Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (8): 1727-1740.doi: 10.12307/2025.315
Previous Articles Next Articles
Effects of interval and continuous training on the quality of life in physically inactive adults: a meta-analysis
Zheng Huakun1, Yin Mingyue2, Liu Qian1
- 1School of Physical Education, Sichuan Agricultural University, Yaan 625014, Sichuan Province, China; 2School of Athletic Performance, Shanghai University of Sport, Shanghai 200438, China
-
Received:2024-02-27Accepted:2024-03-29Online:2025-03-18Published:2024-07-06 -
Contact:Liu Qian, Master, Professor, Master’s supervisor, School of Physical Education, Sichuan Agricultural University, Yaan 625014, Sichuan Province, China -
About author:Zheng Huakun, School of Physical Education, Sichuan Agricultural University, Yaan 625014, Sichuan Province, China Yin Mingyue, Master candidate, School of Athletic Performance, Shanghai University of Sport, Shanghai 200438, China Zheng Huakun and Yin Mingyue contributed equally to this work. -
Supported by:Sichuan Province Philosophy and Social Sciences Research “14th Five-Year Plan,” No. SC22B101 (to LQ); Sichuan Province College Student Innovation Training Program Project, No. S202310626033 (to ZHK)
CLC Number:
Cite this article
Zheng Huakun, Yin Mingyue, Liu Qian. Effects of interval and continuous training on the quality of life in physically inactive adults: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1727-1740.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
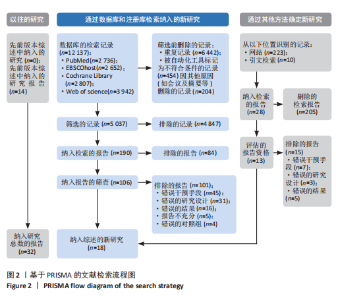
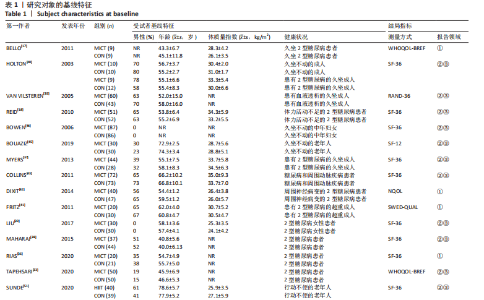
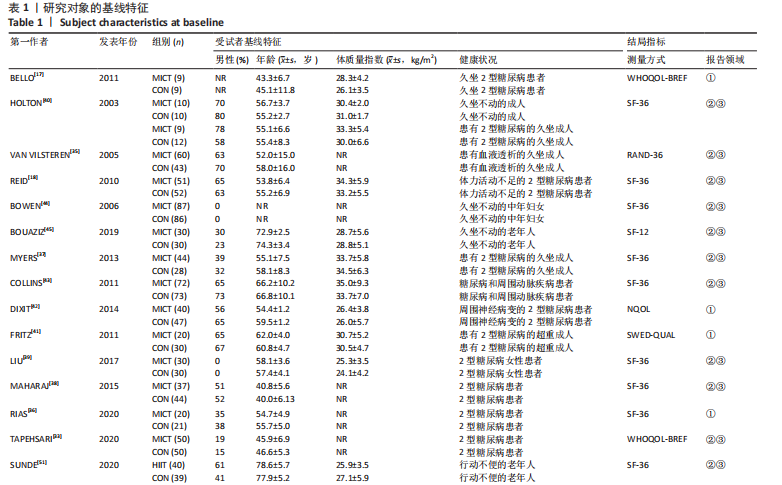
2.1 文献检索结果 文章共检索到12 137条记录,并在所引用研究的参考文献中补充了14项研究。此外,通过Google学术搜索额外发现了13项研究。在剔除重复项并按照纳入标准筛选后,共有32项随机对照试验符合纳入条件[17-18,33-62],见图2。 2.2 纳入研究临床特征 表1总结了参与者的基线特征。研究共纳入2 083名受试者,其中50.8%为男性,平均年龄(54.1±6.75)岁,体质量指数(31.0±4.84) kg/m2。有3项研究未报告性别[17,54-55],4项研究的研究对象为女性参与者[39,44,46,59]。在20项研究中,参与者大多为久坐不动且患有诸如糖尿病[17-18,33,36-43,49,61-62]、慢性心力衰竭[48,50]、行动不便[51]、外周动脉疾病[43]、血液透析患者[35],外周神经病变[42]、代谢综合征[54-55]、纤维肌痛和心肌梗死等并发症患者[46-47]。剩余参与者为久坐健康成人或体力活动不足的肥胖人群。在结局指标的报"
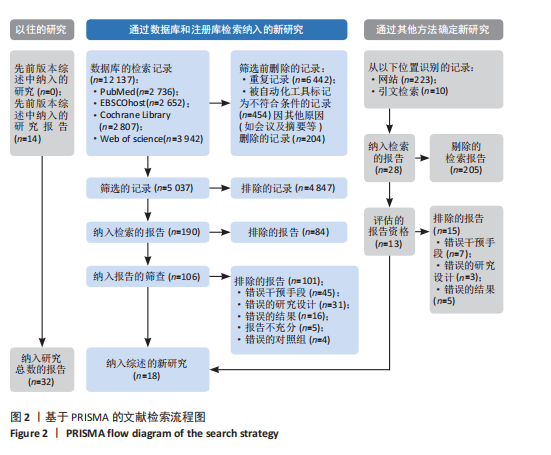

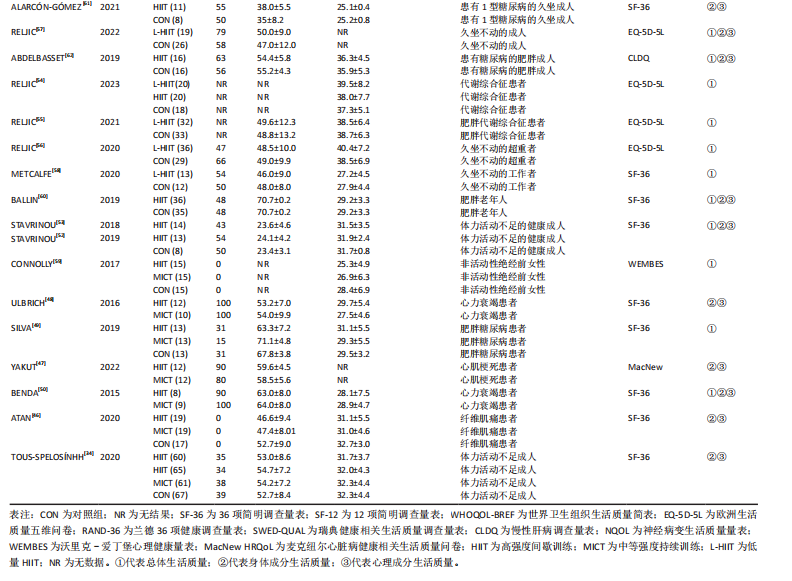
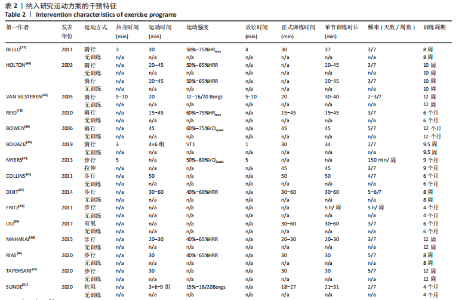
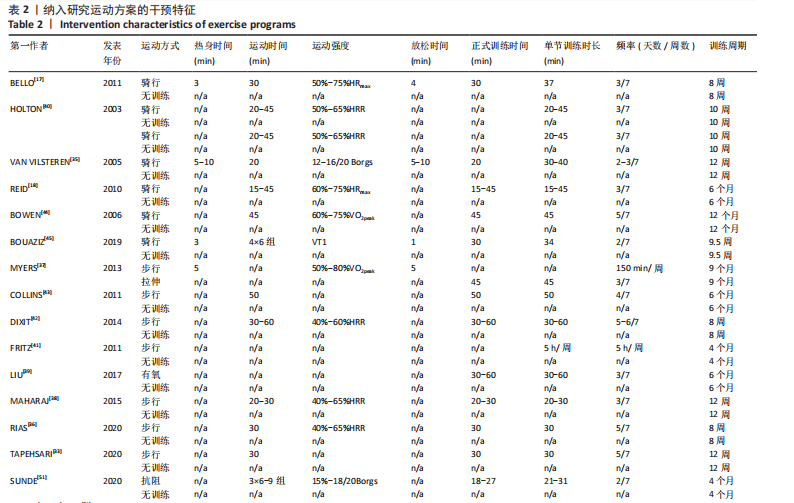
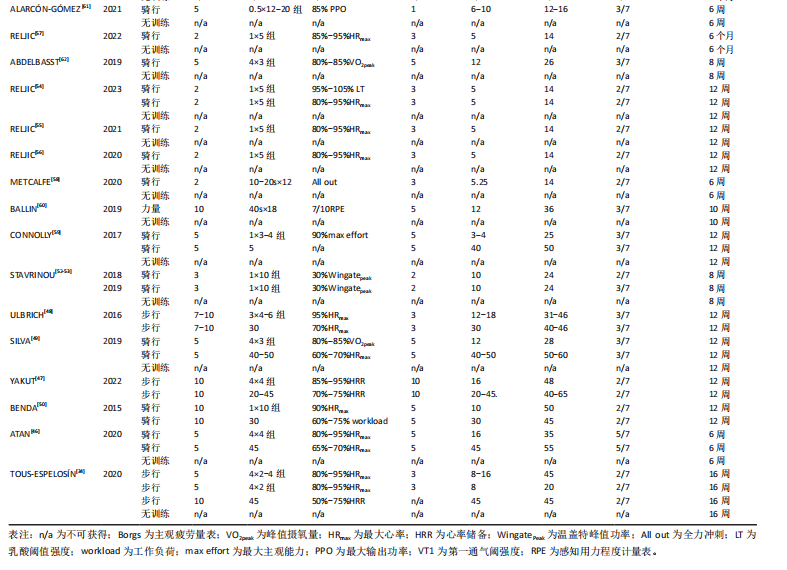
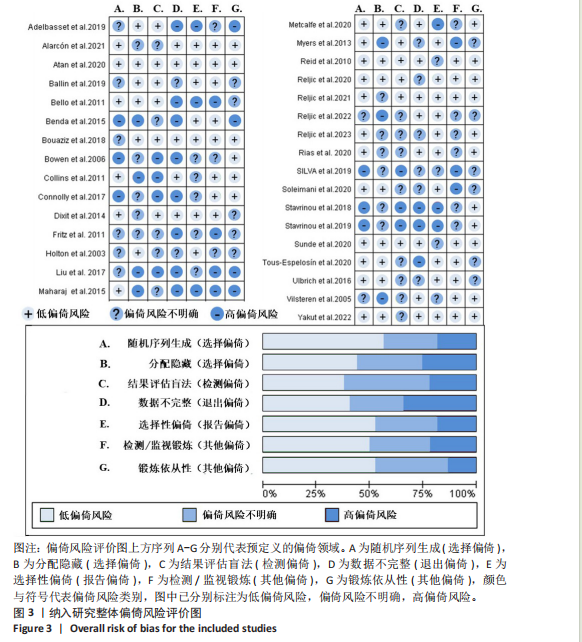
道中,最常用于测量生活质量的工具是SF-36,并在18项研究中得到使用[18,34,36-37,39-40,43-44,46,48-53,58,60-61]。共15项研究报告了整体生活质量[17,36,41-42,49-50,52-60],共17项研究使用特定领域的综合评分来评估身体与心理方面生活质量[18,33-35,37-40,43-48,51]。 2.3 运动方案的干预特征 表2总结了运动方案的干预特点。有18项研究比较了MICT与无训练组别的效果差异[17-18,40-46,33-39,49,59];有6项研究对HIIT与无训练组别的效果差异进行比较[34,46,49,51,53,62];7项研究直接比较了MICT与HIIT效果差异 [34,46-50,59];4项研究包含多个干预组,将MICT和HIIT与对照组相结合[34,46,49,59];1项研究具有多个对照组,包括MICT对久坐个体以及2型糖尿病患者生活质量的影响[40]。有2项研究对每周2次的低量HIIT与高量HIIT的效果差异进行比较[34,54];2项研究统计了每周2次的HIIT与每周3次的HIIT与不训练相比对生活质量的身心组成部分的影响[52-53]。 干预时长6-48周不等,其中8周[17,36,42,53,62],12周的干预最为常见[33,35,38,47-50,54-56,59]。锻炼频率每周2-5次,大多数研究采用每周3次的训练频率[17-18,37-40,46,49,53,59,61-62]。有3项研究采用了无监督的锻炼方式[33,36,41]。 2.4 纳入研究质量评价结果 图3概括了偏倚风险评估的结果。在32项研究中,有15项在偏倚风险评估的4个或更多领域中具有不明确或高风险[17,33,35,38-41,44,50,52-53,55-56,59,62],其中最常见的偏倚风险与结果评估中的盲法和分配隐藏的不充分实施有关。 2.5 Meta分析结果 2.5.1 HIIT对体力活动不足成人总体生活质量的影响 有15篇随机对照试验的结果显示,HIIT与无训练组别相比对体力活动不足成人的总体生活质量有显著的积极影响(Hedges’ g=0.61,95%CI:0.40–0.83,P < 0.01)[34,46,49,51-62],见图4。研究间异质性为中等(I2=45%,P=0.02,PI:–0.01–1.22),见图4。敏感性分析证实HIIT对总体生活质量的积极影响(Hedges’ g=0.50,95%CI:0.35–0.65,"
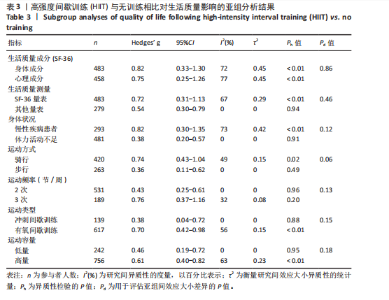
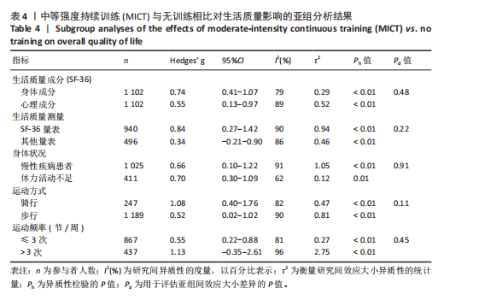
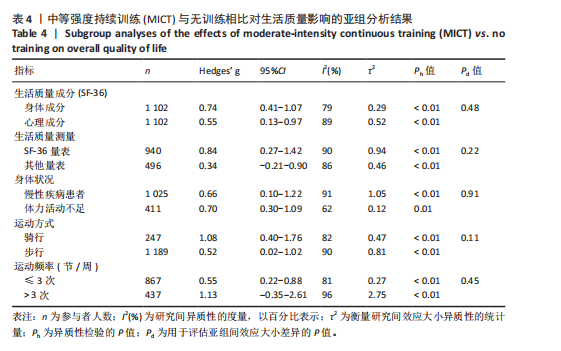
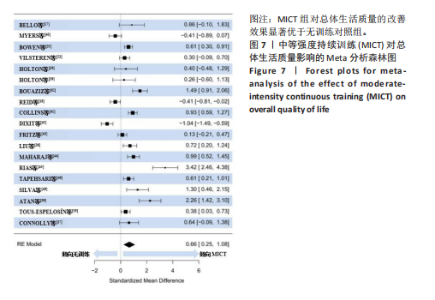
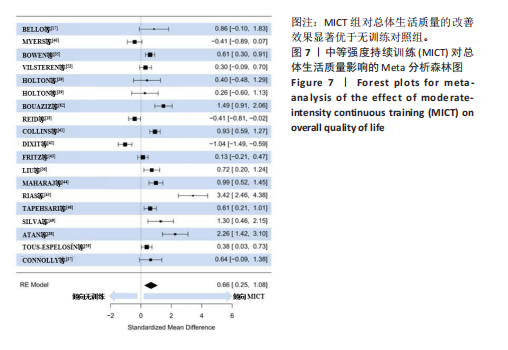
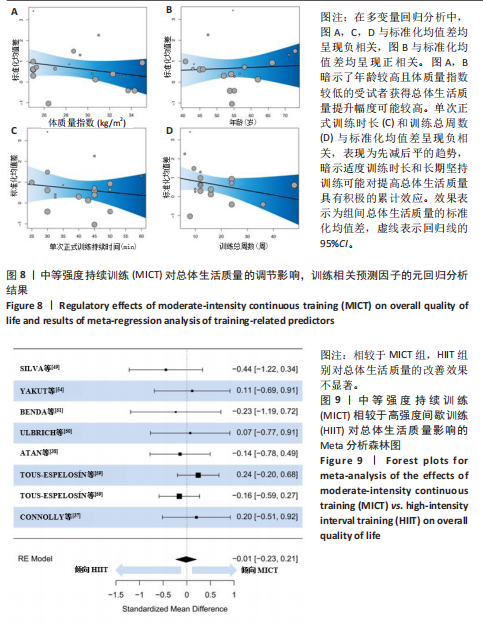
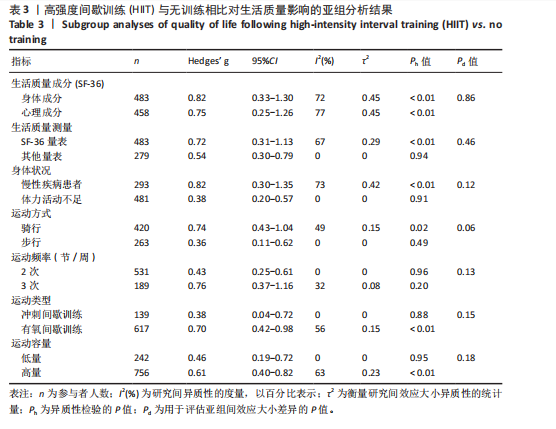
P=0.63)。Egger’s检验表明,主效应的合并结果无发表偏倚(P=0.05),详见漏斗图5A。 亚组分析结果见表3,HIIT在提升生活质量的身体成分方面效果更佳(Hedges’ g=0.82 vs. 0.75)。此外,参与者基线健康状况和运动方式显示出显著趋势,会影响HIIT对总体生活质量的提升效果。慢性疾病患者通过HIIT获得的改善幅度更大(Hedges’ g=0.82 vs. 0.38),且骑行能够更有效地改善总体生活质量(Hedge’s g=0.74 vs. 0.36)。测量方式、运动频率、类型和容量对HIIT效果的调节影响不显著(P > 0.05)。 回归分析结果表明,在HIIT组中,受试者的年龄40–60岁,体质量指数在25–40 kg/m2分布较为均匀。单次训练的持续时间范围为30 s–9 min,训练总周数一般为6–24周,间歇时间为30 s–3 min,每节训练的重复次数通常为2–5次。同时,文章未发现参与者的体质量指数、年龄、单次训练持续时间、总训练时长、每次训练的重复次数、恢复间隔对HIIT影响总体生活质量的调节作用显著(P > 0.05),见图6。 2.5.2 MICT对体力活动不足成人总体生活质量的影响 荟萃分析纳入了18篇文献[17-18,33-46,49,59]。结果显示,与无训练组别相比,MICT对体力活动不足成人的总体生活质量产生显著的积极影响(Hedges’ g=0.66,95%CI:0.24–1.08,P < 0.01),见图7。此外,这些研究间存在显著异质性 (I2=92%,P < 0.01,PI:–1.23–2.55),见图7。敏感性分析进一步证实了MICT相较于无训练状态下能显著提高总体生活质量 (Hedges’ g=0.66,95%CI:0.24–1.08,P < 0.01)。Egger’s检验显示主效应合并结果不存在发表偏倚(P=0.11),详见图5B。 亚组分析结果见表4,MICT在改善身体层面的生活质量方面效果更佳(Hedge’s g=0.74 vs. 0.55);运动方式显示出显著趋势,其中骑行在提高生活质量方面呈现出更优的趋势(Hedge’s g=1.08 vs. 0.52)。其他亚组分析未发现受试者的身体状况、运动频率和生活质量测量方式存在显著影响(P > 0.05)。"

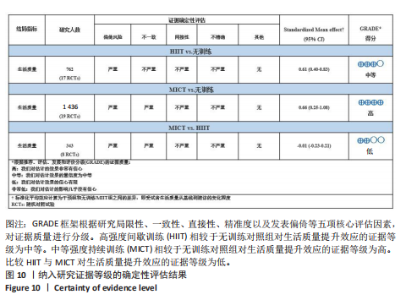
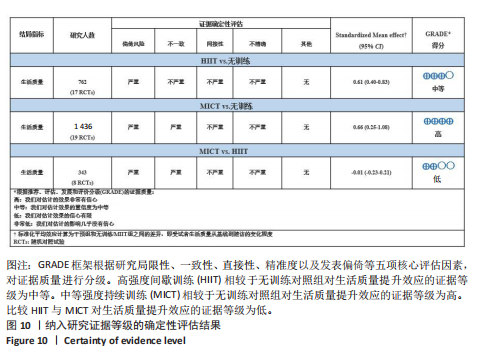
回归分析的结果显示,在MICT组中,受试者年龄集中在50–60岁,体质量指数分布均匀,介于25–35 kg/m2。单次训练时长通常在25–60 min,总训练周数多在8–24周范围内。文章未观察到参与者的体质量指数、年龄、单次训练时长或总训练时长对MICT总体生活质量影响的显著调节作用(P > 0.05),见图8。 2.5.3 HIIT与MICT对体力活动不足成人总体生活质量的效果差异 文章汇总了8篇随机对照试验的结果[17,34,46,49,52-54,59]。结果显示,针对体力活动不足成人,HIIT和MICT对总体生活质量的影响并不显著,且无显著性意义(Hedges’ g=–0.01,95%CI:–0.23–0.21,P=0.81),见图9。敏感性分析也显示,HIIT与MICT在提高总体生活质量方面的效果无显著差异(Hedges’ g=–0.01,95%CI:–0.23–0.21,P=0.81)。Egger’s检验显示主效应合并结果无发表偏倚(P=0.59),详见图5C。由于以下2个原因,未能进行进一步的亚组和回归分析:①关于比较HIIT与MICT的研究数量有限;②在直接比较HIIT与MICT在改善总体生活质量的效果差异方面,研究之间的异质性较低(I2=0)。 2.6 证据等级评价结果 文章采用GRADE方法对研究结果的确证性进行评估,见图10。由于部分纳入研究存在方法学偏差以及汇总结果的高异质性,HIIT对总体生活质量影响的证据确证性被评定为“中等”。同样,由于相同的原因,MICT对总体生活质量影响的证据也被降级。但考虑到MICT组别纳入的研究与试验数量最多,以及合并结果显示的大效应量,使得MICT对总体生活质量的影响被认为是“高”。此外,由于部分纳入研究的方法学偏差,HIIT与MICT在改善总体生活质量方面的证据等级被认为是“低”。"

| [1] KERR NR, BOOTH FW. Contributions of physical inactivity and sedentary behavior to metabolic and endocrine diseases. Trends Endocrinol Metab. 2022;33(12):817-827. [2] LEE IM, SHIROMA EJ, LOBELO F, et al. Effect of physical inactivity on major Non-communicable diseases worldwide: an analysis of burden of disease and life Expectancy. Lancet. 2012;380(9838): 219-229. [3] BHUI K, FLETCHER A. Common mood and anxiety states: gender differences in the protective effect of physical activity. Soc Psychiatry Psychiatr Epidemiol. 2000;35(1): 28-35. [4] DUNN AL, TRIVEDI MH, NEAL HA. Physical activity dose-response effects on outcomes of depression and anxiety. Med Sci Sports Exerc. 2001;33(Suppl):S587-S597. [5] GOODWIN RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;36(6):698-703. [6] TU WJ, SUN H, YAN F, et al. China trends in physical inactivity from 2013 to 2019: an analysis of 4.23 million participants. Med Sci Sports Exerc. 2024;56(3):528-535. [7] BURCKHARDT CS, ANDERSON KL. The Quality of Life Scale (QOLS): reliability, validity, and utilization. Health Qual Life Outcomes. 2003;1:60. [8] ANONYMOUS. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995; 41(10):1403-1409. [9] WU XY, HAN LH, ZHANG JH, et al. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: a systematic review. PLoS ONE. 2017;12(11):e0187668. [10] SCARABOTTOLO CC, TEBAR WR, ARAÚJO GUERRA PH, et al. Association between different domains of sedentary behavior and health-related quality of life in adults: a longitudinal study. Int J Environ Res Public Health. 2022;19(24):16389. [11] STAMATAKIS E, GALE J, BAUMAN A, et al. Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol. 2019;30;73(16):2062-2072. [12] PHYO AZZ, FREAK-POLI R, CRAIG H, et al. Quality of life and mortality in the general population: a systematic review and meta-analysis. BMC Public Health. 2020;20(1):1596. [13] REBAR AL, DUNCAN MJ, SHORT C, et al. Differences in Health-related quality of life between three clusters of physical activity, sitting time, depression, anxiety, and stress. BMC Public Health. 2014;14(1):1088. [14] MARQUEZ DX, AGUIÑAGA S, VÁSQUEZ PM, et al. A systematic review of physical activity and quality of life and well-being. Transl Behav Med. 2020;10(5):1098-1109. [15] SABAG A, CHANG CR, FRANCOIS ME, et al. The effect of exercise on quality of life in type 2 diabetes: a systematic review and meta-analysis. Med Sci Sports Exerc. 2023;1;55(8):1353-1365. [16] GRIFFITHS M, EDWARDS JJ, MCNAMARA J, et al. The effects of high intensity interval training on quality of life: a systematic review and meta-analysis. J Public Health. 2024. doi: 10.1007/s10389-024-02192-4. [17] BELLO AI, OWUSU-BOAKYE E, ADEGOKE BO, et al. Effects of aerobic exercise on selected physiological parameters and quality of life in patients with type 2 diabetes mellitus. Int J Gen Med. 2011;4:723-727. [18] REID RD, TULLOCH HE, SIGAL RJ, et al. Effects of aerobic exercise, resistance exercise or both, on patient-reported health status and well-being in type 2 diabetes mellitus: a randomised trial. Diabetologia. 2010;53(4):632-640. [19] PAGE MJ, MCKENZIE JE, BOSSUYT PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. [20] SHEA BJ, REEVES BC, WELLS G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or Both. BMJ. 2017. doi: 10.1136/bmj.j4008. [21] BULL FC, AL-ANSARI SS, BIDDLE S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451-1462. [22] GBD OBESITY COLLABORATORS. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13-27. [23] GUTHOLD R, STEVENS GA, RILEY LM, et al. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6(10):e1077-e1086. [24] MARENGONI A, ANGLEMAN S, MELIS R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430-439. [25] HAJAT C, STEIN E. The global burden of multiple chronic conditions: a narrative review. Prev Med Rep. 2018;12:284-293.
[26] COATES AM, JOYNER MJ, LITTLE JP, et al. A perspective on high-intensity interval training for performance and health. Sports Med. 2023;53(S1):85-96. [27] CUMPSTON M, LI T, PAGE MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10ED000142. [28] TAKESHIMA N, SOZU T, TAJIKA A, et al. Which is more generalizable, powerful and interpretable in meta-analyses, mean difference or standardized mean difference? BMC Med Res Methodol. 2014;14:30. [29] NAKAGAWA S, NOBLE DWA, SENIOR AM, et al. Meta-evaluation of meta-analysis: ten appraisal questions for biologists. BMC Biol. 2017;15(1):18. [30] NAGASHIMA K, NOMA H, FURUKAWA T A. Prediction intervals for random-effects meta-analysis: a confidence distribution approach. Stat Methods Med Res. 2019; 28(6):1689-1702. [31] PETERS JL, SUTTON AJ, JONES DR, et al. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol. 2008;61(10):991-996. [32] EGGER M, SMITH GD, SCHNEIDER M, et al. Bias in Meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629-634. [33] TAPEHSARI B, ALIZADEH M, KHAMSEH M, et al. Physical activity and quality of life in people with type 2 diabetes mellitus: a randomized controlled trial. Int J Prev Med. 2020;24:11:9 [34] TOUS-ESPELOSÍN M, GOROSTEGI-ANDUAGA I, CORRES P, et al. Impact on health-related quality of life after different aerobic exercise programs in physically inactive adults with overweight/obesity and primary hypertension: data from the EXERDIET-HTA study. IJERPH. 2020;17(24):9349. [35] VAN VILSTEREN MCBA, DE GREEF MHG, HUISMAN RM. The effects of a Low-to-moderate intensity pre-conditioning exercise programme linked with exercise counselling for sedentary haemodialysis patients in The Netherlands: results of a randomized clinical trial. Nephrol Dial Transplant. 2005;20(1):141-146. [36] RIAS YA, KURNIAWAN AL, CHANG CW, et al. Synergistic effects of regular walking and alkaline electrolyzed water on decreasing inflammation and oxidative stress, and increasing quality of life in individuals with type 2 diabetes: a community based randomized controlled trial. Antioxidants. 2020;9(10):946. [37] MYERS VH, MCVAY MA, BRASHEAR MM, et al. Exercise training and quality of life in individuals with type 2 diabetes. Diabetes Care. 2013;36(7):1884-1890. [38] MAHARAJ SS, NUHU JM. The effect of rebound exercise and treadmill walking on the quality of life for patients with Non-insulin-dependent type 2 diabetes. Int J Diabetes Dev Ctries. 2015;35(S2):223-229. [39] LIU SX, YUE XW, LIU EP, et al. Effect of square aerobic exercise on cardiovascular risk factors and Health-related quality of life in Chinese women with type 2 diabetes. Int J Diabetes Dev Ctries. 2017;37(2):183-189. [40] HOLTON DR, COLBERG SR, NUNNOLD T, et al. The effect of an aerobic exercise training program on quality of life in type 2 diabetes. Diabetes Educ. 2003;29(5):837-846. [41] FRITZ T, CAIDAHL K, OSLER M, et al. Effects of Nordic walking on health‐related quality of life in overweight individuals with Type 2 diabetes mellitus, impaired or normal glucose tolerance. Diabet Med. 2011;28(11):1362-1372. [42] DIXIT S, MAIYA A, SHASTRY B. Effect of aerobic exercise on quality of life in population with diabetic peripheral neuropathy in type 2 diabetes: a single blind, randomized controlled trial. Qual Life Res. 2014;23(5):1629-1640. [43] COLLINS TC, LUNOS S, CARLSON T, et al. Effects of a home-based walking intervention on mobility and quality of life in people with diabetes and peripheral arterial disease. Diabetes Care. 2011;34(10):2174-2179. [44] BOWEN DJ, FESINMEYER MD, YASUI Y, et al. Randomized trial of exercise in sedentary middle aged women: effects on quality of life. Int J Behav Nutr Phys Act. 2006;3(1):34. [45] BOUAZIZ W, SCHMITT E, VOGEL T, et al. Effects of a short-term interval aerobic training programme with active recovery bouts (IATP-R) on cognitive and mental health, functional performance and quality of life: a randomised controlled trial in sedentary Seniors. Int J Clin Pract. 2019;73(1):e13219. [46] ATAN T, KARAVELIOĞLU Y. Effectiveness of high-intensity interval training vs moderate-intensity continuous training in patients with fibromyalgia: a pilot randomized controlled trial. Arch Phys Med Rehabil. 2020;101(11):1865-1876. [47] YAKUT H, DURSUN H, FELEKOĞLU E, et al. Effect of home-based high-intensity interval training versus moderate-intensity continuous training in patients with myocardial infarction: a randomized controlled trial. Ir J Med Sci. 2022;191(6): 2539-2548. [48] ULBRICH AZ, ANGARTEN VG, SCHMITT NETTO A, et al. Comparative effects of high intensity interval training versus moderate intensity continuous training on quality of life in patients with heart failure: Study protocol for a randomized controlled trial. Clin Trials Regul Sci Cardiol. 2016;13:21-28. [49] SILVA MA. High intensity interval training improves Health-related quality of life in adults and older adults with diagnosed cardiovascular risk. JPES. 2019;2019:611. [50] BENDA NMM, SEEGER JPH, STEVENS GGCF, et al. Effects of high-intensity interval training versus continuous training on physical fitness, cardiovascular function and quality of life in heart failure patients. PLoS ONE. 2015;10(10):e0141256. [51] SUNDE S, HESSEBERG K, SKELTON DA, et al. Effects of a multicomponent high intensity exercise program on physical function and Health-related quality of life in older adults with or at risk of mobility disability after discharge from hospital: a randomised controlled Trial. BMC Geriatr. 2020;20(1):464. [52] STAVRINOU PS, BOGDANIS GC, GIANNAKI CD, et al. Effects of High-intensity interval training frequency on perceptual responses and future physical activity participation. Appl Physiol Nutr Metab. 2019;44(9): 952-957. [53] STAVRINOU PS, BOGDANIS GC, GIANNAKI CD, et al. High-intensity interval training frequency: cardiometabolic effects and quality of life. Int J Sports Med. 2018;39(3): 210-217. [54] RELJIC D, FRENK F, HERRMANN HJ, et al. Maximum heart rate- and lactate threshold-based low-volume high-intensity interval training prescriptions provide similar health benefits in metabolic syndrome patients. Healthcare (Basel). 2023;11(5):711. [55] RELJIC D, FRENK F, HERRMANN HJ, et al. Effects of very low volume high intensity versus moderate intensity interval training in obese metabolic syndrome patients: a randomized controlled study. Sci Rep. 2021;11(1):2836. [56] RELJIC D, FRENK F, HERRMANN HJ, et al. Low-volume high-intensity interval training improves cardiometabolic health, work ability and well-being in severely obese individuals: a randomized-controlled trial sub-study. J Transl Med. 2020;18(1):419. [57] RELJIC D, EICHHORN A, HERRMANN HJ, et al. Very low-volume, high-intensity interval training mitigates negative health impacts of COVID-19 pandemic-induced physical inactivity: 19. int j environ res public health. 2022;19(19):12308.
[58] METCALFE RS, ATEF H, MACKINTOSH K, et al. Time-efficient and computer-guided sprint interval exercise training for improving health in the workplace: a randomised mixed-methods feasibility study in office-based employees. BMC Public Health. 2020;20(1):313.
[59] CONNOLLY LJ, BAILEY SJ, KRUSTRUP P, et al. Effects of Self-paced interval and continuous training on health markers in women. Eur J Appl Physiol. 2017;117(11):2281-2293. [60] BALLIN M, LUNDBERG E, SÖRLÉN N, et al. Effects of interval training on quality of life and cardiometabolic risk markers in older adults: a randomized controlled trial. Clin Interv Aging. 2019;14:1589-1599. [61] ALARCÓN-GÓMEZ J, CHULVI-MEDRANO I, MARTIN-RIVERA F, et al. Effect of high-intensity interval training on quality of life, sleep quality, exercise motivation and enjoyment in sedentary people with type 1 diabetes mellitus. Int J Environ Res Public Health. 2021;18(23):12612. [62] ABDELBASSET WK, TANTAWY SA, KAMEL DM, et al. A randomized controlled trial on the effectiveness of 8-week high-intensity interval exercise on intrahepatic triglycerides, visceral lipids, and health-related quality of life in diabetic obese patients with nonalcoholic fatty liver disease. Medicine. 2019;98(12):e14918. [63] EDWARDS JJ, GRIFFITHS M, DEENMAMODE AHP, et al. High-intensity interval training and cardiometabolic health in the general population: a systematic review and meta-analysis of randomised controlled trials. Sports Med. 2023;53(9):1753-1763. [64] MILLET GP, VLECK VE, BENTLEY DJ. Physiological differences between cycling and running: lessons from triathletes. Sports Med. 2009;39(3):179-206. [65] COLBERG SR, ALBRIGHT AL, BLISSMER BJ, et al. Exercise and type 2 diabetes: american college of sports medicine and the american diabetes association: joint position statement. exercise and type 2 diabetes. Med Sci Sports Exerc. 2010;42(12):2282-2303. [66] TANG Y, WANG D, WANG Y, et al. Do surface slope and posture influence lower extremity joint kinetics during cycling? Int J Environ Res Public Health. 2020;17(8):2846. [67] YIN M, LI H, BAI M, et al. Is low-volume high-intensity interval training a time-efficient strategy to improve cardiometabolic health and body composition? A meta-analysis. Appl Physiol Nutr Metab. 2024;49(3):273-292. [68] SABAG A, LITTLE JP, JOHNSON NA. Low-volume high-intensity interval training for cardiometabolic health. J Physiol. 2022; 600(5):1013-1026. [69] VOLLAARD NBJ, METCALFE RS. Research into the health benefits of sprint interval training should focus on protocols with fewer and shorter sprints. Sports Med. 2017;47(12):2443-2451. [70] VOLLAARD NBJ, METCALFE RS, WILLIAMS S. Effect of number of sprints in an sit session on change in vo2 max: a meta-analysis. Med Sci Sports Exerc. 2017;49(6):1147-1156. [71] YIN M, CHEN Z, LI Y. Chronic High-intensity interval training and moderate-intensity continuous training are both effective in increasing maximum fat oxidation during exercise in overweight and obese adults: a meta-analysis. J Exerc Sci Fit. 2023;21(4): 354-365. [72] KOOHKAN S, SCHAFFNER D, MILLIRON BJ, et al. The impact of a weight reduction program with and without meal-replacement on health related quality of life in middle-aged obese females. BMC Womens Health. 2014;14(1):45. [73] CILLI M, SERBEST K, KAYAOGLU E. The effect of body weight on joint torques in teenagers: investigation of sit-to-stand movement. Clin Biomech (Bristol, Avon). 2021;83:105288. [74] 殷明越,陈志力,李汉森,等.碎片化运动:兼具应用可行性与健康促进效果的新策略[J].西安体育学院学报,2023,40(5): 615-627. [75] GILLEN J B, GIBALA M J. Is High-intensity interval training a time-efficient exercise strategy to improve health and fitness? Appl Physiol Nutr Metab. 2014;39(3):409-412. [76] RELJIC D, LAMPE D, WOLF F, et al. Prevalence and predictors of dropout from high-intensity interval training in sedentary individuals: a meta-analysis. Scand J of Med Sci Sports. 2019;29(9):1288-1304. [77] DUNSTAN DW, DOGRA S, CARTER SE, et al. Sit less and move more for cardiovascular health: emerging insights and opportunities. Nat Rev. Cardiol 2021;18(9):637-648. [78] 黎涌明.高强度间歇训练对不同训练人群的应用效果[J].体育科学,2015,35(8):59-75,96. [79] CAI H, LI G, ZHANG P, et al. Effect of exercise on the quality of life in type 2 diabetes mellitus: a systematic review. Qual Life Res. 2017;26(3):515-530. [80] MARKER AM, STEELE RG, NOSER AE. Physical activity and Health-related quality of life in children and adolescents: a systematic review and meta-analysis. Health Psychol. 2018;37(10):893-903. [81] KHURSHID S, AL-ALUSI MA, CHURCHILL TW, et al. Accelerometer-derived, weekend warrior, physical activity and incident cardiovascular disease. JAMA. 2023;330(3): 247-252. [82] KRAWCZYK-SUSZEK M, KLEINROK A. Health-Related Quality of Life (HRQoL) of people over 65 years of age. Int J Environ Res Public Health. 2022;19(2):625. [83] SAHLE BW, SLEWA-YOUNAN S, MELAKU YA, et al. A Bi-directional association between weight change and health-related quality of life: evidence from the 11-year follow-up of 9916 community-dwelling adults. Qual Life Res. 2020;29(6):1697-1706. [84] MATURANA FM, MARTUS P, ZIPFEL S, et al. Effectiveness of HIIE versus MICT in improving cardiometabolic risk factors in health and disease: a meta-analysis. Med Sci Sports Exerc. 2021;53(3):559-573. [85] SULTANA RN, SABAG A, KEATING SE, et al. The effect of low-volume high-intensity interval training on body composition and cardiorespiratory fitness: a systematic review and meta-analysis. Sports Med. 2019;49(11):1687-1721. [86] BATACAN RB, DUNCAN MJ, DALBO VJ, et al. Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. Br J Sports Med. 2017;51(6):494-503. [87] FLEG JL. Salutary effects of High-intensity interval training in persons with elevated cardiovascular risk. F1000Res. 2016;5:F1000 Faculty Rev-2254. [88] ROGNMO Ø, HETLAND E, HELGERUD J, et al. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil. 2004;11(3):216-222. [89] WEWEGE MA, AHN D, YU J, et al. High‐intensity interval training for patients with cardiovascular disease—is it safe? A systematic review. J Am Heart Assoc. 2018;6;7(21):e009305. [90] EKKEKAKIS P. Extraordinary claims in the literature on High-intensity interval training (HIIT): IV. is HIIT associated with higher long-term exercise adherence? Psychol Sport Exerc. 2023;64:102295. [91] SANTOS A, BRAATEN K, MACPHERSON M, et al. Rates of compliance and adherence to high-intensity interval training: a systematic review and meta-analyses. Int J Behav Nutr Phys Act. 2023;20(1):134. [92] MARTLAND R, MONDELLI V, GAUGHRAN F, et al. Can high-intensity interval training improve physical and mental health outcomes? A meta-review of 33 systematic reviews across the lifespan. J Sports Sci. 2020;38(4):430-469. [93] GIELEN S, LAUGHLIN M H, O’CONNER C, et al. Exercise training in patients with heart disease: review of beneficial effects and clinical recommendations. Prog Cardiovasc Dis. 2015;57(4):347-355. [94] 黎涌明,殷明越,李博,等.运动与训练科学的五大“论战”[J].首都体育学院学报,2024,36(1):22-33. [95] STAMATAKIS E, AHMADI MN, GILL JMR, et al. Association of wearable device-measured vigorous intermittent lifestyle physical activity with mortality. Nat Med. 2022;28(12):2521-2529. |
| [1] | Gao Feng, Zhang Jun, Yu Wenjun, Chanyu Yujing, Zhao Le, Hu Yuting, Wang Junhua, Liu Yongfu. Effects of wrist-hand orthosis on hand dysfunction in stroke patients: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2124-2131. |
| [2] | Zheng Yin, Wu Zhenhua, Zhang Cheng, Ruan Kexin, Gang Xiaolin, Ji Hong. Safety and efficacy of immunoadsorption therapy for rheumatoid arthritis: a network meta-analysis and systematic review [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1260-1268. |
| [3] | Chen Qiang, Wu Wenjuan, Jiang Shuhua, Huang Da. Physical exercise improves physical function in burn patients: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1269-1281. |
| [4] | Leng Xiaoxuan, Zhao Yuxin, Liu Xihua. Effects of different neuromodulatory stimulation modalities on non-motor symptoms in Parkinson’s patients: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1282-1293. |
| [5] | Wen Xiaolong, Weng Xiquan, Feng Yao, Cao Wenyan, Liu Yuqian, Wang Haitao. Effects of inflammation on serum hepcidin and iron metabolism related parameters in patients with type 2 diabetes mellitus: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1294-1301. |
| [6] | Jiang Yang, Peng Hao, Song Yanping, Yao Na, Song Yueyu, Yin Xingxiao, Li Yanqi, Chen Qigang. Isometric exercise reduces resting blood pressure: a meta-analysis of moderating factors and dose effects [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 975-986. |
| [7] | Li Hanyue, Li Yini, Xiang Linmei, Li Sen. Effects of resistance exercise therapy on pain and function in patients with cervical spondylotic radiculopathy: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 987-996. |
| [8] | Sun Jiahe, Shi Jipeng, Zhu Tianrui, Quan Helong, Xu Hongqi. Effect of exercise intervention in elderly individuals with sarcopenia and its comorbidities: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 997-1007. |
| [9] | Yang Yuanyuan, Zhou Shanshan, Cheng Xiaofei, Feng Luye, Tang Jiqin. Network meta-analysis of non-invasive brain stimulation in the treatment of lower limb motor dysfunction after stroke [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1008-1018. |
| [10] | Yang Peng, Xu Chenghan, Zhou Yingjie, Chai Xubin, Zhuo Hanjie, Li Lin, Shi Jinyu. A meta-analysis of risk factors for residual back pain after vertebral augmentation for osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 731-739. |
| [11] | Zhang Xinxin, Gao Ke, Xie Shidong, Tuo Haowen, Jing Feiyue, Liu Weiguo. Network meta-analysis of non-surgical treatments for foot and ankle ability and dynamic balance in patients with chronic ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1931-1944. |
| [12] | Sun Yundi, Cheng Lulu, Wan Haili, Chang Ying, Xiong Wenjuan, Xia Yuan. Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1945-1952. |
| [13] | Wang Yida, Liu Jun, Wang Xiaoling, Wang Liyan, Yang Chengru, Zhang Xuexiao. Effects of wearable electronic device-based interventions on physical activity and sedentary behavior in healthy adolescents: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1693-1704. |
| [14] | Zhang Zixian, Xu Youliang, Wu Shaokui, Wang Xiangying. Effects of blood flow restriction training combined with resistance training on muscle indicators in college athletes: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1705-1713. |
| [15] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||