Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (5): 1282-1293.doi: 10.12307/2026.032
Previous Articles Next Articles
Effects of different neuromodulatory stimulation modalities on non-motor symptoms in Parkinson’s patients: a network meta-analysis
Leng Xiaoxuan1, Zhao Yuxin1, Liu Xihua2
- 1College of Rehabilitation Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China; 2Department of Rehabilitation, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250012, Shandong Province, China
-
Received:2024-12-04Accepted:2025-02-06Online:2026-02-18Published:2025-06-27 -
Contact:Liu Xihua, MD, Chief physician, Master’s supervisor, Department of Rehabilitation, Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250012, Shandong Province, China -
About author:Leng Xiaoxuan, Master candidate, College of Rehabilitation Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China -
Supported by:Shandong Province Traditional Chinese Medicine Science and Technology Project, No. M-2023142 (to LXH); Shandong Province Medical Staff Science and Technology Innovation Program Project, No. SDYWZGKCJH2022024 (to LXH)
CLC Number:
Cite this article
Leng Xiaoxuan, Zhao Yuxin, Liu Xihua. Effects of different neuromodulatory stimulation modalities on non-motor symptoms in Parkinson’s patients: a network meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1282-1293.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

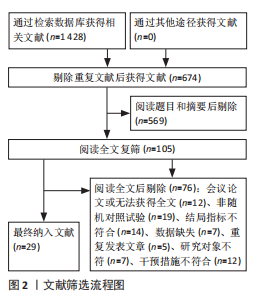
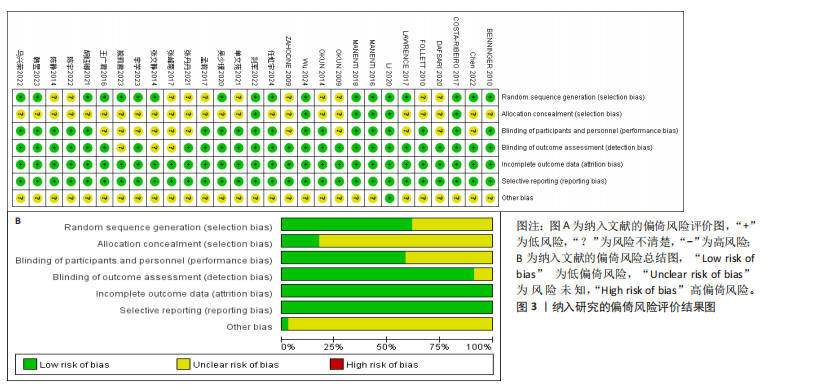
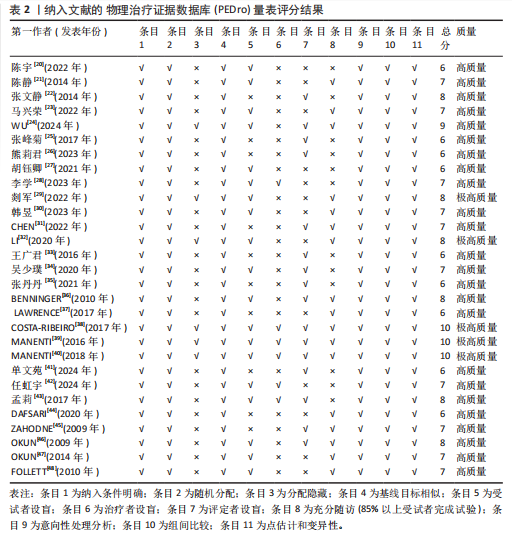
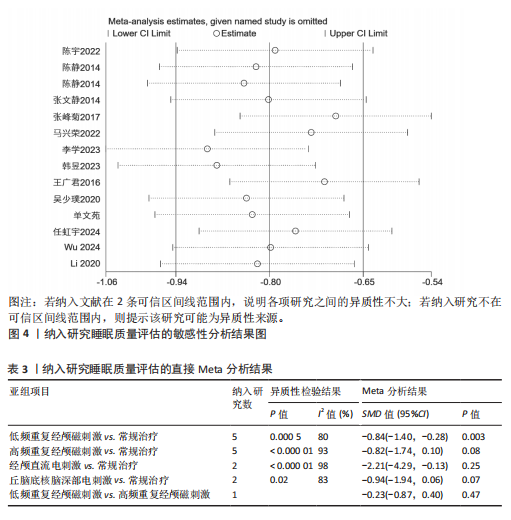
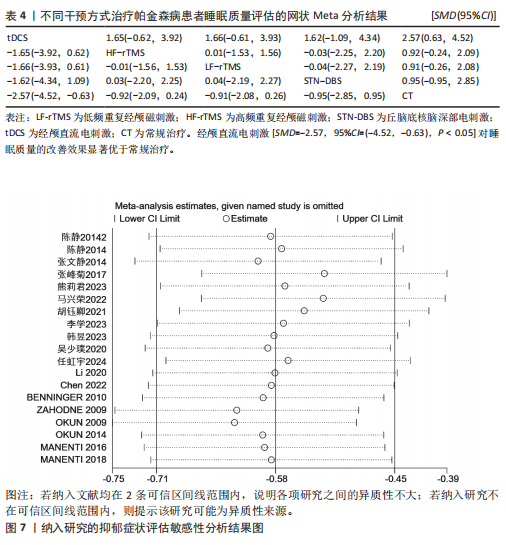
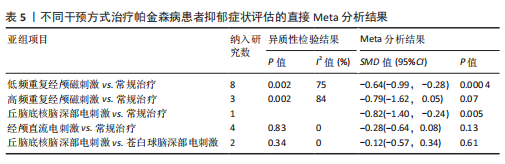
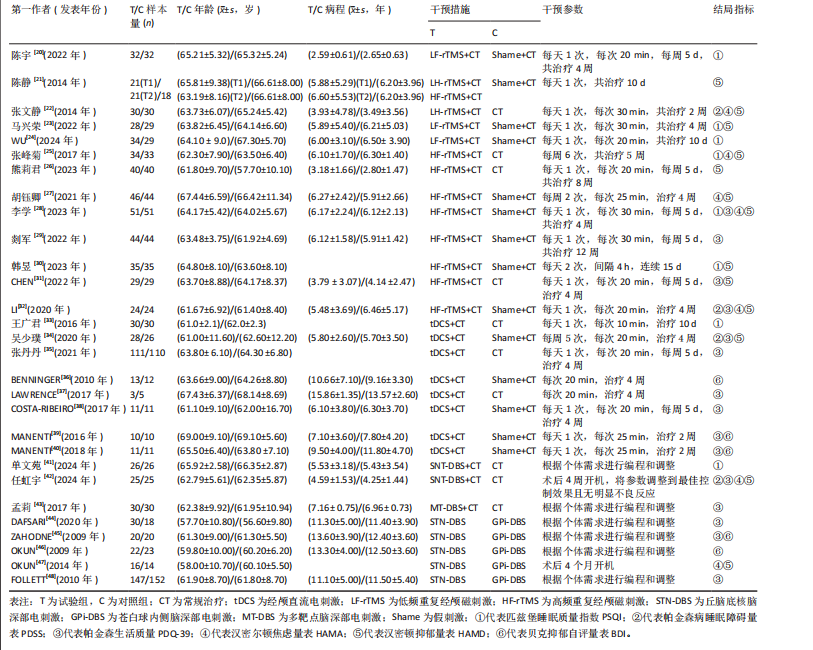
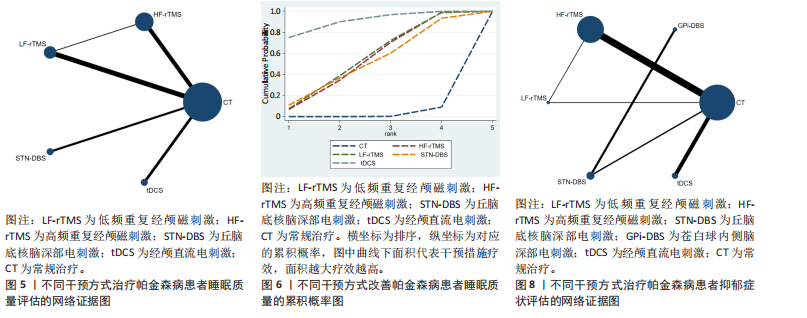
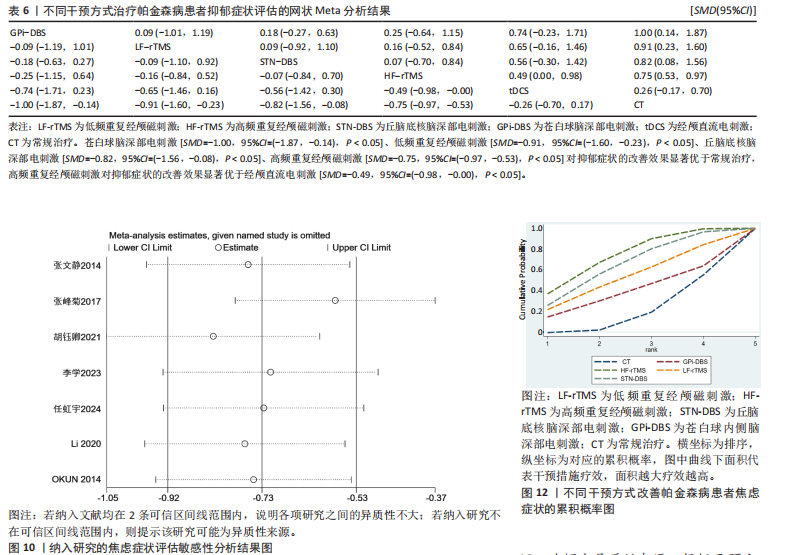
2.2 纳入文献的基本特征 纳入29篇文献的发表年份为2009-2024年,包含高频重复经颅磁刺激、低频重复经颅磁刺激、经颅直流电刺激、丘脑底核脑深部电刺激、苍白球内侧脑深部电刺激、多靶点脑深部电刺激6种神经调控技术刺激方式。纳入文献的基本特征表见表1。 2.3 纳入文献的质量评价结果 纳入的29项研究均为随机分组,均采用随机数字表法进行随机分组;6项研究采用不透明信封进行分配隐藏[24,29,32,38-40];19项研究对纳入对象或干预者施盲[20-21,23-24,27-30,32,34,36,38-40,42-43,46-48]; 16项研究对结局评估者施盲[22,24-26,31,33-36,38-41,43,45-46];29项研究结局数据均完整、均无选择性报告(低风险)、其他风险偏倚不清楚[20-48]。纳入文献的风险偏倚评价结果,见图3。采用 PEDro量表对纳入的文献进行质量评价,结果显示纳入的文献总体质量较高,平均分为7.28,24项研究为高质量[20-28,30-31,33-37,41-48],5项研究为极高质量[29,32,38-40],详情见表2。 2.4 Meta分析结果 2.4.1 睡眠质量评估结果 (1)传统Meta分析结果:13项研究的结局指标涉及睡眠质量评估[20-25,28,30,32-34,41-42],异质性检验结果显示I2=91%、P < 0.001,表明研究间存在较高的异质性,采用随机效应模型,并对纳入文献进行敏感性分析,提示结果比较稳健,见图4。为探究异质性来源,根据干预方式进行亚组分析,结果显示异质性仍较高,因此,仅对结果进行描述性分析。传统Meta分析结果显示,低频重复经颅磁刺激对睡眠质量评分的改善情况显著优于常规治疗(P < 0.05),见表3。 (2)网状Meta分析结果:13项研究的结局指标涉及睡眠质量评估[20-25,28,30,32-34,41-42],包括经颅直流电刺激、高频重复经颅磁刺激、低频重复经颅磁刺激、丘脑底核脑深部电刺激及常规治疗在内的5种治疗方式,睡眠质量评估的证据网络,见图5。节点分析模型显示睡眠质量评估指标P=0.688 2,提示整体一致性良好。使用节点劈裂法进行局部不一致性检验,发现P均> 0.05,说明局部不一致性不显著,直接比较与间接比较具有较强的一致性,采用一致性模型进行分析。 网状Meta分析结果显示,经颅直流电刺激[SMD=-2.57,95%CI=(-4.52,-0.63),P < 0.05]对睡眠质量的改善效果显著优于常规治疗,但尚无证据表明其他脑刺激方式对睡眠质量的改善效果显著优于常规治疗,并且4种脑刺激方式两两比较差异无显著性意义(P > 0.05),见表4。 对5种干预方式改善睡眠质量的优劣进行排序,最佳概率排序由高到低为:经颅直流电刺激(92.9%)>高频重复经颅磁刺激(50.4%)>丘脑底核脑深部电刺激(49.9%)>低频重复经颅磁刺激(49.7%)>常规治疗(7.1 %),见图6。 2.4.2 抑郁症状评估结果(1)传统Meta分析结果:18项研究的结局指标涉及抑郁症状评估[21-23,25-28,30-32,34,36,39-40,42,45-47],异质性检验结果显示I2=83%、P < 0.05,表明研究间存在较高的异质性,采用随机效应模型,对纳入文献进行敏感性分析,提示结果比较稳健,见图7。为探究异质性来源,根据干预方式进行亚组分析,结果显示部分亚组异质性显著降低,提示不同干预方式可能是异质性的来源。传统Meta分析结果显示,低频重复经颅磁刺激、丘脑底核脑深部电刺激对抑郁症状的改善情况显著优于常规治疗(P < 0.05),见表5。 (2)网状Meta分析结果:18项研究的结局指标涉及抑郁症状评估[21-23,25-28,30-32,34,36,39-40,42,45-47],包括低频重复经颅磁刺激、高频重复经颅磁刺激、丘脑底核脑深部电刺激、苍白球内侧脑深部电刺激、经颅直流电刺激及常规治疗在内的6种治疗方式,抑郁症状评估的证据网络,见图8。节点分析模型显示抑郁症状评估指标P=0.428 9,提示该结局指标整体上直"

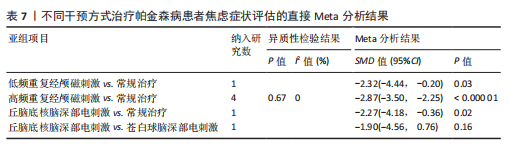
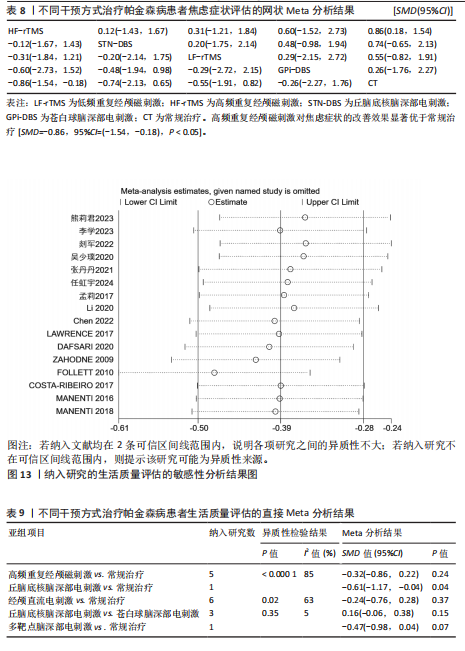
接比较与间接比较之间不存在不一致性,采用一致性模型进行分析。采用节点劈裂法进行局部不一致性检验,发现P均> 0.05,说明局部一致性良好。 网状Meta分析结果显示,苍白球脑深部电刺激[SMD=-1.00,95%CI=(-1.87,-0.14),P < 0.05]、低频重复经颅磁刺激[SMD=-0.91,95%CI=(-1.60,-0.23),P < 0.05]、丘脑底核脑深部电刺激[SMD=-0.82,95%CI=(-1.56,-0.08),P < 0.05]、高频重复经颅磁刺激[SMD=-0.75,95%CI=(-0.97,-0.53),P < 0.05]对抑郁症状的改善效果显著优于常规治疗,而尚无证据表明其他脑刺激方式对抑郁症状的改善效果显著优于常规治疗;5种脑刺激方式之间,高频重复经颅磁刺激对抑郁症状的改善效果显著优于经颅直流电刺激[SMD=-0.49,95%CI=(-0.98,-0.00),P < 0.05],而其他脑刺激之间对抑郁症状的改善效果两两比较差异均无显著性意义(P > 0.05),见表6。 对6种干预方式改善抑郁症状的优劣进行排序,最佳概率排序由高到低为:苍白球内侧脑深部电刺激(80.6%)>低频重复经颅磁刺激(71.9%)>丘脑底核脑深部电刺激(62.7%)>高频重复经颅磁刺激(59.6%)>经颅直流电刺激(22.2%)>常规治疗(2.9%),见图9。 2.4.3 焦虑症状评估结果 (1)传统Meta分析结果:7项研究的结局指标涉及焦虑症状评估[22,25,27-28,32,42,47],异质性校验显示I2=83%、P < 0.05,表明研究间存在较高的异质性,采用随机效应模型,对纳入文献进行敏感性分析,提示结果比较稳健,见图10。为探究异质性来源,根据干预方式进行亚组分析后异质性显著降低,提示不同干预方式为异质性的主要来源。传统Meta分析结果显示,低频重复经颅磁刺激、高频重复经颅磁刺激、丘脑底核脑深部电刺激对焦虑症状的改善情况显著优于常规治疗(P < 0.05),见表7。 (2)网状Meta分析结果:7项研究的结局指标涉及焦虑症状评"

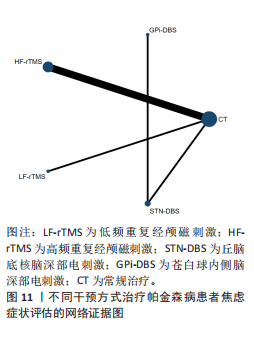
估[22,25,27-28,32,42,47],包括高频重复经颅磁刺激、低频重复经颅磁刺激、丘脑底核脑深部电刺激、苍白球脑深部电刺激及常规治疗在内的5种治疗方式,抑郁症状评估的网络证据图,见图11。未形成闭合环,因此未对该结果进行不一致性检验,直接采用一致性模型进行分析。 网状Meta分析结果显示,高频重复经颅磁刺激对焦虑症状的改善效果显著优于常规治疗[SMD=-0.86,95%CI=(-1.54,-0.18),P < 0.05],而尚无证据表明其他脑刺激方式焦虑症状的改善效果显著优于常规治疗,并且4种脑刺激方式对焦虑症状的改善两两比较差异无显著性意义(P > 0.05),见表8。 对5种干预方式改善焦虑症状的"

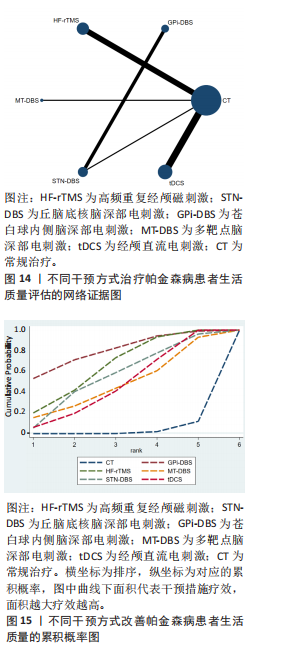
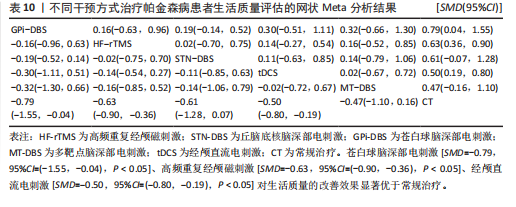
优劣进行排序,最佳概率排序由高到低为:高频重复经颅磁刺激(72.5%)>丘脑底核脑深部电刺激(65.4%)>低频重复经颅磁刺激(53.7%)>苍白球内侧脑深部电刺激(39.4%)>常规治疗(19.1%),见图12。 2.4.4 生活质量评估 (1)传统Meta分析:16项研究的结局指标涉及生活质量评估[26,28-29,31-32,34-35,37-40,42-45,48],传统Meta分析结果显示I2=70%、P < 0.05,表明研究间存在较高的异质性,采用随机效应模型,对纳入文献进行敏感性分析,提示结果比较稳健,见图13。为探究异质性来源,根据干预方式对其进行亚组分析发现异质性仍较高,因此,仅对结果进行描述性分析。传统Meta分析结果显示,丘脑底核脑深部电刺激对生活质量评分的改善情况显著优于常规治疗(P < 0.05),见表9。 (2)网状Meta分析结果:16项研究的结局指标涉及生活质量评估[26,28-29,31-32,34-35,37-40,42-45,48],包括高频重复经颅磁刺激、丘脑底核脑深部电刺激、苍白球内侧脑深部电刺激、多靶点脑深部电刺激、经颅直流电刺激及常规治疗在内的6种治疗方式,生活质量评分的网络证据图,见图14。图中未形成闭合环,因此未对该结果进行不一致性检验,直接采用一致性模型进行分析。 网状Meta分析结果显示,苍白球脑深部电刺激[SMD=-0.79,95%CI=(-1.55,-0.04),P < 0.05]、高频重复经颅磁刺激[SMD=-0.63,95%CI=(-0.90,-0.36),P < 0.05]、经"

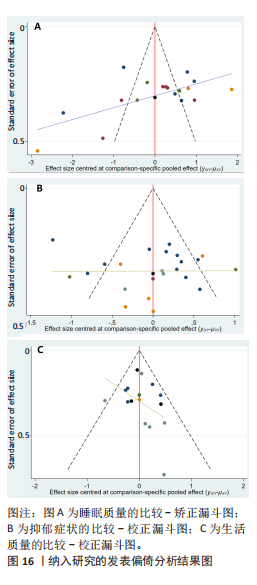
颅直流电刺激[SMD=-0.50,95%CI=(-0.80,-0.19),P < 0.05]对生活质量的改善效果显著优于常规治疗,而尚无证据表明其他脑刺激方式对生活质量的改善效果显著优于常规治疗,5种脑刺激方式之间对生活质量的改善两两比较差异均无显著性意义(P > 0.05),见表10。 对6种干预方式改善生活质量的优劣进行排序,最佳概率排序由高到低为:苍白球内侧脑深部电刺激(80.2%)>高频重复经颅磁刺激(66.0%)>丘脑底核脑深部电刺激(55.4%)>经颅直流电刺激(47.9%)>多靶点脑深部电刺激(47.7%)>常规治疗(2.7%),见图15。 2.5 不良反应分析 纳入文献中,有1篇文献报道,在接受rTMS后患者出现短暂轻微的头晕、头痛,治疗结束后随即消失[30];1篇文献报道,在接受rTMS治疗后患者出现轻微肩痛[20];1篇文献报道,在接受tDCS时电极贴片处有轻微刺痛,但能耐受[34];1篇文献报道,rTMS组患者因腿部疼痛无法静坐而退出试验[42]。总体来说,上述神经调控技术的安全性较高。 2.6 发表偏倚检验结果 研究对睡眠质量、抑郁症状及生活质量3个结局指标进行发表偏倚检验,结果显示,针对睡眠质量及抑郁症状的漏斗图内散点分布不均匀,并且部分散点落于漏斗图外,见图16A,B,提示可能存在一定的小样本效应及发表偏倚;针对生活质量的漏斗图内散点基本落于图的上部,并且左右对称良好,见图16C,提示文章存在发表偏倚的可能性较小。进一步进行Egger检验,结果显示睡眠质量P=0.433、生活质量P=0.573、抑郁症状P=0.188,提示所纳入的研究不存在小样本研究效应。"
| [1] MORRIS HR, SPILLANTINI MG, SUE CM, et al. The pathogenesis of Parkinson’s disease. Lancet. 2024;403(10423):293-304. [2] 王坚,邬剑军,常颖,等.中国帕金森疾病蓝皮书[J].中国临床神经科学,2024,32(S1):1-41. [3] HAYES MT. Parkinson’s Disease and Parkinsonism. Am J Med. 2019;132(7):802-807. [4] STEFANI A, HÖGL B. Sleep in Parkinson’s disease. Neuropsychopharmacology. 2020; 45(1):121-128. [5] AHMAD MH, RIZVI MA, ALI M, et al. Neurobiology of depression in Parkinson’s disease: Insights into epidemiology, molecular mechanisms and treatment strategies. Ageing Res Rev. 2023;85: 101840. [6] PONTONE GM, MILLS KA. Optimal Treatment of Depression and Anxiety in Parkinson’s Disease. Am J Geriatr Psychiatry. 2021;29(6):530-540. [7] MÜLLER B, ASSMUS J, HERLOFSON K, et al. Importance of motor vs. non-motor symptoms for health-related quality of life in early Parkinson’s disease. Parkinsonism Relat Disord. 2013;19(11):1027-1032. [8] 司慧丽,纪别克,赵鸿雁,等.帕金森病患者睡眠障碍特点及其影响因素分析[J].广东医学, 2020,41(1):61-65. [9] PARPURA V, SILVA GA, TASS PA, et al. Neuromodulation: selected approaches and challenges. J Neurochem. 2013;124(4):436-453. [10] 解虎涛,张建国.神经调控技术的过去、现在和未来[J].四川大学学报(医学版),2022, 53(4):559-563. [11] FOLTYNIE T, BRUNO V, FOX S, et al. Medical, surgical, and physical treatments for Parkinson’s disease. Lancet. 2024;403(10423):305-324. [12] LEE JY, KIM SH, KO AR, et al. Therapeutic effects of repetitive transcranial magnetic stimulation in an animal model of Parkinson’s disease. Brain Res. 2013;1537:290-302. [13] DAGAN M, HERMAN T, HARRISON R, et al. Multitarget transcranial direct current stimulation for freezing of gait in Parkinson’s disease. Mov Disord. 2018;33(4):642-646. [14] FAN SY, WANG KL, HU W, et al. Pallidal versus subthalamic nucleus deep brain stimulation for levodopa-induced dyskinesia. Ann Clin Transl Neurol. 2020;7(1):59-68. [15] CHEN T, LIN F, CAI G. Comparison of the Efficacy of Deep Brain Stimulation in Different Targets in Improving Gait in Parkinson’s Disease: A Systematic Review and Bayesian Network Meta-Analysis. Front Hum Neurosci. 2021;15:749722. [16] POL F, SALEHINEJAD MA, BAHARLOUEI H, et al. The effects of transcranial direct current stimulation on gait in patients with Parkinson’s disease: a systematic review. Transl Neurodegener. 2021;10(1):22. [17] 黄木兰,王丽萍,胡柯嘉,等.非侵入式脑刺激对帕金森病患者执行功能的影响:网状meta分析[J].海军军医大学学报,2024,45(5):584-591. [18] 张振馨.帕金森病的诊断[J].中华神经科杂志, 2006,39(6):408-409. [19] 曹武婷,朱毅.循证物理治疗的推动者:物理治疗证据数据库PEDro[J].中国康复理论与实践, 2021,27(3):368-372. [20] 陈宇,赵静,万志荣,等.低频重复经颅磁刺激治疗帕金森病焦虑失眠的疗效分析[J].神经损伤与功能重建,2022,17(8):449-451+475. [21] 陈静,张长国,张红波,等.高频与低频重复经颅磁刺激治疗帕金森病的临床观察[J].中国康复医学杂志,2014,29(5):464-467. [22] 张文静,聂坤,张玉虎,等.重复经颅磁刺激治疗帕金森病失眠患者的效果观察[J].护理学报, 2014,21(23):28-30. [23] 马兴荣,刘希,任幼红,等.右侧前额叶背外侧区低频重复经颅磁刺激对帕金森病非运动症状的疗效[J].中国实用神经疾病杂志,2022, 25(3):289-294. [24] WU J, ZHUANG S, ZHANG X, et al. Objective sleep enhancement in Parkinson’s disease: A sham-controlled trial of low-frequency repetitive transcranial magnetic stimulation over the right dorsolateral prefrontal cortex. Parkinsonism Relat Disord. 2024;126:107050. [25] 张峰菊,王晓雪,刘欣欣.重复经颅磁刺激联合认知行为疗法对帕金森病非运动症状的疗效[J].中国实用神经疾病杂志,2017,20(9):61-63. [26] 熊莉君,杨燕,王芳.重复经颅磁刺激联合心理干预治疗帕金森病抑郁患者的疗效观察[J]. 中华物理医学与康复杂志,2023,45(4):312-316. [27] 胡钰卿,刘振国,叶青,等.熟地平颤方联合重复经颅磁刺激治疗帕金森病合并睡眠障碍临床研究[J].中国中医药信息杂志,2021,28(5):88-93. [28] 李学,陈思远,吴少璞,等.重复经颅磁刺激对中晚期帕金森病患者睡眠及血浆食欲素-A含量的影响[J].中华物理医学与康复杂志,2023, 45(3):232-235. [29] 剡军,王永正,赖彩琼.高频rTMS治疗帕金森病伴白天过度嗜睡的临床疗效及与弥散张量成像的相关性研究[J].中国康复,2022,37(10):592-597. [30] 韩昱,白抚生,张顺,等.高频重复经颅磁刺激治疗帕金森病非运动症状的疗效观察[J].中国实用内科杂志,2023,43(4):318-321. [31] CHEN J, XU P, GUO X, et al. Comparative Analysis of the Effects of Escitalopram, Pramipexole, and Transcranial Magnetic Stimulation on Depression in Patients With Parkinson Disease: An Open-Label Randomized Controlled Trial. Clin Neuropharmacol. 2022; 45(4):84-88. [32] LI J, MI TM, ZHU BF, et al. High-frequency repetitive transcranial magnetic stimulation over the primary motor cortex relieves musculoskeletal pain in patients with Parkinson’s disease: A randomized controlled trial. Parkinsonism Relat Disord. 2020;80:113-119. [33] 王广君,赵振华,吴东川,等.经颅直流电刺激对帕金森病非运动症状的疗效[J].中国医药导报,2016,13(5):75-78. [34] 吴少璞,李学,祁亚伟,等.经颅直流电刺激对伴快速眼动睡眠行为障碍-帕金森病患者睡眠障碍的影响[J].中华物理医学与康复杂志, 2020,42(1):50-54. [35] 张丹丹,毛洁萍.重复经颅直流电刺激对于PD患者躯干肌电特征、步行功能及生存质量的影响[J].中华保健医学杂志,2021,23(5):465-468. [36] BENNINGER DH, LOMAREV M, LOPEZ G, et al. Transcranial direct current stimulation for the treatment of Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2010;81(10):1105-1111. [37] LAWRENCE BJ, GASSON N, BUCKS RS, et al. Cognitive Training and Noninvasive Brain Stimulation for Cognition in Parkinson’s Disease: A Meta-analysis. Neurorehabil Neural Repair. 2017;31(7):597-608. [38] COSTA-RIBEIRO A, MAUX A, BOSFORD T, et al. Transcranial direct current stimulation associated with gait training in Parkinson’s disease: A pilot randomized clinical trial. Dev Neurorehabil. 2017; 20(3):121-128. [39] MANENTI R, BRAMBILLA M, BENUSSI A, et al. Mild cognitive impairment in Parkinson’s disease is improved by transcranial direct current stimulation combined with physical therapy. Mov Disord. 2016;31(5):715-724. [40] MANENTI R, COTELLI MS, COBELLI C, et al. Transcranial direct current stimulation combined with cognitive training for the treatment of Parkinson Disease: A randomized, placebo-controlled study. Brain Stimul. 2018;11(6):1251-1262. [41] 单文苑.双侧丘脑底核脑深部电刺激术对帕金森病患者睡眠质量及非运动症状的影响[J].中文科技期刊数据库(全文版)医药卫生,2024, 11(4):118-121. [42] 任虹宇,马俊,何森,等.丘脑底核脑深部电刺激术治疗帕金森病患者的疗效及术后认知功能分析[J].中国实用神经疾病杂志,2024,27(4):448-452. [43] 孟莉,郑德利,刘娜,等.脑深部电刺激术联合药物治疗原发性帕金森病疗效观察[J].中国现代神经疾病杂志,2017,17(2):121-126. [44] DAFSARI HS, DOS SANTOS GHILARDI MG, VISSER-VANDEWALLE V, et al. Beneficial nonmotor effects of subthalamic and pallidal neurostimulation in Parkinson’s disease. Brain Stimul. 2020;13(6): 1697-1705. [45] ZAHODNE LB, OKUN MS, FOOTE KD, et al. Greater improvement in quality of life following unilateral deep brain stimulation surgery in the globus pallidus as compared to the subthalamic nucleus. J Neurol. 2009;256(8):1321-1329. [46] OKUN MS, FERNANDEZ HH, WU SS, et al. Cognition and mood in Parkinson’s disease in subthalamic nucleus versus globus pallidus interna deep brain stimulation: the COMPARE trial. Ann Neurol. 2009;65(5):586-595. [47] OKUN MS, WU SS, FAYAD S, et al. Acute and Chronic Mood and Apathy Outcomes from a randomized study of unilateral STN and GPi DBS. PLoS One. 2014;9(12):e114140. [48] FOLLETT KA, WEAVER FM, STERN M, et al. Pallidal versus subthalamic deep-brain stimulation for Parkinson’s disease. N Engl J Med. 2010;362(22):2077-2091. [49] 王辰,朱玉连,王卫宁.神经调控技术在帕金森病冻结步态中的应用现状及进展[J].中国康复医学杂志,2024,39(7):1068-1074. [50] LIONNET A, LECLAIR-VISONNEAU L, NEUNLIST M, et al. Does Parkinson’s disease start in the gut? Acta Neuropathol. 2018;135(1):1-12. [51] MONTI JM, MONTI D. The involvement of dopamine in the modulation of sleep and waking. Sleep Med Rev. 2007;11(2):113-133. [52] MIZRAHI-KLIGER AD, KAPLAN A, ISRAEL Z, et al. Basal ganglia beta oscillations during sleep underlie Parkinsonian insomnia. Proc Natl Acad Sci U S A. 2020;117(29):17359-17368. [53] FILMER HL, DUX PE, MATTINGLEY JB. Applications of transcranial direct current stimulation for understanding brain function. Trends Neurosci. 2014;37(12):742-753. [54] SABÉ M, HYDE J, CRAMER C, et al. Transcranial Magnetic Stimulation and Transcranial Direct Current Stimulation Across Mental Disorders: A Systematic Review and Dose-Response Meta-Analysis [published correction appears in JAMA Netw Open. 2024;7(7):e2424292. [55] BEGEMANN MJ, BRAND BA, ĆURČIĆ-BLAKE B, et al. Efficacy of non-invasive brain stimulation on cognitive functioning in brain disorders: a meta-analysis. Psychol Med. 2020;50(15):2465-2486. [56] MERZAGORA AC, FOFFANI G, PANYAVIN I, et al. Prefrontal hemodynamic changes produced by anodal direct current stimulation. Neuroimage. 2010;49(3):2304-2310. [57] 袁德智,胡洁,赵秋叶,等.帕金森病进展速度与抑郁、睡眠障碍的相关性分析[J].中国医科大学学报,2020,49(4):326-330. [58] LI J, ZHU BF, GU ZQ, et al. Musculoskeletal Pain in Parkinson’s Disease. Front Neurol. 2022;12: 756538. [59] GREENHOUSE I, GOULD S, HOUSER M, et al. Stimulation at dorsal and ventral electrode contacts targeted at the subthalamic nucleus has different effects on motor and emotion functions in Parkinson’s disease. Neuropsychologia. 2011; 49(3):528-534. [60] 梁秦川,高国栋,王学廉,等.丘脑底核脑深部电刺激治疗帕金森病合并抑郁障碍的长期疗效[J].中华神经医学杂志,2006,5(11):1129-1131. [61] STEFANI A, TRENDAFILOV V, LIGUORI C, et al. Subthalamic nucleus deep brain stimulation on motor-symptoms of Parkinson’s disease: Focus on neurochemistry. Prog Neurobiol. 2017;151:157-174. [62] FAGGIANI E, DELAVILLE C, BENAZZOUZ A. The combined depletion of monoamines alters the effectiveness of subthalamic deep brain stimulation. Neurobiol Dis. 2015;82:342-348. [63] 陈普建,韩睿,周春英,等.苍白球内侧部脑深部电刺激治疗对帕金森病患者运动功能和抑郁的疗效[J].解放军预防医学杂志,2019,37(3):136-137. [64] 孔祥薇,康思敏,商慧芳,等.脑深部电刺激对帕金森病抑郁影响的网状Meta分析[J].华西医学,2023,38(3):416-423. [65] BIRCHALL EL, WALKER HC, CUTTER G, et al. The effect of unilateral subthalamic nucleus deep brain stimulation on depression in Parkinson’s disease. Brain Stimul. 2017;10(3):651-656. [66] 董震,张云淑,吴涵,等.功能磁共振引导下的重复经颅磁刺激对抑郁症短期疗效和执行功能的影响[J].河北医药,2022,44(8):1156-1159. [67] 郑秀琴,于苏文,何益民,等.高频重复经颅磁刺激对帕金森病患者临床症状及其细胞衰老相关因子的影响[J].中华物理医学与康复杂志, 2022,44(5):427-432. |
| [1] | Haonan Yang, Zhengwei Yuan, Junpeng Xu, Zhiqi Mao, Jianning Zhang. Preliminary study on the mechanisms and efficacy of deep brain stimulation in treating depression [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(在线): 1-9. |
| [2] | Yang Zhijie, Zhao Rui, Yang Haolin, Li Xiaoyun, Li Yangbo, Huang Jiachun, Lin Yanping, Wan Lei, HuangHongxing. Postmenopausal osteoporosis: predictive values of muscle mass, grip strength, and appendicular skeletal muscle index [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1073-1080. |
| [3] | Yin Yongcheng, Zhao Xiangrui, Yang Zhijie, Li Zheng, Li Fang, Ning Bin. Effect and mechanism of peroxiredoxin 1 in microglial inflammation after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1106-1113. |
| [4] | Zhang Jiuxuan, Zhang Jinnan, Sui Xiaofan, Pei Xiaxia, Wei Jianhong, Su Qiang, Li Tian. Effects of ammonia poisoning on cognitive behavior and hippocampal synaptic damage in mice [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1122-1128. |
| [5] | Zhang Di, Zhao Jun, Ma Guangyue, Sun Hui, Jiang Rong. Mechanism of depression-like behavior in chronic social defeat stress mice based on high-throughput sequencing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1139-1146. |
| [6] | Sun Yajie, Zhao Xinchen, Bo Shuangling. Spatiotemporal expression of bone morphologic protein 7 in mouse kidney development [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1156-1161. |
| [7] | Li Haojing, Wang Xin, Song Chenglin, Zhang Shengnan, Chen Yunxin. Therapeutic efficacy of extracorporeal shock wave therapy in the upper trapezius muscle area combined with exercise control training in patients with chronic non-specific neck pain [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1162-1170. |
| [8] | Liu Yu, Lei Senlin, Zhou Jintao, Liu Hui, Li Xianhui. Mechanisms by which aerobic and resistance exercises improve obesity-related cognitive impairment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1171-1183. |
| [9] | Yu Huifen, Mo Licun, Cheng Leping. The position and role of 5-hydroxytryptamine in the repair of tissue injury [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1196-1206. |
| [10] | Wang Zhengye, Liu Wanlin, Zhao Zhenqun. Advance in the mechanisms underlying miRNAs in steroid-induced osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1207-1214. |
| [11] | Bu Yangyang, Ning Xinli, Zhao Chen. Intra-articular injections for the treatment of osteoarthritis of the temporomandibular joint: different drugs with multiple combined treatment options [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1215-1224. |
| [12] | Wen Fan, Xiang Yang, Zhu Huan, Tuo Yanfang, Li Feng. Exercise improves microvascular function in patients with type 2 diabetes [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1225-1235. |
| [13] | Liu Xinyue, Li Chunnian, Li Yizhuo, Xu Shifang. Regeneration and repair of oral alveolar bone defects [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1247-1259. |
| [14] | Zheng Yin, Wu Zhenhua, Zhang Cheng, Ruan Kexin, Gang Xiaolin, Ji Hong. Safety and efficacy of immunoadsorption therapy for rheumatoid arthritis: a network meta-analysis and systematic review [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1260-1268. |
| [15] | Wen Xiaolong, Weng Xiquan, Feng Yao, Cao Wenyan, Liu Yuqian, Wang Haitao. Effects of inflammation on serum hepcidin and iron metabolism related parameters in patients with type 2 diabetes mellitus: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1294-1301. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||