Chinese Journal of Tissue Engineering Research ›› 2014, Vol. 18 ›› Issue (20): 3212-3217.doi: 10.3969/j.issn.2095-4344.2014.20.018
Previous Articles Next Articles
Biomechanical and histological analysis of alveolar distraction osteogenesis in a canine model
Zhou Miao1, Che Yue-juan2, Guo Ming-yan2, Huang Dai-ying3, Piao Zheng-guo1, Yu Xiao-wei4, Chen Song-ling3
- 1Department of Oral and Maxillofacial Surgery, Stomatological Hospital, School of Stomatology, Research Institute of Stomatological Disease, Guangzhou Medical University, Guangzhou 510140, Guangdong Province, China; 2Department of Anesthesiology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou 510120, Guangdong Province, China; 3Department of Oral and Maxillofacial Surgery, the First Affiliated Hospital, Sun Yat-sen University, Guangzhou 510060, Guangdong Province, China; 4Department of Oral and Maxillofacial Surgery, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou 510120, Guangdong Province, China
-
Received:2014-03-21Online:2014-05-14Published:2014-05-14 -
Contact:Chen Song-ling, Professor, Department of Oral and Maxillofacial Surgery, the First Affiliated Hospital, Sun Yat-sen University, Guangzhou 510060, Guangdong Province, China -
About author:Zhou Miao, M.D., Attending physician, Department of Oral and Maxillofacial Surgery, Stomatological Hospital, School of Stomatology, Research Institute of Stomatological Disease, Guangzhou Medical University, Guangzhou 510140, Guangdong Province, China -
Supported by:the National Natural Science Foundation of China, No. 81000421; Key Program of Science and Technology Plan of Guangdong Province, No. 2004B33101010; ITI Fund, No. 881-2012
CLC Number:
Cite this article
Zhou Miao, Che Yue-juan, Guo Ming-yan, Huang Dai-ying, Piao Zheng-guo, Yu Xiao-wei, Chen Song-ling. Biomechanical and histological analysis of alveolar distraction osteogenesis in a canine model[J]. Chinese Journal of Tissue Engineering Research, 2014, 18(20): 3212-3217.
share this article

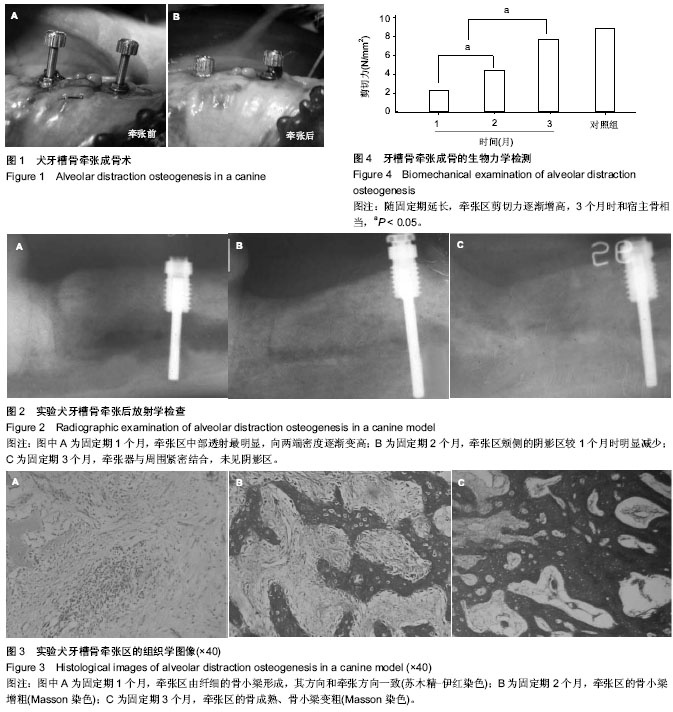
2.1 临床检查 所有的动物能耐受整个手术和牵张过程。有1只出现伤口感染导致牵张器排出,其余伤口愈合正常。固定期0,1,2和3个月的临床牙槽嵴增加高度值分别为(4.80±0.50) mm,(4.67±0.31) mm,(4.41±0.19) mm和(4.32±0.21) mm,增加高度随固定时间延长有所降低。在牵张后2个月复查,舌侧骨板触诊坚硬、连续性好。在整个观察期,唇侧骨面触诊粗糙。牙槽黏膜和牙龈颜色未出现明显改变。牵张器与周围组织愈合良好。 2.2 放射学检查 种植体植入后放射学检查显示牵张器就位良好,在输送盘和基骨间有约1 mm的阴影。所有的牵张器都可使输送盘增高,输送盘两端有明显的骨突。固定期1个月时,发现输送盘与基骨之间有明显的透射区,输送盘两端与基骨的界限变模糊,骨突明显变钝。颊侧的透射影比舌侧更明显。垂直向观察,牵张区中部透射最明显,向两端密度逐渐变高(图2A)。固定期2个月时,牵张区的阻射较1个月明显上升,牵张区与基骨和输送盘的界限隐约可见。输送盘两端的骨突与邻近骨连接平滑。牵张区的阻射为舌侧高于颊侧、两端高于中间(垂直向)。颊侧的阴影区较1个月时明显减少(图2B)。固定期3个月时,牵张区阻射较2个月又有提高。牵张区舌侧骨与基骨和输送盘阻射程度无分别。颊侧牵张区可见中间段向舌侧凹陷。螺纹杆周围骨质成明显阻射影。整个牵张器与周围骨紧密结合,未见阴影区(图2C)。固定期0,1,2和3个月的放射学牙槽嵴高度增加值分别是(5.12±0.67) mm,(4.92±0.57) mm,(4.73±0.46) mm和(4.58±0.35) mm,增加高度随固定时间延长而降低。 2.3 组织学检查 固定期1个月时,牵张区可见由3个区组成:与两边的宿主骨交界处为疏松的、网状骨小梁,中间为纤维组织区。牵张区未发现有软骨的存在,骨组织主要是由纤维组织中的间充质细胞直接分化为骨母细胞,再分化为成骨细胞产生新生骨,新生骨进一步改建、成熟。在骨小梁区,可看到靠近中间的部分较为幼稚,骨小梁纤细,有时在纤维组织中直接形成骨岛;在接近宿主骨的部分,骨小梁逐渐致密、粗大,并向板状骨过渡,形成陷窝状的编织骨。在新生骨小梁的周围有成骨细胞规则地围绕,提示有活跃的成骨。纤维结构区可见纤维组织排列与牵张方向一致,其间可见大量的毛细血管,新生血管的方向与牵张方向一致(图3A)。在整个牵张区未发现软骨成骨区,说明牙槽骨牵张成骨术的骨愈合是以膜内成骨的方式进行的,与骨折愈合的方式明显不同。固定期2个月时,大部分的牵张区由网状的骨小梁组成。骨小梁的结构较1个月时变粗,变密和规则。在骨小梁的周围可见成骨细胞围绕。舌侧骨板由完整的骨小梁连接;在颊侧,有软组织向内生长,使颊侧牵张区形成凹陷,这与放射学检查的结果一致(图3B)。固定期3个月时,牵张区主要由板状骨和编织骨组成,有规则的哈弗管。骨组织间的血管密度较1个月、2个月有降低。可观察到骨组织的血管方向与牵张方向一致。板状骨中可以观察到破骨细胞,提示存在骨的形成与改建(图3C)。 2.4 生物力学检测 比较1个月组、2个月组、3个月组与对照组的剪切力发现:牵张区的剪切力值随着固定期的延长而上升,1个月组、2个月组与3个月组间比较差异有显著性意义(P < 0.05),3个月组与对照组比较差异无显著性意义(P > 0.05),见图4。"
| [1] Langenbeck BV. About the pathologic length growth of long bones and its employment in surgical praxis. Berl Klin Wochenschr. 1869;26:265. [2] Ilizarov GA.The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation.Clin Orthop Relat Res. 1989; (238):249-281. [3] Ilizarov GA.The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction.Clin Orthop Relat Res. 1989;(239): 263-285. [4] Block MS, Daire J, Stover J,et al.Changes in the inferior alveolar nerve following mandibular lengthening in the dog using distraction osteogenesis.J Oral Maxillofac Surg. 1993; 51(6):652-660. [5] Block MS, Chang A, Crawford C.Mandibular alveolar ridge augmentation in the dog using distraction osteogenesis.J Oral Maxillofac Surg. 1996;54(3):309-314. [6] Block MS, Almerico B, Crawford C,et al.Bone response to functioning implants in dog mandibular alveolar ridges augmented with distraction osteogenesis.Int J Oral Maxillofac Implants. 1998;13(3):342-351. [7] Makarov MR, Harper RP, Cope JB,et al.Evaluation of inferior alveolar nerve function during distraction osteogenesis in the dog.J Oral Maxillofac Surg. 1998;56(12):1417-1423. [8] Engel PS, Rauch DM, Ladov MJ,et al.Alveolar distraction osteogenesis: a new alternative to bone grafts. Report of three cases.J N J Dent Assoc. 1999;70(1):15, 20-21, 56-57. [9] Mitsukawa N, Saiga A, Morishita T,et al.Special distraction osteogenesis before bone grafting for alveolar cleft defects to correct maxillary deformities in patients with bilateral cleft lips and palates: Distraction osteogenesis performed separately for each bone segment.J Craniomaxillofac Surg. 2013. [Epub ahead of print] [10] Kumar N, Prashantha G, Raikar S, et al.Dento-Alveolar Distraction Osteogenesis for rapid Orthodontic Canine Retraction.J Int Oral Health. 2013;5(6):31-41. [11] Block MS, Gardiner D, Almerico B,et al.Loaded hydroxylapatite-coated implants and uncoated titanium-threaded implants in distracted dog alveolar ridges. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 89(6): 676-685. [12] Yamauchi K, Takahashi T, Nogami S,et al.Horizontal alveolar distraction osteogenesis for dental implant: long-term results.Clin Oral Implants Res. 2013;24(5):563-568. [13] Ugurlu F, Sener BC, Dergin G,et al.Potential complications and precautions in vertical alveolar distraction osteogenesis: a retrospective study of 40 patients.J Craniomaxillofac Surg. 2013;41(7):569-573. [14] Rachmiel A, Emodi O, Gutmacher Z,et al.Oral and dental restoration of wide alveolar cleft using distraction osteogenesis and temporary anchorage devices.J Craniomaxillofac Surg. 2013;41(8):728-734. [15] Ohba S, Tobita T, Tajima N,et al.Correction of an asymmetric maxillary dental arch by alveolar bone distraction osteogenesis.Am J Orthod Dentofacial Orthop. 2013;143(2): 266-273. [16] Kim JW, Cho MH, Kim SJ,et al.Alveolar distraction osteogenesis versus autogenous onlay bone graft for vertical augmentation of severely atrophied alveolar ridges after 12 years of long-term follow-up.Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116(5):540-549. [17] Kawashima W, Takayama K, Fujii R,et al.Vector-controlled alveolar distraction osteogenesis using an implant-fixed provisional prosthesis: a case report.Implant Dent. 2013; 22(1):26-30. [18] Joss CU, Triaca A, Antonini M, et al.Neurosensory and functional evaluation in distraction osteogenesis of the anterior mandibular alveolar process.Int J Oral Maxillofac Surg. 2013;42(1):55-61. [19] Isomura ET, Shogen Y, Hamaguchi M,et al.Electrophysiologic evaluation of inferior alveolar nerve regenerated by bifocal distraction osteogenesis in dogs.Plast Reconstr Surg. 2013; 132(4):877-882. . [20] Isomura ET, Shogen Y, Hamaguchi M, et al.Inferior alveolar nerve regeneration after bifocal distraction osteogenesis in dogs.J Oral Maxillofac Surg. 2013;71(10):1810.e1-11. [21] Felice P, Lizio G, Checchi L.Alveolar distraction osteogenesis in posterior atrophic mandible: a case report on a new technical approach.Implant Dent. 2013;22(4):332-338. [22] Faysal U, Cem SB, Atilla S.Effects of different consolidation periods on bone formation and implant success in alveolar distraction osteogenesis: a clinical study.J Craniomaxillofac Surg. 2013;41(3):194-197. [23] Cheung LK, Chua HD, Hariri F,et al.Alveolar distraction osteogenesis for dental implant rehabilitation following fibular reconstruction: a case series.J Oral Maxillofac Surg. 2013; 71(2):255-271. [24] Chiapasco M, Casentini P, Zaniboni M.Bone augmentation procedures in implant dentistry.Int J Oral Maxillofac Implants. 2009;24 Suppl:237-259. [25] McAllister BS, Haghighat K.Bone augmentation techniques.J Periodontol. 2007;78(3):377-396. [26] Uckan S, Veziroglu F, Dayangac E.Alveolar distraction osteogenesis versus autogenous onlay bone grafting for alveolar ridge augmentation: Technique, complications, and implant survival rates.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(4):511-515. [27] Vega LG, Bilbao A.Alveolar distraction osteogenesis for dental implant preparation: an update.Oral Maxillofac Surg Clin North Am. 2010;22(3):369-385. [28] Cheung LK, Hariri F, Chua HD.Alveolar distraction osteogenesis for oral rehabilitation in reconstructed jaws.Curr Opin Otolaryngol Head Neck Surg. 2011;19(4):312-316. [29] Saulacic N, Gándara-Vila P, Somoza-Martín M,et al. Distraction osteogenesis of the alveolar ridge: a review of the literature.Med Oral. 2004;9(4):321-327. [30] Emtiaz S, Noroozi S, Caramês J,et al.Alveolar vertical distraction osteogenesis: historical and biologic review and case presentation.Int J Periodontics Restorative Dent. 2006; 26(6):529-541. [31] Boyne PJ, Herford AS.Distraction osteogenesis of the nasal and antral osseous floor to enhance alveolar height.J Oral Maxillofac Surg. 2004;62(9 Suppl 2):123-130. [32] Whitesides LM, Meyer RA.Effect of distraction osteogenesis on the severely hypoplastic mandible and inferior alveolar nerve function.J Oral Maxillofac Surg. 2004;62(3):292-297. [33] Oda T, Sawaki Y, Ueda M.Alveolar ridge augmentation by distraction osteogenesis using titanium implants: an experimental study.Int J Oral Maxillofac Surg. 1999;28(2): 151-156. [34] Chiapasco M, Zaniboni M, Rimondini L.Autogenous onlay bone grafts vs. alveolar distraction osteogenesis for the correction of vertically deficient edentulous ridges: a 2-4-year prospective study on humans.Clin Oral Implants Res. 2007; 18(4):432-440. [35] Zhao Y, Liu Y, Liu B,et al.Bone healing process around distraction implants following alveolar distraction osteogenesis: a preliminary experimental study in dogs.Int J Periodontics Restorative Dent. 2009;29(5):523-533. [36] Chiapasco M, Consolo U, Bianchi A,et al.Alveolar distraction osteogenesis for the correction of vertically deficient edentulous ridges: a multicenter prospective study on humans.Int J Oral Maxillofac Implants. 2004;19(3):399-407. [37] Sezer B, Koyuncu BÖ, Günbay T, et al.Alveolar distraction osteogenesis in the human mandible: a clinical and histomorphometric study.Implant Dent. 2012;21(4):317-322. [38] Alkan A, Ba? B, Inal S.Alveolar distraction osteogenesis of bone graft reconstructed mandible.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(3):e39-42. [39] Braidy H, Appelbaum M.Alveolar distraction osteogenesis of the severely atrophic anterior maxilla: surgical and prosthetic challenges.J Prosthodont. 2011;20(2):139-143. [40] Mazzonetto R, Serra E Silva FM, Ribeiro Torezan JF.Clinical assessment of 40 patients subjected to alveolar distraction osteogenesis.Implant Dent. 2005;14(2):149-153. [41] Henkel KO, Ma L, Lenz JH,et al.Closure of vertical alveolar bone defects with guided horizontal distraction osteogenesis: an experimental study in pigs and first clinical results.J Craniomaxillofac Surg. 2001;29(5):249-253. [42] Saulacic N, Zix J, Iizuka T.Complication rates and associated factors in alveolar distraction osteogenesis: a comprehensive review.Int J Oral Maxillofac Surg. 2009;38(3):210-217. [43] Perdijk FB, Meijer GJ, Strijen PJ,et al.Complications in alveolar distraction osteogenesis of the atrophic mandible.Int J Oral Maxillofac Surg. 2007;36(10):916-921. [44] Garcia Garcia A, Somoza Martin M, Gandara Vila P,et al.Alveolar ridge osteogenesis using 2 intraosseous distractors: uniform and nonuniform distraction.J Oral Maxillofac Surg. 2002;60(12):1510-1512. [45] Veziroglu F, Yilmaz D.Biomechanical evaluation of the consolidation period of alveolar distraction osteogenesis with three-dimensional finite element analysis.Int J Oral Maxillofac Surg. 2008;37(5):448-452. [46] Enislidis G, Fock N, Millesi-Schobel G,et al.Analysis of complications following alveolar distraction osteogenesis and implant placement in the partially edentulous mandible.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(1): 25-30. [47] Wolf JH.Julis Wolff and his "law of bone remodeling". Orthopade. 1995;24(5):378-386. [48] Costantino PD, Friedman CD.Distraction osteogenesis. Applications for mandibular regrowth.Otolaryngol Clin North Am. 1991;24(6):1433-1443. [49] Costantino PD, Shybut G, Friedman CD,et al.Segmental mandibular regeneration by distraction osteogenesis. An experimental study.Arch Otolaryngol Head Neck Surg. 1990; 116(5):535-545. |
| [1] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [2] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [3] | Zhou Jihui, Li Xinzhi, Zhou You, Huang Wei, Chen Wenyao. Multiple problems in the selection of implants for patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1440-1445. |
| [4] | Wang Debin, Bi Zhenggang. Related problems in anatomy mechanics, injury characteristics, fixed repair and three-dimensional technology application for olecranon fracture-dislocations [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1446-1451. |
| [5] | Xu Yulin, Shen Shi, Zhuo Naiqiang, Yang Huilin, Yang Chao, Li Yang, Zhao Heng, Zhao Lu. Biomechanical comparison of three different plate fixation methods for acetabular posterior column fractures in standing and sitting positions [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 826-830. |
| [6] | Cai Qunbin, Zou Xia, Hu Jiantao, Chen Xinmin, Zheng Liqin, Huang Peizhen, Lin Ziling, Jiang Ziwei. Relationship between tip-apex distance and stability of intertrochanteric femoral fractures with proximal femoral anti-rotation nail: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 831-836. |
| [7] | Wang Jiangna, Zheng Huifen, Sun Wei. Changes in dynamic stability, motor coordination and joint mechanics of the lower extremity during stair descent and performing phone task [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 837-843. |
| [8] | Song Chengjie, Chang Hengrui, Shi Mingxin, Meng Xianzhong. Research progress in biomechanical stability of lateral lumbar interbody fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 923-928. |
| [9] | Xie Chongxin, Zhang Lei. Comparison of knee degeneration after anterior cruciate ligament reconstruction with or without remnant preservation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 735-740. |
| [10] | Nie Shaobo, Li Jiantao, Sun Jien, Zhao Zhe, Zhao Yanpeng, Zhang Licheng, Tang Peifu. Mechanical stability of medial support nail in treatment of severe osteoporotic intertrochanteric fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 329-333. |
| [11] | Tan Jiachang, Yuan Zhenchao, Wu Zhenjie, Liu Bin, Zhao Jinmin. Biomechanical analysis of elastic nail combined with end caps and wire fixation for long oblique femoral shaft fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 334-338. |
| [12] | Chen Lu, Zhang Jianguang, Deng Changgong, Yan Caiping, Zhang Wei, Zhang Yuan. Finite element analysis of locking screw assisted acetabular cup fixation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 356-361. |
| [13] | Zhou Jihui, Li Xinzhi, Zhou You, Huang Wei, Chen Wenyao. Comparison of the advantages and disadvantages of multiple implants in treatment of traumatic dislocation of sternoclavicular joint [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 443-448. |
| [14] | Li Kun, Li Zhijun, Zhang Shaojie, Gao Shang, Sun Hao, Yang Xi, Wang Xing, Dai Lina . A 4-year-old child model of occipito-atlanto-axial joints established by finite element dynamic simulation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3773-3778. |
| [15] | Sun Maji, Wang Qiuan, Zhang Xingchen, Guo Chong, Yuan Feng, Guo Kaijin. Development and biomechanical analysis of a new anterior cervical pedicle screw fixation system [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3821-3825. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||