Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (8): 1714-1726.doi: 10.12307/2025.312
Previous Articles Next Articles
Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br#
Wang Juan, Wang Guanglan, Zuo Huiwu
- School of Sports Medicine, Wuhan Sports University, Wuhan 430079, Hubei Province, China
-
Received:2024-03-07Accepted:2024-03-29Online:2025-03-18Published:2024-07-06 -
Contact:Wang Guanglan, Professor, School of Sports Medicine, Wuhan Sports University, Wuhan 430079, Hubei Province, China Corresponding author: Zuo Huiwu, Master, School of Sports Medicine, Wuhan Sports University, Wuhan 430079, Hubei Province, China -
About author:Wang Juan, Master, Intermediate experimentalist, School of Sports Medicine, Wuhan Sports University, Wuhan 430079, Hubei Province, China -
Supported by:Teaching and Research Project of Hubei Province Department of Education, No. 2021407 (to WJ)
CLC Number:
Cite this article
Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br#[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
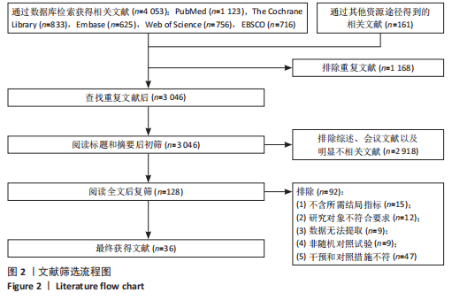
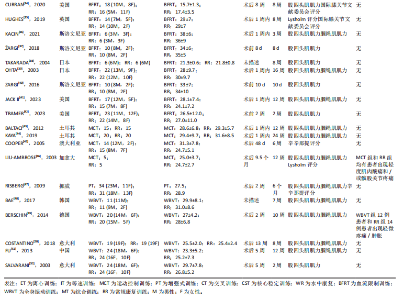
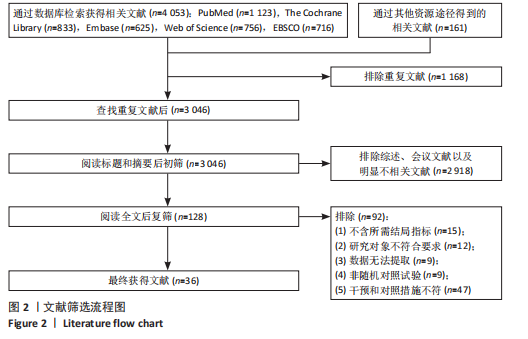
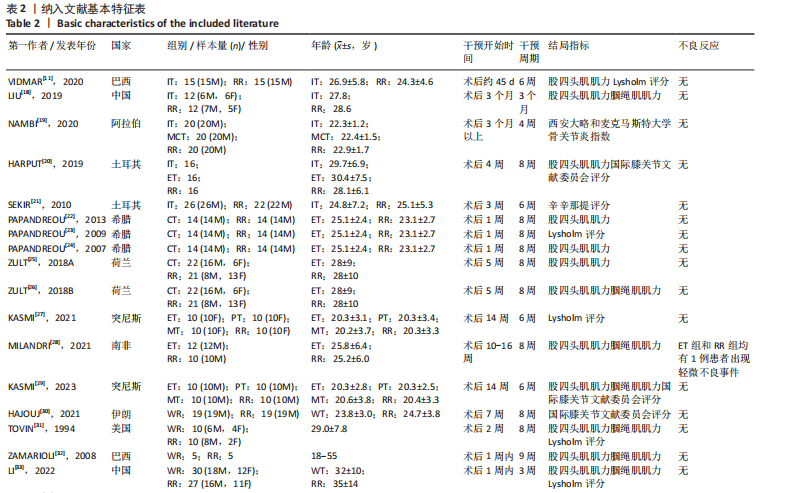
2.1 文献筛选流程及结果 初步检索获得4 053篇文献,采用EndNote X9.1软件剔除重复发表文献1 168篇,剩余3 046篇;阅读文章标题摘要,排除综述、会议文献以及明显不相关的文献2 918篇,剩余128篇;阅读剩余文章具体内容,严格按照文献纳入和排除标准进一步筛选,排除不含所需结局指标、研究对象不符合要求、数据无法提取、非随机对照试验、干预和对照措施不符的文献92篇,最终纳入36项随机对照试验[11,18-52],文献筛选流程见图2。 2.2 纳入文献基本特征 共纳入1 179例前交叉韧带重建后患者,年龄多在18-38岁;干预开始时间最早为术后1周内,最晚为术后9.5个月;干预周期最短为10 d,最长为6个月。共29项研究报告了股四头肌肌力[11,18,20,22,24-26,28-29,31-34,36-44,46-52];18项研究报告了腘绳肌肌力[18,26,28-29,31-33,36,39,41,43-44,46-51];15项研究报告了膝关节功能评分[11,19-21,23,27,29-31,33-35,45-47],包括Lysholm评分7项[11,23,27,31,33,35,46]、国际膝关节文献委员会评分5项[20,29-30,34,35]、西安大略和麦克马斯特大学骨关节炎指数1项[19]、辛辛那提评分3项[21,45,47],其中一项研究同时报告了Lysholm评分和国际膝关节文献委员会评分[35],由于Lysholm评分、国际膝关节文献委员会评分和辛辛那提评分越高代表膝关节功能越好,而西安大略和麦克马斯特大学骨关节炎指数评分越低代表膝"
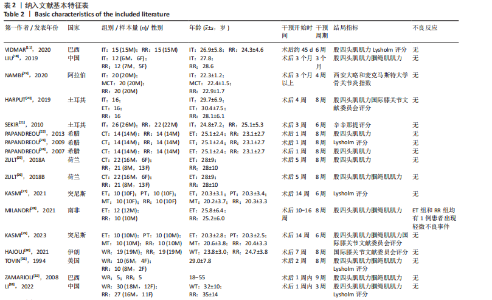
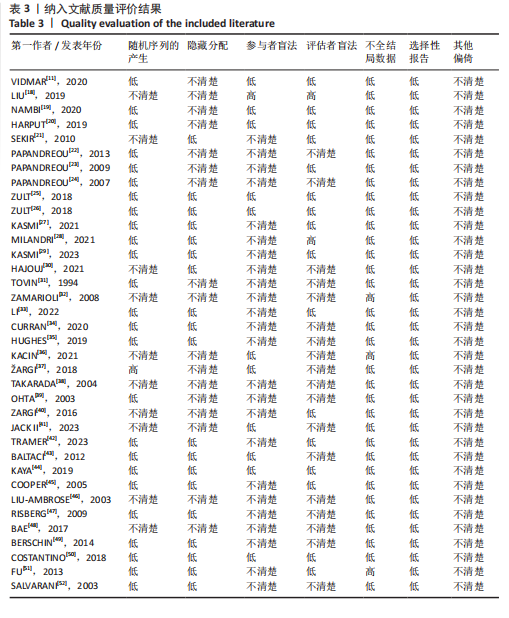
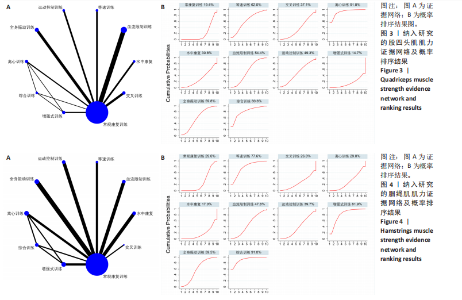
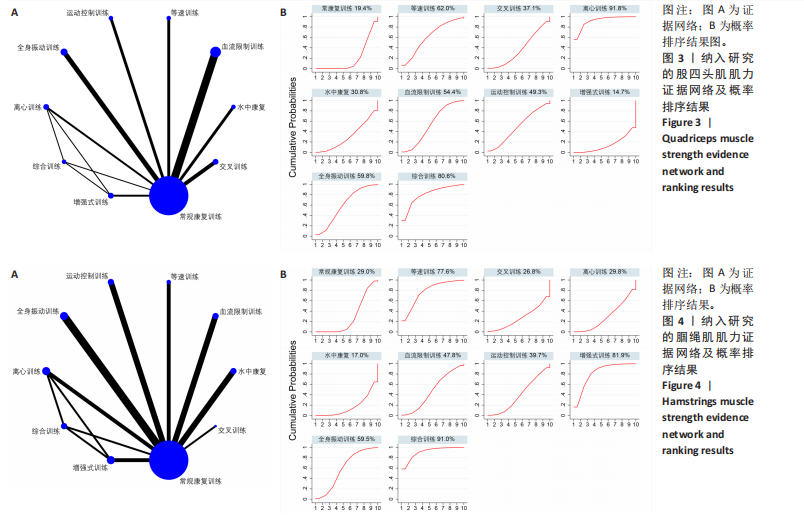
关节功能越好,故文章将西安大略和麦克马斯特大学骨关节炎指数数据做负向处理后再与其他数据进行比较,纳入研究的基本特征见表2。 2.3 纳入研究的质量评价结果 在纳入的36项研究中,26项研究报告了随机序列产生的具体方法[11,19-20,22-29,31,33-35,37,39,42-45,47,49-50,52],主要为随机数字表法和计算机随机序列法,其中1项研究采用分层随机法[37],10项仅提及随机[18,21,30,32,36,38,40-41,46,48],未描述具体方法;19项研究采用分配隐藏[21,25-30,33-35,42-45,47,49-52];盲法方面,7项研究使用双盲[11,19-20,25-26,44,50],13项使用单盲[21,23,27,29,33,36-37,40-43,45,51],剩余研究未提及盲法;有3项研究存在病例脱落[32,36,51];未发现选择性报告,不清楚其是否存在其他可能的偏倚;整体文献质量中等;详见表3。 2.4 Meta分析结果 2.4.1 股四头肌力量差异 该指标纳入的运动疗法共9种,包括等速训练、交叉训练、离心训练、水中康复、血流限制训练、运动控制训练、增强式训练、全身振动训练和综合训练,证据网络见图3A。节点分析模型显示股四头肌肌力指标P=0.128,说明股四头肌肌力指标整体的直接比较和间接比较结果一致,故采用一致性进行分析。使用节点劈裂法进行不一致检验,发现离心训练和综合训练直接比较和间接比较的结果存在不一致(P < 0.05),直接结果显示,离心训练对股四头肌肌力的提升效果显著优于综合训练(SMD=1.33,95%CI:0.34-2.31,P=0.009)。 网状Meta分析结果显示,离心训练(P=0.007)、血流限制训练(P=0.039)、全身振动训练(P=0.042)、综合训练(P=0.249)对股四头肌肌力的提升效果显著优于常规康复训练;而尚无证据表明等速训练(P=0.162)、交叉训练(P=0.548)、水中康复(P=0.806)、运动控制训练(P=0.349)、增强式训练(P=0.629)对股四头肌肌力的提升效果优于常规康复训练,详见表4。 直接Meta分析结果显示,离心训练(SMD=0.81,95%CI:0.09-1.53,P=0.03)、血流限制训练(SMD=0.43,95%CI:0.15-0.71,P=0.003)、全身振动训练(SMD=0.58,95%CI:0.25-0.92,P < 0.001)、综合训练(SMD=4.43,95%CI:2.66-6.19,P < 0.001)对股四头肌肌力的提升效果显著优于常规康复训练;离心训练对股四头肌肌力的提升效果显著优于综合训练(SMD=3.33,95%CI:1.88-4.77,P < 0.001)和增强式训练(SMD=1.33,95%CI:0.34-2.31,P=0.009);综合训练对股四头肌肌力的提升效果显著优于增强式训练(SMD=8.32,95%CI:5.31-11.33,P < 0.001),详见表5。 排序结果显示,9种运动疗法改善股四头肌肌力效果优劣顺序依次为:离心训练(SUCRA=91.8%)、综合训练(SUCRA=80.6%)、等速训练(SUCRA=62.0%)、全身振动训练(SUCRA=59.8%)、血流限制训练"
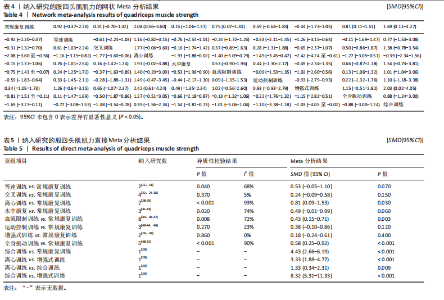
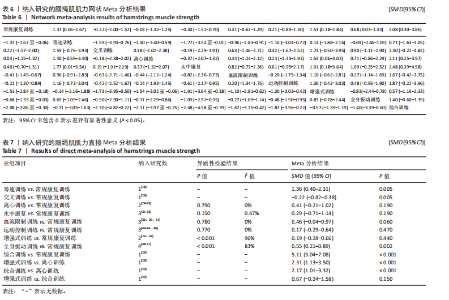
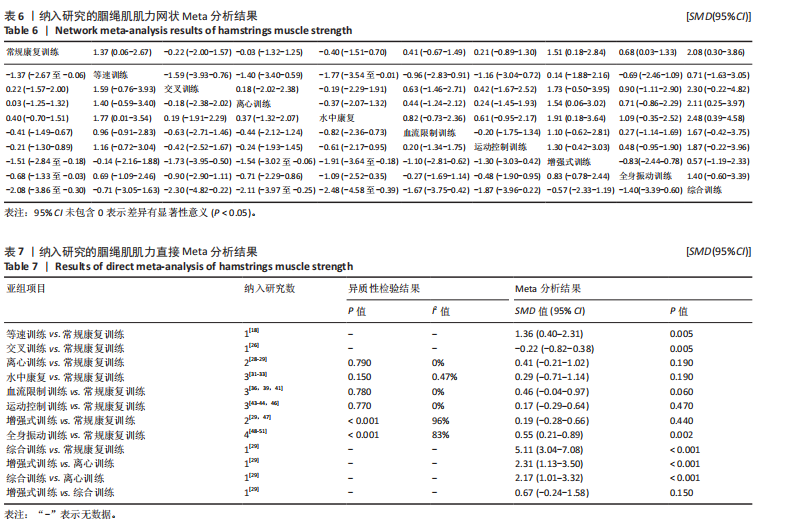
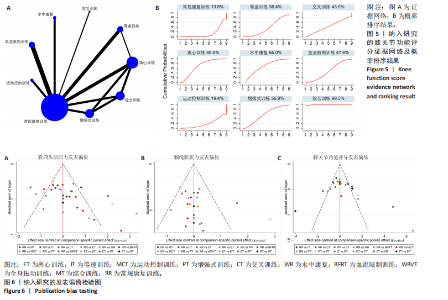
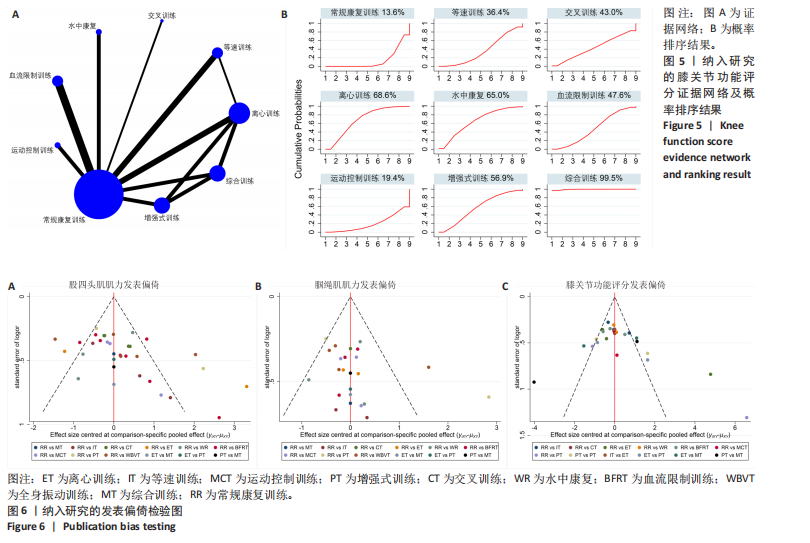
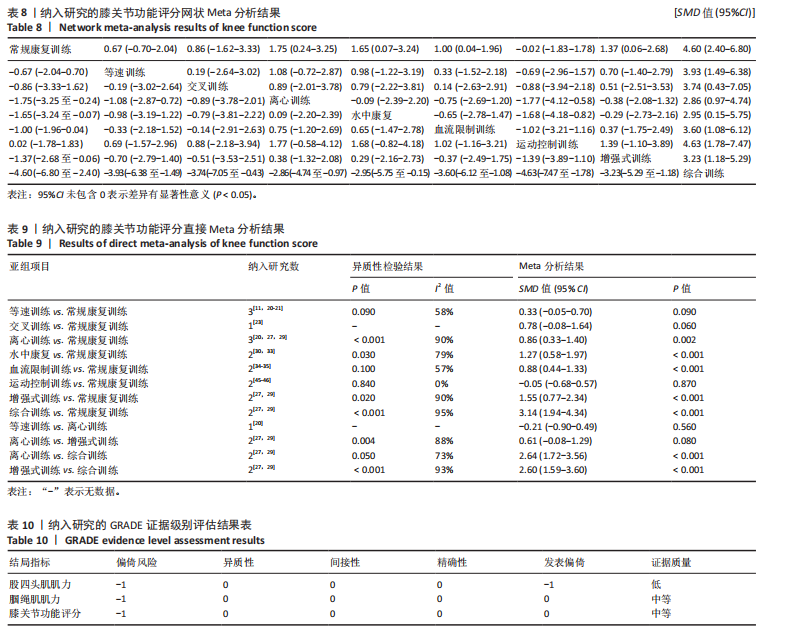
(SUCRA=54.4%)、运动控制训练(SUCRA=49.3%)、交叉训练(SUCRA=37.1%)、水中康复(SUCRA=30.8%)、增强式训练(SUCRA=14.7%),详见图3B。 2.4.2 腘绳肌力量差异 该指标纳入的运动疗法共9种,包括等速训练、交叉训练、离心训练、水中康复、血流限制训练、运动控制训练、增强式训练、全身振动训练、综合训练,证据网络见图4A。节点分析模型显示腘绳肌肌力指标P=0.112,说明腘绳肌肌力指标整体的结果较为一致,使用一致性模型进行分析;使用节点劈裂法进行不一致检验,发现增强式训练与常规康复训练直接比较和间接比较证据存在不一致(P < 0.05),直接Meta分析结果显示,与常规康复训练相比,增强式训练并不能显著提升腘绳肌肌力(SMD=0.19,95%CI:-0.28-0.66,P=0.440)。 网状Meta分析结果显示:等速训练(P=0.039)、增强式训练(P=0.026)、全身振动训练(P=0.048)、综合训练(P=0.022)对腘绳肌肌力的提升效果显著优于常规康复训练;而尚无证据表明交叉训练(P=0.811)、离心训练(P=0.960)、水中康复(P=0.473)、血流限制训练(P=0.456)、运动控制训练(P=0.714)对腘绳肌肌力的提升效果优于常规康复训练,详见表6。 9种运动疗法两两比较结果显示,等速训练(SMD=1.77,95%CI:0.01-3.54,P < 0.05)、增强式训练(SMD=1.91,95%CI:0.18-3.64,P < 0.05)和综合训练(SMD=2.48,95%CI:0.39-4.58,P < 0.05)对腘绳肌肌力的提升效果显著优于水中康复;此外,综合训练对腘绳肌肌力的提升效果显著优于离心训练(SMD=2.11,95%CI:0.25-3.97,P < 0.05);剩余两两比较结果比较未呈现显著性差异(P > 0.05),详见表6。 直接Meta分析结果显示,等速训练(SMD=1.36,95%CI:0.40-2.31,P=0.005)、全身振动训练(SMD=0.55,95%CI:0.21-0.89,P=0.002)、综合训练(SMD=5.11,95%CI:3.04-7.08,P < 0.001)对腘绳肌肌力的提升效果显著优于常规康复训练,增强式训练(SMD=2.31,95%CI:1.13-3.50,P < 0.001)和综合训练(SMD=2.17,95%CI:1.01-3.32,P < 0.001)对腘绳肌肌力的提升效果显著优于离心训练,详见表7。 排序结果显示,9种运动疗法改善腘绳肌肌力效果优劣顺序依次为:综合训练(SUCRA=91.0%)、增强式训练(SUCRA=81.9%)、等速训练(SUCRA=77.6%)、全身振动训练(SUCRA=59.5%)、血流限制训练(SUCRA=47.8%)、运动控制训练(SUCRA=39.7%)、离心训练(SUCRA=29.8%)、交叉训练(SUCRA=26.8%)、水中康复(SUCRA=17.0%),详见图4B。 2.4.3 膝关节功能评分差异 该指标纳入的运动疗法共8种,包括等速训练、交叉训练、离心训练、水中康复、血流限制训练、运动控制训练、增强式训练、综合训练,证据网络见图5A。节点分析模型显示膝关节功能评分指标P=0.463;使用节点劈裂法进行不一致检验,未发现局部不一致。说明肌肉疼痛指标的直接比较和间接比较结果一致,使用一致性模型进行分析。 网状Meta分析结果显示,离心训练(P=0.023)、水中康复(P=0.041)、血流限制训练(P=0.047)、增强式训练(P=0.040)、综合训练(P < 0.001)对膝关节功能评分的提升效果显著优于常规康复训练,而尚无证据表明等速训练(P=0.338)、交叉训练(P=0.496)、运动控制训练(P=0.980)对腘绳肌肌力的提升效果优于常规康复训练,详见表8。 8种运动疗法两两比较结果显示,综合训练对膝关节功能评分的提升效果显著优于等速训练(SMD=3.93,95%CI:1.49-6.38,P < 0.05)、交叉训练(SMD=3.74,95%CI:0.43-7.05,"

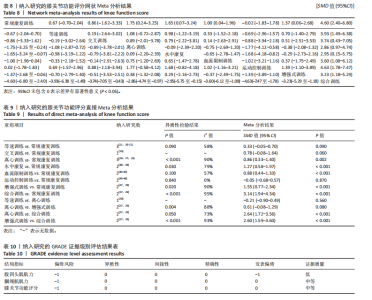
P < 0.05)、离心训练(SMD=2.86,95%CI:0.97-4.74,P < 0.05)、水中康复(SMD=2.95,95%CI:0.15-5.75,P < 0.05)、血流限制训练(SMD=3.60,95%CI:1.08-6.12,P < 0.05)、运动控制训练(SMD=4.68,95%CI:1.73-6.47,P < 0.05)、综合训练(SMD=3.23,95%CI:1.18-5.29,P < 0.05),剩余两两比较结果比较未呈现显著性差异(P > 0.05),详见表8。 直接Meta分析结果显示,水中康复(SMD=1.27,95%CI:0.58-1.97,P < 0.001)、血流限制训练(SMD=0.88,95%CI:0.44-1.33,P < 0.001)、增强式训练(SMD=1.55,95%CI:0.77-2.34,P < 0.001)、综合训练(SMD=3.14,95%CI:1.94-4.34,P < 0.001)对膝关节功能评分的提升效果显著优于常规康复训练;综合训练对膝关节功能评分的提升效果显著优于离心训练(SMD=2.64,95%CI:1.72-3.56,P < 0.001)和增强式训练(SMD=2.60,95%CI:1.59-3.60,P < 0.001),详见表9。 排序结果显示,8种运动疗法改善膝关节功能评分效果优劣顺序依次为:综合训练(SUCRA=99.5%)、离心训练(SUCRA=68.6%)、水中康复(SUCRA=65.0%)、增强式训练(SUCRA=56.9%)、血流限制训练(SUCRA=47.6%)、交叉训练(SUCRA=43.0%)、等速训练(SUCRA=36.4%)、运动控制训练(SUCRA=19.4%),详见图5B。 2.5 发表偏倚检验结果 对股四头肌肌力、腘绳肌肌力、膝关节功能评分3个结局指标进行发表偏倚检验;对于股四头肌肌力,漏斗图两侧对称性欠佳,提示存在一定发表偏倚风险,见图6A;对于腘绳肌肌力和膝关节功能评分,漏斗图基本对称,提示发表偏倚的可能性较小,但对结果的解释仍需谨慎对待,详见图6B,C。 2.6 纳入文献指标的证据强度等级 根据GRADE证据强度等级标准,文章结果的证据强度可因以下5个因素降级:①偏倚风险:大部分研究具体随机方式、隐藏分配及盲法的实施不消楚;②异质性:存在中等或以上异质性;③间接性:结局指标与评估目的关联不强;④精准性:置信区间宽;⑤发表偏倚:漏斗图不对称。纳入研究均为随机对照试验,但由于大部分研究具体随机方式、隐藏分配及盲法的实施不清楚,对3个结局指标进行降级;此外,股四头肌肌力指标漏斗图不对称,存在发表偏倚的风险较高,对股四头肌结局指标进行降级。因此,股四头肌肌力结局指标证据等级为低级,腘绳肌肌力及膝关节功能评分证据等级为中等,详见表10。"
| [1] WASHABAUGH EP, BROWN SR, PALMIERI-SMITH RM, et al. Functional resistance training differentially alters gait kinetics after anterior cruciate ligament reconstruction: a pilot study. Sports Health. 2023;15(3):372-381. [2] 陈鹏,左会武,王玲,等.前交叉韧带重建后运动员单腿垂直跳跃高度对称性掩盖其异常下肢生物力学[J].中国运动医学杂志,2023,42(12):939-947. [3] DAVEY MS, HURLEY ET, WITHERS D, et al. Anterior cruciate ligament reconstruction with platelet-rich plasma: a systematic review of randomized control trials. Arthroscopy. 2020;36(4):1204-1210. [4] BRINLEE AW, DICKENSON SB, HUNTER-GIORDANO A, et al. ACL reconstruction rehabilitation: clinical data, biologic healing, and criterion-based milestones to inform a return-to-sport guideline. Sports Health. 2022;14(5):770-779. [5] PALMIERI-SMITH RM, LEPLEY LK. Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sports Med. 2015;43(7):1662-1669. [6] ARDERN CL, TAYLOR NF, FELLER JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543-1552. [7] LEPLEY LK, PALMIERI-SMITH RM. Quadriceps strength, muscle activation failure, and patient-reported function at the time of return to activity in patients following anterior cruciate ligament reconstruction: a cross-sectional study. J Orthop Sports Phys Ther. 2015;45(12):1017-1025. [8] OBERLäNDER KD, BRüGGEMANN GP, HöHER J, et al. Altered landing mechanics in ACL-reconstructed patients. Med Sci Sports Exerc. 2013;45(3):506-513. [9] KOTSIFAKI A, VAN ROSSOM S, WHITELEY R, et al. Single leg vertical jump performance identifies knee function deficits at return to sport after ACL reconstruction in male athletes. Br J Sports Med. 2022;56(9):490-498. [10] SHIMIZU T, SAMAAN MA, TANAKA MS, et al. Abnormal biomechanics at 6 months are associated with cartilage degeneration at 3 years after anterior cruciate ligament reconstruction. Arthroscopy. 2019;35(2): 511-520. [11] VIDMAR MF, BARONI BM, MICHELIN AF, et al. Isokinetic eccentric training is more effective than constant load eccentric training for quadriceps rehabilitation following anterior cruciate ligament reconstruction: a randomized controlled trial. Braz J Phys Ther. 2020;24(5):424-432. [12] CHMIELEWSKI TL, GEORGE SZ, TILLMAN SM, et al. Low- versus high-intensity plyometric exercise during rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(3):609-617. [13] KıNıKLı GI, YüKSEL I, BALTACı G, et al. The effect of progressive eccentric and concentric training on functional performance after autogenous hamstring anterior cruciate ligament reconstruction: a randomized controlled study. Acta Orthop Traumatol Turc. 2014;48(3):283-289. [14] WIGGINS AJ, GRANDHI RK, SCHNEIDER DK, et al. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016; 44(7):1861-1876. [15] CINQUE ME, DORNAN GJ, CHAHLA J, et al. High rates of osteoarthritis develop after anterior cruciate ligament surgery: an analysis of 4108 patients. Am J Sports Med. 2018;46(8):2011-2019. [16] KOTSIFAKI R, KORAKAKIS V, KING E, et al. Aspetar clinical practice guideline on rehabilitation after anterior cruciate ligament reconstruction. Br J Sports Med. 2023;57(9):500-514. [17] OWEN PJ, MILLER CT, MUNDELL NL, et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. 2020;54(21):1279-1287. [18] LIU H, LU W, LIANG D, et al. Effect of isokinetic training of thigh muscle group on graft remodeling after anterior cruciate ligament reconstruction. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33(9):1088-1094. [19] NAMBI G, ABDELBASSET WK, ALRAWAIL SM, et al. Effects of isokinetic knee muscle training on bone morphogenetic proteins and inflammatory biomarkers in post-traumatic osteoarthritis after anterior cruciate ligament injury: a randomized trial. J Rehabil Med. 2020;52(9):jrm00098. [20] HARPUT G, ULUSOY B, YILDIZ TI, et al. Cross-education improves quadriceps strength recovery after ACL reconstruction: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):68-75. [21] SEKIR U, GUR H, AKOVA B. Early versus late start of isokinetic hamstring-strengthening exercise after anterior cruciate ligament reconstruction with patellar tendon graft. Am J Sports Med. 2010;38(3):492-500. [22] PAPANDREOU M, BILLIS E, PAPATHANASIOU G, et al. Cross-exercise on quadriceps deficit after ACL reconstruction. J Knee Surg. 2013; 26(1):51-58. [23] PAPANDREOU MG, BILLIS EV, ANTONOGIANNAKIS EM, et al. Effect of cross exercise on quadriceps acceleration reaction time and subjective scores (Lysholm questionnaire) following anterior cruciate ligament reconstruction. J Orthop Surg Res. 2009;4(1):2-10. [24] PAPANDREOU MG, NIKOS P, EMMANOUEL A, et al. The effect of cross exercise on quadriceps strength in different knee angles after the anterior cruciate ligament reconstruction. Brazilian J Biomotricity. 2007;1(4):123-138. [25] ZULT T, GOKELER A, VAN RAAY J, et al. Cross-education does not accelerate the rehabilitation of neuromuscular functions after ACL reconstruction: a randomized controlled clinical trial. Eur J Appl Physiol. 2018;118(8):1609-1623. [26] ZULT T, GOKELER A, VAN RAAY J, et al. Cross-education does not improve early and late-phase rehabilitation outcomes after ACL reconstruction: a randomized controlled clinical trial. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):478-490. [27] KASMI S, ZOUHAL H, HAMMAMI R, et al. The effects of eccentric and plyometric training programs and their combination on stability and the functional performance in the post-ACL-surgical rehabilitation period of elite female athletes. Front Physiol. 2021;12(7):688385. [28] MILANDRI G, SIVARASU S. A randomized controlled trial of eccentric versus concentric cycling for anterior cruciate ligament reconstruction rehabilitation. Am J Sports Med. 2021;49(3):626-636. [29] KASMI S, SARIATI D, HAMMAMI R, et al. The effects of different rehabilitation training modalities on isokinetic muscle function and male athletes’ psychological status after anterior cruciate ligament reconstructions. BMC Sports Sci Med Rehabil. 2023;15(1):43-53. [30] HAJOUJ E, HADIAN MR, MIR SM, et al. Effects of innovative aquatic proprioceptive training on knee proprioception in athletes with anterior cruciate ligament reconstruction: a randomized controlled trial. Arch Bone Jt Surg. 2021;9(5):519-526. [31] TOVIN BJ, WOLF SL, GREENFIELD BH, et al. Comparison of the effects of exercise in water and on land on the rehabilitation of patients with intra-articular anterior cruciate ligament reconstructions. Phys Ther. 1994;74(8):710-719. [32] ARIANE Z; ADRIANO P, EVANDRO M, et al. The significance of water rehabilitation in patients with anterior cruciate ligament reconstruction. Physiotherapy. 2008; 16(2):3-6. [33] LI D, ZHANG Q, LIU X, et al. Effect of water-based walking exercise on rehabilitation of patients following ACL reconstruction: a prospective, randomised, single-blind clinical trial. Physiotherapy. 2022;115(6):18-26. [34] CURRAN MT, BEDI A, MENDIAS CL, et al. Blood flow restriction training applied with high-intensity exercise does not improve quadriceps muscle function after anterior cruciate ligament reconstruction: a randomized controlled trial. Am J Sports Med. 2020;48(4):825-837. [35] HUGHES L, ROSENBLATT B, HADDAD F, et al. Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a uk national health service randomised controlled trial. Sports Med. 2019;49(11):1787-1805. [36] KACIN A, DROBNIČ M, MARŠ T, et al. Functional and molecular adaptations of quadriceps and hamstring muscles to blood flow restricted training in patients with ACL rupture. Scand J Med Sci Sports. 2021;31(8):1636-1646. [37] ŽARGI T, DROBNIČ M, STRAŽAR K, et al. Short-term preconditioning with blood flow restricted exercise preserves quadriceps muscle endurance in patients after anterior cruciate ligament reconstruction. Front Physiol. 2018;9(8):1150-1162. [38] TAKARADA Y, TSURUTA T, ISHII N. Cooperative effects of exercise and occlusive stimuli on muscular function in low-intensity resistance exercise with moderate vascular occlusion. Jpn J Physiol. 2004;54(6):585-592. [39] OHTA H, KUROSAWA H, IKEDA H, et al. Low-load resistance muscular training with moderate restriction of blood flow after anterior cruciate ligament reconstruction. Acta Orthop Scand. 2003; 74(1):62-68. [40] GRAPAR ZARGI T, DROBNIC M, JKODER J, et al. The effects of preconditioning with ischemic exercise on quadriceps femoris muscle atrophy following anterior cruciate ligament reconstruction: a quasi-randomized controlled trial. Eur J Phys Rehabil Med. 2016;52(3):310-320. [41] JACK RA 2ND, LAMBERT BS, HEDT CA, et al. Blood flow restriction therapy preserves lower extremity bone and muscle mass after ACL reconstruction. Sports Health. 2023;15(3):361-371. [42] TRAMER JS, KHALIL LS, JILDEH TR, et al. Blood flow restriction therapy for 2 weeks prior to anterior cruciate ligament reconstruction did not impact quadriceps strength compared to standard therapy. Arthroscopy. 2023;39(2):373-381. [43] BALTACI G, HARPUT G, HAKSEVER B, et al. Comparison between Nintendo Wii Fit and conventional rehabilitation on functional performance outcomes after hamstring anterior cruciate ligament reconstruction: prospective, randomized, controlled, double-blind clinical trial. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):880-887. [44] KAYA D, GUNEY-DENIZ H, SAYACA C, et al. Effects on lower extremity neuromuscular control exercises on knee proprioception, muscle strength, and functional level in patients with ACL reconstruction. Biomed Res Int. 2019;15(11):1694695. [45] COOPER RL, TAYLOR NF, FELLER JA. A randomised controlled trial of proprioceptive and balance training after surgical reconstruction of the anterior cruciate ligament. Res Sports Med. 2005; 13(3):217-230. [46] LIU-AMBROSE T, TAUNTON JE, MACINTYRE D, et al. The effects of proprioceptive or strength training on the neuromuscular function of the ACL reconstructed knee: a randomized clinical trial. Scand J Med Sci Sports. 2003;13(2):115-123. [47] RISBERG MA, HOLM I. The long-term effect of 2 postoperative rehabilitation programs after anterior cruciate ligament reconstruction: a randomized controlled clinical trial with 2 years of follow-up. Am J Sports Med. 2009;37(10):1958-1966. [48] BAE CH, LEE JH, KIM JC, et al. Effects of resistance exercise using vibration stimulation on knee muscle strength and balance after anterior cruciate ligament Reconstruction. J Korean Acad Orthop Manual Phys Ther. 2017;23(2):17-25.
[49] BERSCHIN G, SOMMER B, BEHRENS A, et al. Whole body vibration exercise protocol versus a standard exercise protocol after ACL reconstruction: a clinical randomized controlled trial with short term follow-up. J Sports Sci Med. 2014;13(3):580-589. [50] COSTANTINO C, BERTULETTI S, ROMITI D. Efficacy of whole-body vibration board training on strength in athletes after anterior cruciate ligament reconstruction: a randomized controlled study. Clin J Sport Med. 2018;28(4):339-349. [51] FU CL, YUNG SH, LAW KY, et al. The effect of early whole-body vibration therapy on neuromuscular control after anterior cruciate ligament reconstruction: a randomized controlled trial. Am J Sports Med. 2013;41(4):804-814. [52] SALVARANI A, AGOSTI M, ZANRé A, et al. Mechanical vibration in the rehabilitation of patients with reconstructed anterior cruciate ligament. Europa medicophysica. 2003;39(1):19-25. [53] DOUGLAS J, PEARSON S, ROSS A, et al. Chronic adaptations to eccentric training: a systematic review. Sports Med. 2017;47(5):917-941. [54] CRENSHAW AG, KARLSSON S, STYF J, et al. Knee extension torque and intramuscular pressure of the vastus lateralis muscle during eccentric and concentric activities. Eur J Appl Physiol Occup Physiol. 1995; 70(1):13-19. [55] DOUGLAS MJ, HUTCHISON JD, SUTHERLAND AG. Anterior cruciate ligament integrity in osteoarthritis of the knee in patients undergoing total knee replacement. J Orthop Traumatol. 2010;11(3):149-154. [56] LEPLEY LK, LEPLEY AS, ONATE JA, et al. Eccentric exercise to enhance neuromuscular control. Sports Health. 2017;9(4):333-340. [57] LASTAYO PC, WOOLF JM, LEWEK MD, et al. Eccentric muscle contractions: their contribution to injury, prevention, rehabilitation, and sport. J Orthop Sports Phys Ther. 2003;33(10):557-571. [58] AMERICAN COLLEGE OF SPORTS MEDICINE. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41(3):687-708. [59] SCHOENFELD BJ. Does exercise-induced muscle damage play a role in skeletal muscle hypertrophy? J Strength Cond Res. 2012;26(5):1441-1453. [60] HORTOBáGYI T, DEVITA P, MONEY J, et al. Effects of standard and eccentric overload strength training in young women. Med Sci Sports Exerc. 2001;33(7):1206-1212. [61] GERBER JP, MARCUS RL, DIBBLE LE, et al. Effects of early progressive eccentric exercise on muscle structure after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2007;89(3):559-570. [62] GERBER JP, MARCUS RL, DIBBLE LE, et al. Safety, feasibility, and efficacy of negative work exercise via eccentric muscle activity following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2007;37(1):10-18. [63] FRIEDMANN-BETTE B, PROFIT F, GWECHENBERGER T, et al. Strength training effects on muscular regeneration after ACL reconstruction. Med Sci Sports Exerc. 2018;50(6):1152-1161. [64] FAXON JL, SANNI AA, MCCULLY KK. Hamstrings and quadriceps muscles function in subjects with prior ACL reconstruction surgery. J Funct Morphol Kinesiol. 2018;3(4):56-65. [65] LIU W, MAITLAND ME. The effect of hamstring muscle compensation for anterior laxity in the ACL-deficient knee during gait. J Biomech. 2000;33(7):871-879. [66] 陈鹏,王玲,董诗雨,等.全身振动训练对前交叉韧带重建后影响的Meta分析[J].中国组织工程研究,2023,27(36):5875-5883. [67] WERNBOM M, AUGUSTSSON J, THOMEé R. The influence of frequency, intensity, volume and mode of strength training on whole muscle cross-sectional area in humans. Sports Med. 2007;37(3):225-264. [68] LIM JM, CHO JJ, KIM TY, et al. Isokinetic knee strength and proprioception before and after anterior cruciate ligament reconstruction: a comparison between home-based and supervised rehabilitation. J Back Musculoskelet Rehabil. 2019;32(3):421-429. [69] LOUDER T, BRESSEL M, BRESSEL E. The kinetic specificity of plyometric training: verbal cues revisited. J Hum Kinet. 2015; 49(12):201-208. [70] BEHRENS M, MAU-MOELLER A, BRUHN S. Effect of plyometric training on neural and mechanical properties of the knee extensor muscles. Int J Sports Med. 2014;35(2):101-119. [71] SáEZ-SáEZ DE VILLARREAL E, REQUENA B, NEWTON RU. Does plyometric training improve strength performance? A meta-analysis. J Sci Med Sport. 2010;13(5):513-522. [72] RAMíREZ-CAMPILLO R, MEYLAN C, ALVAREZ C, et al. Effects of in-season low-volume high-intensity plyometric training on explosive actions and endurance of young soccer players. J Strength Cond Res. 2014;28(5):1335-1342. [73] VETTER S, SCHLEICHARDT A, KöHLER HP, et al. The effects of eccentric strength training on flexibility and strength in healthy samples and laboratory settings: a systematic review. Front Physiol. 2022;13(4):873370. [74] DAVIES G, RIEMANN BL, MANSKE R. Current concepts of plyometric exercise. Int J Sports Phys Ther. 2015;10(6):760-786. [75] LEPLEY LK, WOJTYS EM, PALMIERI-SMITH RM. Combination of eccentric exercise and neuromuscular electrical stimulation to improve quadriceps function post-ACL reconstruction. Knee. 2015;22(3):270-277. [76] MANDELBAUM BR, SILVERS HJ, WATANABE DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003-1010. [77] PEULTIER-CELLI L, MAINARD D, WEIN F, et al. Comparison of an innovative rehabilitation, combining reduced conventional rehabilitation with balneotherapy, and a conventional rehabilitation after anterior cruciate ligament reconstruction in athletes. Front Surg. 2017;4(11):61-70. [78] ARUMUGAM A, BJöRKLUND M, MIKKO S, et al. Effects of neuromuscular training on knee proprioception in individuals with anterior cruciate ligament injury: a systematic review and GRADE evidence synthesis. BMJ Open. 2021;11(5):e049226. [79] MANCA A, DRAGONE D, DVIR Z, et al. Cross-education of muscular strength following unilateral resistance training: a meta-analysis. Eur J Appl Physiol. 2017; 117(11):2335-2354. |
| [1] | Zhou Jian, Zhang Tao, Zhou Weili, Zhao Xingcheng, Wang Jun, Shen Jie, Qian Li, Lu Ming. Effects of resistance training on quadriceps mass and knee joint function in patients with osteoporosis and sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1081-1088. |
| [2] | Li Hanyue, Li Yini, Xiang Linmei, Li Sen. Effects of resistance exercise therapy on pain and function in patients with cervical spondylotic radiculopathy: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 987-996. |
| [3] | Sun Jiahe, Shi Jipeng, Zhu Tianrui, Quan Helong, Xu Hongqi. Effect of exercise intervention in elderly individuals with sarcopenia and its comorbidities: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 997-1007. |
| [4] | Sun Yundi, Cheng Lulu, Wan Haili, Chang Ying, Xiong Wenjuan, Xia Yuan. Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1945-1952. |
| [5] | Wang Yida, Liu Jun, Wang Xiaoling, Wang Liyan, Yang Chengru, Zhang Xuexiao. Effects of wearable electronic device-based interventions on physical activity and sedentary behavior in healthy adolescents: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1693-1704. |
| [6] | Zhang Zixian, Xu Youliang, Wu Shaokui, Wang Xiangying. Effects of blood flow restriction training combined with resistance training on muscle indicators in college athletes: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1705-1713. |
| [7] | Zheng Huakun, Yin Mingyue, Liu Qian. Effects of interval and continuous training on the quality of life in physically inactive adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1727-1740. |
| [8] | Wang Changbing, Zhao Lilian, Fu Chuying, Li Yanjin. Modified double-bundle arthroscopic repair of the anterior cruciate ligament after Sherman type I injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1192-1198. |
| [9] | Xiong Bohan, Wang Guoliang, Yu Yang, Xue Wenqiang, Yu Hong, Liu Jinrui, Ruan Zhaohui, Li Yajuan, Liu Haolong, Dong Kaiyan, Long Dan, Chen Zhao. Internal tension relieving technique assisted anterior cruciate ligament reconstruction to promote ligamentization of Achilles tendon grafts in small ear pigs in southern Yunnan province [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(4): 713-720. |
| [10] | Wang Feng, Cao Chunfeng, He Chao, Zhang Tao, Zhou Zixian, Zhu Fengchen. All-inside versus traditional techniques of anterior cruciate ligament reconstruction: meta-analysis of therapeutic efficacy and radiological outcomes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7629-7638. |
| [11] | Liu Mengling, Li Yongjie, Liu Hongju. Effect of increased stride length on knee kinematics and dynamics of asymmetric gait after anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7109-7115. |
| [12] | Wei Zhiheng, Guan Tianmin, Liu Qing, Gong Jue, Xiang Xianxiang. Application of 3D printing accurate osteotomy guide combined with the revision of anterior cruciate ligament with abnormally increased posterior slope of tibial plateau [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7130-7136. |
| [13] | Jiang Tao, Zhang Chuankai, Hao Liang, Liu Yong. MAKO robot- and navigation-assisted knee replacement: comparison of lower limb force alignment and prosthesis position accuracy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7150-7157. |
| [14] | Liu Liguo, Qiu Mingwang, Huang Yanling, Fan Zhiyong, Wu Shan, Guo Rusong. Reporting quality of randomized controlled trials on acupuncture and manipulation for greater occipital neuralgia evaluated using the CONSORT statement and STRICTA checklist [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6566-6573. |
| [15] | Jiang Siqi, Huang Huanhuan, Yu Xinyu, Peng Ying, Zhou Wei, Zhao Qinghua. Meta-analysis of dose-effect of exercise on improving muscle health in community-dwelling older adults with sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6295-6304. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||