[1] SCHOLZ M, KANDZIORA F, KOBBE P, et al. Treatment of Axis Ring Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J. 2018; 8(2 Suppl):18S-24S.
[2] CHAUDHARY SB, MARTINEZ M, SHAH NP, et al. Traumatic atlantoaxial dislocation with Hangman fracture. Spine J. 2015;15(4):e15-e18.
[3] AL-MAHFOUDH R, BEAGRIE C, WOOLLEY E, et al. Management of Typical and Atypical Hangman’s Fractures . Global Spine J. 2016;6(3): 248-256.
[4] YUNDE A, FURUYA T, ORITA S, et al. Hangman’s Fracture in Geriatric Population: A Nationwide Multicenter Study in Japan. Global Spine J. 2023:21925682231216925. doi: 10.1177/21925682231216925.
[5] PROST S, BARREY C, BLONDEL B, et al. Hangman’s fracture: Management strategy and healing rate in a prospective multi-centre observational study of 34 patients. Orthop Traumatol Surg Res. 2019; 105(4):703-707.
[6] HUR H, LEE JK, JANG JW, et al. Is it feasible to treat unstable hangman’s fracture via the primary standard anterior retropharyngeal approach? Eur Spine J. 2014;23(8):1641-1647.
[7] LI S, DU J, HUANG Y, et al. Comparison of the efficacies of TINAVI robot-assisted surgery and conventional open surgery for Levine-Edward type IIA (postreduction) hangman fractures. Sci Rep. 2023;13(1):15934.
[8] 王清, 王松, 钟德君,等. 不稳定性Hangman骨折手术入路选择[J]. 中国脊柱脊髓杂志,2012,22(6):526-530.
[9] LI G, WANG Q, LIU H, et al. Individual Surgical Strategy Using Posterior Lag Screw-Rod Technique for Unstable Atypical Hangman’s Fracture Based on Different Fracture Patterns. World Neurosurg. 2018;119: e848-e854.
[10] ZHANG J, LI G, WANG Q. Is it feasible to treat unstable traumatic spondylolisthesis of the axis via posterior fixation without fusion? BMC Musculoskelet Disord. 2023;24(1):122.
[11] JEONG DH, YOU NK, LEE CK, et al. Posterior C2-C3 Fixation for Unstable Hangman’s Fracture. Korean J Spine. 2013;10(3):165-169.
[12] WANG S, WANG Q, YANG H, et al. A novel technique for unstable Hangman’s fracture: lag screw-rod (LSR) technique. Eur Spine J. 2017; 26(4):1284-1290.
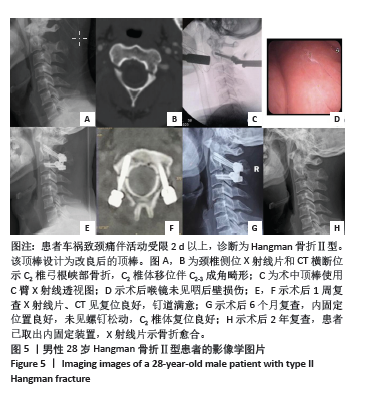
[13] 王高举, 王清, 王松,等. 后路椎弓根置钉顶棒技术治疗C2椎弓根骨折的疗效[J]. 中华创伤杂志,2017,33(4):327-331.
[14] LI G, YANG Y, LIU H, et al. Residual Deformity After Anterior Cervical Discectomy and Fusion for Unstable Hangman’s Fractures. World Neurosurg. 2017;108:216-224.
[15] MAGERL FP. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation . Clin Orthop Relat Res. 1984;(189):125-141.
[16] XIE N, KHOO LT, YUAN W, et al. Combined anterior C2-C3 fusion and C2 pedicle screw fixation for the treatment of unstable hangman’s fracture: a contrast to anterior approach only . Spine (Phila Pa 1976). 2010;35(6):613-619.
[17] LI Z, LI F, HOU S, et al. Anterior discectomy/corpectomy and fusion with internal fixation for the treatment of unstable hangman’s fractures: a retrospective study of 38 cases. J Neurosurg Spine. 2015;22(4): 387-393.
[18] BRISTOL R, HENN JS, DICKMAN CA. Pars screw fixation of a hangman’s fracture: technical case report. Neurosurgery. 2005;56(1 Suppl):E204; discussion E.
[19] MAHMOUD A, SHANMUGANATHAN K, MONTGOMERY A. Surgical Management of Hangman’s Fracture: A Systematic Review. Int J Spine Surg. 2023;17(3):454-467.
[20] 张帅,张引,李新武,等.两种非融合术式治疗Ⅱ型和Ⅱa型Hangman骨折的疗效比较[J]. 实用骨科杂志,2022,28(2):97-102.
[21] SEO HY, KO JH, PARK JB, et al. Anterior C2-3 fusion surgery alone for highly displaced Hangman’s fracture with severe angulation of C2-3 of more than 30° . Clin Neurol Neurosurg. 2021;206:106701.
[22] 勾瑞恩, 母心灵, 崔京福,等. 颈前路间盘切除植骨融合治疗不稳定Hangman骨折[J]. 中国矫形外科杂志,2021,29(14):1269-1272.
[23] 陈荣滋, 郑耿阳, 王顺民,等. C2/C3颈椎前路椎间盘切除融合术治疗Hangman骨折对下位颈椎椎间盘高度及颈椎曲度的影响[J]. 脊柱外科杂志,2021,19(6):411-415.
[24] 谭军,贾连顺,侯黎升,等. C2椎弓根拉力螺钉选择性治疗Hangman骨折[J]. 中华骨科杂志,2002,22(11):653-656.
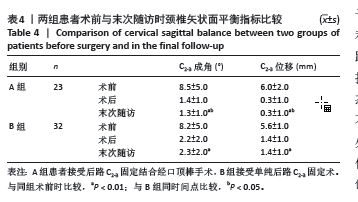
[25] JIN C, XIE N, REN Y, et al. How Does Cervical Sagittal Balance Change After Hangman Fracture Treated with Anterior or Posterior Approach Surgery? World Neurosurg. 2020;138:e767-e77.
[26] XU D, GAN K, WANG Y, et al. Comparison of C2-3 Pedicle Screw Fixation With C2 Spinous Muscle Complex and Iliac Bone Graft for Instable Hangman Fracture. Front Surg. 2021;8:723078.
[27] 阮汉江,金根洋,李新武,等.三种后路单节段固定方式治疗Ⅱ型Hangman骨折的生物力学性能[J]. 中国组织工程研究,2021,25(15): 2309-2314.
[28] DUGGAL N, CHAMBERLAIN RH, PEREZ-GARZA LE, et al. Hangman’s fracture: a biomechanical comparison of stabilization techniques. Spine (Phila Pa 1976). 2007;32(2):182-187.
[29] 徐昊,马迅. 手术治疗Ⅲ型Hangman骨折的研究进展[J]. 实用骨科杂志,2023,29(3):234-238.
[30] 张腾飞,梅伟. Hangman骨折的诊断与治疗进展[J]. 中国骨与关节杂志,2021,10(4):281-286.
[31] 方艳志, 徐志强, 迟寿远, 等. Hangman骨折两种气管插管全麻下短节段固定融合[J]. 中国矫形外科杂志,2023,31(16):1482-1487.
[32] LONG Z, YU H, YANG H, et al. Biomedical analysis of four fixation systems in treatment of type II traumatic spondylolisthesis of the axis: a finite element analysis. Med Biol Eng Comput. 2024;62(3):843-852.
[33] 雷舒澳, 王清, 李广州,等. 机动车事故致Hangman骨折的临床特征分析:一项基于多中心数据的回顾性研究[J]. 中国脊柱脊髓杂志, 2023,33(7):577-583.
[34] LI G, WANG Q. Application of novel self-designed surgical tools for the safe C2 pedicle screw placement in 12 patients with Hangman fracture. Asian J Surg. 2023;46(6):2419-2420.
[35] WANG J, CHEN H, CAO P, et al. Combined Anterior-Posterior Fixation and Fusion for Completely Dislocated Hangman’s Fracture: A Retrospective Analysis of 11 Cases. Clin Spine Surg. 2017;30(8): E1050-E1054.
[36] WANG G, JIANG D, WANG Q, et al. A novel technique using a pedicle screw and bucking bar for the treatment of hangman’s fracture. Orthop Traumatol Surg Res. 2019;105(4):709-711.
[37] IYER S, NEMANI VM, NGUYEN J, et al. Impact of Cervical Sagittal Alignment Parameters on Neck Disability. Spine (Phila Pa 1976). 2016; 41(5):371-377.
[38] EFFENDI B, ROY D, CORNISH B, et al. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg Br. 1981;63-B(3):319-327.
[39] TAKEUCHI K, YOKOYAMA T, ABURAKAWA S, et al. Inadvertent C2-C3 union after C1-C2 posterior fusion in adults. Eur Spine J. 2006;15(3): 270-277.
[40] 金晨, 任亦龙, 徐委,等. 两种不同手术方式治疗不稳定性Hangman骨折的疗效对比 [J]. 中国脊柱脊髓杂志,2020,30(1):20-29.
[41] KONG W, YANG X, LI Z, et al. Analysis of the Cervical Sagittal Alignment in Patients with Unstable Hangman Fracture Under C2-3 Anterior Discectomy and Fusion. World Neurosurg. 2020;137:e1-e8.
[42] 周虹羽, 汪姝玥, 王清,等. 解剖型顶棒辅助后路C2椎弓根钉内固定治疗寰枢椎不稳对咽后壁软组织的影响[J]. 中国骨与关节损伤杂志,2022,37(3):246-249. |