):735-742.
[14] 任东,邢丹谋,张明,等.桥接组合内固定系统与锁定钉板系统治疗闭合性肱骨干骨折的疗效比较[J].中华骨科杂志,2022,42(3): 156-163.
[15] 熊晨,何贵平,张堃,等.保守治疗、切开复位及经皮微创接骨板内固定和髓内钉固定治疗肱骨干骨折的网状Meta分析[J].中国组织工程研究,2021,25(36):5878-5887.
[16] WANG Y, CHEN H, WANG L, et al. Comparison between osteosynthesis with interlocking nail and minimally invasive plating for proximal- and middle-thirds of humeral shaft fractures. Int Orthop. 2021;45(8): 2093-2102.
[17] 王延鹤,成金磊,吕飞飞,等.微创钢板接骨术与顺行交锁髓内钉内固定术治疗肱骨干骨折的临床疗效及安全性比较[J].临床和实验医学杂志,2023,22(14):1515-1519.
[18] 许志贤,何武兵,柯铁,等.微创钢板接骨术和交锁髓内钉内固定术治疗肱骨干骨折的疗效比较[J].创伤外科杂志,2022,24(3):192-197.
[19] BOILEAU P, D’OLLONNE T, BESSIÈRE C, et al. Displaced humeral surgical neck fractures: classification and results of third-generation percutaneous intramedullary nailing. J Shoulder Elbow Surg. 2019; 28(2):276-287.
[20] 王华松,姜壮,秦佳军,等.交锁髓内钉与锁定接骨板治疗老年内翻型肱骨近端骨折的疗效比较[J].中华创伤杂志,2021,37(12): 1105-1111.
[21] 王庆伟,王华松,石华峰,等.闭合复位髓内钉与切开复位锁定接骨板固定治疗肱骨中上段骨折的疗效比较[J].中华创伤骨科杂志, 2022,24(11):943-949.
[22] SHETTY MS, KUMAR MA, SUJAY K, et al. Minimally invasive plate osteosynthesis for humerus diaphyseal fractures. Indian J Orthop. 2011;45(6):520-526.
[23] CONCHA JM, SANDOVAL A, STREUBEL PN. Minimally invasive plate osteosynthesis for humeral shaft fractures: are results reproducible? Int Orthop. 2010;34(8):1297-1305.
[24] LODE I, NORDVISTE V, ERICHSEN JL, et al. Operative versus nonoperative treatment of humeral shaft fractures: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2020;29(12):2495-2504.
[25] BOGNER R, HÜBNER C, MATIS N, et al. Minimally-invasive treatment of three- and four-part fractures of the proximal humerus in elderly patients. J Bone Joint Surg Br. 2008;90(12):1602-1607.
[26] LI K, LIU Z, LI X, et al. 3D printing-assisted surgery for proximal humerus fractures: a systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2022;48(5):3493-503.
[27] CHEN C, CAI L, ZHENG W, et al. The efficacy of using 3D printing models in the treatment of fractures: a randomised clinical trial. BMC Musculoskelet Disord. 2019;20(1):65.
[28] ZHU D, ZHANG Z, ZHANG J, et al. The efcacy of 3D printing-assisted surgery in treating distal radius fractures: systematic review and metaanalysis. J Comp Ef Res. 2020;9(13):919-931.
[29] COOK A, BALDWIN P, FOWLER JR. Incidence of fexor pollicis longus complications following volar locking plate fxation of distal radius fractures. Hand (N Y). 2020;15(5):692-697.
[30] WAN SX, MENG FB, ZHANG J, et al. Experimental study and preliminary clinical application of mini-invasive percutaneous internal screw fxation for scaphoid fracture under the guidance of a 3D-printed guide plate. Curr Med Sci. 2019;39(6):990-996.
[31] DA SILVA T, RUMMEL F, KNOP C, et al. Comparing iatrogenic radial nerve lesions in humeral shaft fractures treated with helical or straight PHILOS plates: a 10-year retrospective cohort study of 62 cases. Arch Orthop Trauma Surg. 2020;140(12):1931-1937.
[32] CEN C, CAO Y, ZHANG Y, et al. Preoperative position and protection of radial nerve by B-ultrasound combined with MIPPO for treatment of middle-inferior humerus fractures. J Orthop Surg Res. 2022;17(1):260.
[33] 樊伟,宋哲,王晨,等. 单纯经皮微创钢板内固定技术与结合B超定位上臂神经治疗肱骨干中上段骨折的疗效比较[J].中华创伤骨科杂志,2021,23(8):669-673.
[34] BENNINGER E, MEIER C. Minimally invasive lateral plate placement for metadiaphyseal fractures of the humerus and its implications for the distal deltoid insertion- it is not only about the radial nerve. A cadaveric study. Injury. 2017;48(3):615-620.
[35] WANG Y, CHEN H, WANG L, et al. Comparison between osteosynthesis with interlocking nail and minimally invasive plating for proximal- and middle thirds of humeral shaft fractures. Int Orthop. 2021;45(8): 2093-2102.
[36] 任敬,贾斌,郑世成,等.交锁髓内钉内固定治疗肱骨干骨折临床研究[J].陕西医学杂志,2021,50(8):966-968,1030.
[37] 刘涛,查明建,柯荣军.第3代multiloc髓内针、普通弯型髓内针与肱骨近端锁定钢板治疗复杂肱骨近端骨折的比较[J].中国组织工程研究,2023,27(22):3537-3543.
[38] KONDA SR, SALEH H, FISHER N, et al. Humeral Shaft Fracture: Intramedullary Nailing. J Orthop Trauma. 2017;31 Suppl 3:S38.
[39] FAN Y, LI YW, ZHANG HB, et al. Management of Humeral Shaft Fractures With Intramedullary Interlocking Nail Versus Locking Compression Plate. Orthopedics. 2015;38(9):e825-e829.
[40] CHEN YN, CHANG CW, LIN CW, et al. Numerical investigation of fracture impaction in proximal humeral fracture fixation with locking plate and intramedullary nail. Int Orthop. 2017;41(7):1471-1480.
|