Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (27): 4421-4428.doi: 10.12307/2024.577
Proprioceptive training after anterior cruciate ligament reconstruction: improving joint stability and motor balance ability
Ye Yuntian1, 2, Chen Jixin1, 2, Liu Aifeng1, 2
- 1Department of Orthopedics, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin 300381, China; 2National Clinical Research Center for Traditional Chinese Medicine and Acupuncture, Tianjin 300381, China
-
Received:2023-10-28Accepted:2023-12-14Online:2024-09-28Published:2024-01-29 -
Contact:Liu Aifeng, Doctoral supervisor, Chief physician, Department of Orthopedics, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin 300381, China; National Clinical Research Center for Traditional Chinese Medicine and Acupuncture, Tianjin 300381, China -
About author:Ye Yuntian, Master candidate, Department of Orthopedics, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin 300381, China; National Clinical Research Center for Traditional Chinese Medicine and Acupuncture, Tianjin 300381, China -
Supported by:National Natural Science Foundation of China, No. 81873316 (to LAF); Interdisciplinary Research Project on Prevention and Treatment of Orthopedic Diseases of Chinese Society of Traditional Chinese Medicine, No. 2023-GBJC-04 (to LAF); Jinmen Medical Excellence Project of Tianjin Municipal Health Commission, No. TJSJMYXYC-D2-028 (to LAF)
CLC Number:
Cite this article
Ye Yuntian, Chen Jixin, Liu Aifeng. Proprioceptive training after anterior cruciate ligament reconstruction: improving joint stability and motor balance ability[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(27): 4421-4428.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
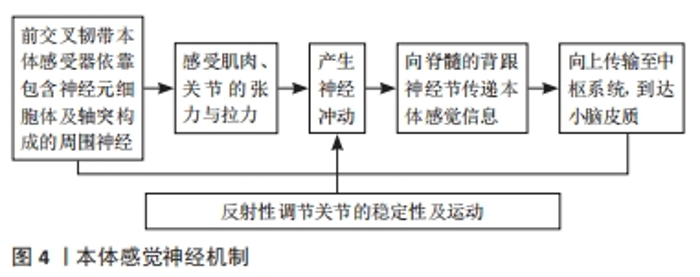
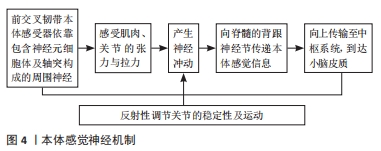
2.1 前交叉韧带本体感觉损伤的机制 本体感觉被定义为有意识地感知位置、运动以及施加在身体各部分上和产生的力的能力,即可以感知躯体对速度、距离和空间位置等感觉, 它在关节稳定、姿势和运动控制方面起着至关重要的作用。 2.1.1 前交叉韧带中的机械感受器 膝关节本体感觉主要源于关节内的机械感受器。1984年,SCHULTZ等[27]首次对人类十字韧带中的感受器进行了组织学证明。FREEMAN等[28]将膝关节中的感受器进行了分类:Ⅰ类为Ruffini小体,Ⅱ类为Pacinian小体,Ⅲ类为Golgi样腱器官,Ⅳ类为游离神经末梢(free nerve ending)。不同的感受器对人体也有着各自的作用。关节伸展、屈曲和旋转引起的扭矩可以刺激Ruffini小体,从而感受静止的膝关节位置。Pacinian小体对关节位置的变化非常敏感,能产生和传递关节运动感觉,在关节动态运动中起重要作用。Golgi腱器官在防止关节极度屈伸和旋转方面起着重要作用。游离神经末梢主要参与疼痛和关节炎症的感知[29-30]。机械感受器大多位于前交叉韧带的远端,靠近胫骨附丽处[31]。 2.1.2 前交叉韧带中的本体感受器作用机制 本体感觉是一种感觉方式,可以帮助人们清楚地察觉身体各部位所处的位置、方向及状态,这其中就包括关节位置和关节运动觉,这将有助于膝关节在生活及运动中的稳定性。膝关节的本体感觉同时是一个复杂的系统,它涉及关节囊中的机械感受器、韧带、视觉、触觉以及连接到脊髓和大脑皮质的神经组织[32]。人类对位置觉及平衡功能等信息来源由中枢神经系统、机械感受器、前庭感受器和视觉感受器共同构成。其中前交叉韧带内包含大量的机械感受器[29],并且与脊髓、脑干和小脑有直接的神经联系[33],感觉通过脊髓后束传递到中枢神经系统,最终到达大脑,大脑内多感觉区进行刺激信息处理后将其整合成运动模式和意识感知并再次传输回躯干及四肢[34]。即人体通过动觉信号及视觉信号而实时做出运动反应,并将此作为传出信号输送至运动系统,再通过“拷贝传出信号”告知中枢系统,以此保证肢体运动的准确性[35],见图4。 "
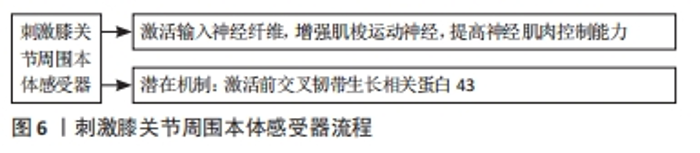
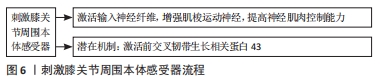
?ABUK等[36]发现,前交叉韧带损伤后的机械感受器数量与健康组相比在数量上有着显著下降,其中Ruffini末梢便会随着时间推移而减少。由于Ruffini末梢可以帮助感觉关节位置[29],所以这种类型的机械感受器的数量减少或许可以解释前交叉韧带损伤后的患者会出现关节错位及僵硬等情况。ADACHI等[37]发现,在其研究的29个前交叉韧带残留物中,平均每个标本存在18个机械感受器,并且机械感受器的数量与关节位置感的准确性呈正相关。 前交叉韧带断裂后,上行传入神经通路中断,脑结构也随之发生改变,KAPRELI等[38]发现,中枢神经系统发生改变引发了脑部运动感觉区的激活减小。小脑脚1区域可以将运动信息从大脑传输至四肢,终而起到维持平衡、协调的作用,前交叉韧带断裂后,同侧的小脑脚1区激活下降,上行传导至大脑皮质的激活同时减少。有研究发现,前交叉韧带损伤后,即便接受了前交叉韧带重建术,大脑神经激活模式也可能被永久改变[39]。苗欣等[40]发现,前交叉韧带断裂的患者当其患侧肢运动时,脑电功率显著提高,这提示相较健侧肢,患侧将调用更多脑资源。顶叶的体感皮质和枕叶的视觉皮质被赋予将传入的感觉信息整合到感觉运动系统的重要作用[41]。KAPRELI等[38]发现,前交叉韧带断裂患者的脑区颞下回区域激活程度更高,其位于视觉皮质,这可能说明他们在运动过程中对视觉反馈的需求增加源于患者的本体感受信息受限。AN等[42]发现,中心前额叶皮质的α-2神经功率变大,说明前额叶皮质的认知处理受到限制;并且前交叉韧带重建术组在中央体感皮质的α-2神经功率下降较多,神经活动减少,可能表明前交叉韧带重建术组更依赖于负责处理来自下肢的感觉输入的体感皮质的皮质激活,而健康组的初级视觉皮质的α-2功率显示较多,说明其更依赖于内部认知处理进而维持平衡。 2.2 本体感觉训练在前交叉韧带重建术后康复机制 2.2.1 刺激膝关节周围本体感受器 本体感觉训练可通过关节运动或肌肉收缩等干预手段激活膝关节周围组织的神经肌肉反馈,以此来重建正确的运动模式。其中平衡训练促进神经肌肉机制,激活了动肌和拮抗肌的共同收缩,从而增强关节稳定性,最终减少关节位移,达到恢复关节功能的目的[43]。平衡训练或其结合某种技术,可通过在训练过程中增加扰乱平衡的因素,提高患膝的平衡能力。如:训练中通过改变速度、站立环境等因素增强其反应能力[23,44],使患者不断的自我纠正失衡状态,刺激其膝关节周围本体感受器,增强其运动觉和位置觉能力,提高了患者身体控制能力、关节控制能力、关节稳定性并缩短膝关节的信号反馈时间,达到激活输入神经纤维、增强肌梭运动神经、提高神经肌肉控制能力的目的,最终改善膝关节本体感觉能力,重建正确运动模式。前交叉韧带的生长相关蛋白43(growth associated protein-43,GAP-43) 是存在于神经系统中的特异性磷蛋白,其对神经的生长、发育和再生有重要影响,是神经修复和再生的标志物之一[45-46]。DUSART等[47]发现,GAP-43是成年期发育和轴突再生过程中最密切的蛋白质,中枢神经系统轴突受损后也可重新表达。前交叉韧带损伤后通常引起周围神经受损,使得相关蛋白表达变化。由于GAP-43在正常神经元中低表达,在受损神经元中则表达上调[48],可能潜在对前交叉韧带本体感受器活性恢复具有一定积极作用。故患者在进行平衡训练时,其运动状态或许可以通过关节内组织刺激本体感受器以及游离神经末梢产生一定的神经冲动,激活GAP-43活性,使该蛋白在前交叉韧带本体感受器内聚合能力升高,进而增强本体感受器活性,提高本体感觉功能,见图6。"
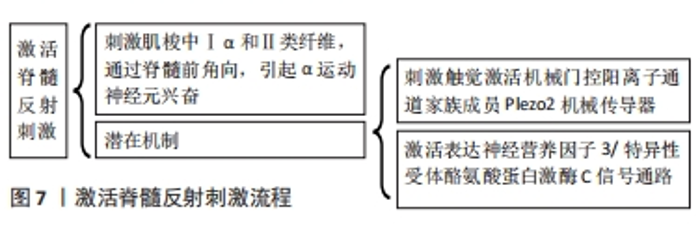
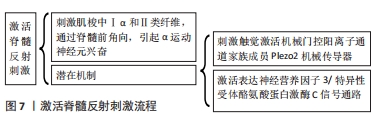
2.2.2 激活脊髓反射刺激 本体感受器通过脊髓后束传输至中枢神经。人类除头面部之外的机械感觉都源于背根神经节的传入神经元,并发出两个主要分支,一支投至外周组织,另一支则投至中枢脊髓部分[49]。本体感觉和触觉会传入共享体感皮质中的重叠网络,振动训练和水疗法便是通过触觉刺激增强本体感觉[50]。Piezo2具备触觉的机械传导功能,RANADE等[51]发现,缺乏Piezo2的小鼠几乎完全丧失了触觉。振动训练引起人体神经肌肉反应,它通过传入神经纤维刺激肌梭,导致高阈值运动单位通过单突触和多突触途径招募[52]。细胞膜联蛋白A2和脯氨酰4-羟化酶参与胶原的合成、组装、交联和重塑,振动刺激可以增加细胞外基质的含量,改变细胞环境,从而促进细胞生长,并产生用于细胞收缩的三磷酸腺苷。全身振动刺激可以提高细胞膜联蛋白A2和脯氨酰4-羟化酶的表达量,帮助前交叉韧带修复[53]。水疗法利用水中阻力,和静水压产生触觉刺激。水中的黏性阻力与静水压是外部感觉刺激的来源,患者在水中运动时,由于移动时身体受到的阻力和在水中控制身体平衡等动作,增加了患者对四肢位置感知,最终促进本体感觉恢复[33]。其另外潜在机制可能是通过外在设备及环境影响了患肢的触觉,刺激本体感觉信号通路,增强了Piezo2表达。 肌肉力量与膝关节稳定性和运动觉有着显著关系[52,54]。谷莉等[55]发现,前交叉韧带重建术后,股四头肌力量与本体感觉恢复呈正相关,暗示肌力训练和本体感觉训练可能互有益处。神经肌肉训练和血流限制训练均可改善肌肉质量,强化肌肉力量。血流限制训练过程中,乳酸和氢离子积累增加,pH值降低,刺激了传入纤维,比没有参与血流限制训练的患者更早导致神经肌肉疲劳,疲劳程度的增加可能在训练中较早地招募阈值较高的运动单位,使更大比例的肌肉纤维产生肥大刺激[56]。肌梭自身也是一类感受器,其中的Ⅰa和Ⅱ类纤维向脊髓传入信息,但二者的反应特征有所不同,前者主要向中枢神经系统输送动态运动引起的肌纤维变化信息,后者为直径较细的Ⅱ类纤维,主要对静态的牵拉刺激敏感性较强[57-58]。中枢神经在慢速运动时对Ⅰα肌梭和关节感受器的外周信号进行了适应,而在快速运动时对Ⅱ型肌梭或动态肌梭进行了适应[59]。肌梭传入会与α运动神经形成突触联系,传入冲动是脊髓前角α运动神经元兴奋的基础[58]。神经肌肉、血流限制和振动训练等刺激了肌梭,并激活作用于α神经元的紧张性振动反射。最终使中枢运动指令开始运作,促进自主运动能力,改善本体感觉[60]。 表达神经营养因子3(neurotrophin-3,NT-3)可以为本体感觉神经元提供其必需的神经营养因子。位于脊髓的背根神经节中的本体感觉神经元,表达NT-3和特异性受体酪氨酸蛋白激酶(tyrosine protein kinase,Trk)C,提示NT-3的局部表达对于本体感觉有着重要作用[61-63]。TrkC是NT-3的高亲和力受体,二者结合可为正常神经元发育及受损神经元修复[64]。已经有研究发现,通过干预NT-3/TrkC信号通路,使TrkC磷酸化,促进局部的GAP-43活性上升,有效改善了本体感觉功能[65-66]。Piezo2是与机械敏感电位相关的蛋白质,在背根神经节的感觉神经元和Merkel细胞的皮肤机械感受器均有表达,是目前认识最充分的哺乳动物本体感觉受体[51,67-68]。WOO等[69]发现,本体感觉神经元中敲除Piezo2的哺乳动物会出现严重不协调和肢体位置异常等表现,表明Piezo2是哺乳动物的主要机械转导器。包括神经肌肉训练等本体感觉训练,在训练中通过刺激关节周围肌梭及神经纤维,或许可以激活NT-3/TrkC信号通路和Piezo2机械传导器,最终改善本体感觉功能,是未来的潜在机制之一,见图7。"
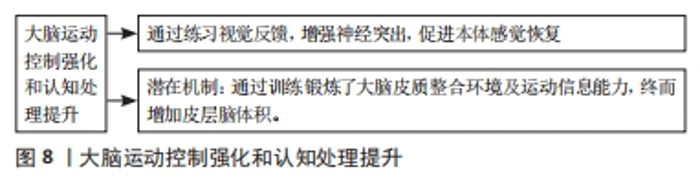
2.2.3 大脑运动控制强化和认知处理提升 本体感觉神经元通过投射至脊髓小脑束的中间神经元,将信号上传至小脑[70]。综合动觉和视觉分别感受到的身体信号及环境信号,动态制定出运动计划然后传输至运动系统。后顶叶皮质是接收并处理本体感觉、视觉等多种信号的联合区之一,将其汇总后,传送至运动脑区[38]。前交叉韧带断裂后,与视觉认知的楔前叶活动增加,导致感觉处理过程重新加权,使其转向顶叶-视觉处理区域。楔前叶的任务增加可能表明,大脑对感觉信号的处理效率降低,由于后顶叶皮质和楔前叶可以提供代偿途径,增强了对视觉认知的依赖以帮助人体维持稳定性[71]。患者前交叉韧带受伤后可能出现视觉-运动控制的改变[72]。 前交叉韧带重建术后,患者会更多地通过视觉感知来补偿受损的平衡控制[73]。接受前交叉韧带重建术的患者在静态姿势稳定性和控制能力方面存在缺陷,如增加身体的摇摆[74]。MIKO等[75]发现患者在前交叉韧带重建术后,较于睁眼而言,闭眼条件下会出现更大的静态姿势不稳定性。位置觉是属于本体感觉的一种特殊感觉形式,其与视觉、前庭系统的神经输入同时被处理,根据特定环境中的不同运动任务稳定身体姿势[73]。此外,患者通过视觉反馈训练,加强了关节向中枢输送本体感觉信号的能力,以此促进本体感觉能力[76]。视觉反馈训练可以增强神经突触,进而改善脑结构可塑性,最终更好地恢复本体感受器与脑之间的信号传输[77]。 随着患者不断接收视觉反馈结合本体感觉训练,增强膝关节本体感受器传输信号能力,使得大脑皮质整合环境、感觉及运动信息能力不断提高,动作逐渐从简单转向复杂,重新恢复对自身躯体动作和周围环境的认知,最终改善感知、控制动作的皮质脑体积,增强了患者姿势控制能力,是该部分的潜在机制,见图8。"

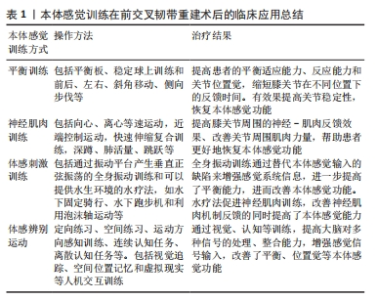
2.3.1 平衡训练 平衡训练包括动态平衡训练和静态平衡训练[79],如平衡板、稳定球上训练和前后、左右、斜角移动、侧向步伐等,通过在训练过程中循序渐进的增加不稳定性,提高患者的平衡适应能力,提升患者的关节位置觉,最终提升了运动中的反应能力[80]。 平衡训练或将其结合各类科技手段,通过增强患者身体控制能力以到达改善本体感觉功能的目的。刘国龙[79]对190例前交叉韧带重建患者进行随机对照试验发现,平衡促进训练相较于常规康复训练对本体感觉功能恢复具有更好的效果。BALTACI等[81]发现,任天堂Wii Fit平衡板设备通过增强患者及时反馈能力,改善了前交叉韧带重建患者的本体感觉。汪杰等[44]发现,使用危机模拟应激跑台训练系统,向大脑皮质传入各种本体觉、前庭觉刺激等动态反馈,可以有效改善前交叉韧带重建术后患者患膝本体感觉,降低跌倒风险。施明等[23]发现,虚拟现实平衡训练通过训练患者在不稳定平面下进行运动控制,能有效改善前交叉韧带重建术后膝关节本体感觉障碍,缩短膝关节在不同位置下的反馈时间。 2.3.2 神经肌肉训练 神经肌肉训练通过改善膝关节周围的神经-肌肉反馈机制,对前交叉韧带重建术后提高关节稳定性、防止二次损伤具有重要意义。神经肌肉训练中,肌肉力量训练是其重要步骤,通过不同训练方法帮助重塑或增强膝关节周围肌肉力量,最终达到改善本体感觉神经-肌肉控制能力[82-83]。 GHADERI等[22]发现,通过包含深蹲、肺活量、跳跃及在不稳定的表面上单腿站立等训练项目的神经肌肉训练,有效改善了患者的本体感觉。GHADERI等[59]的另一篇文章发现,神经肌肉训练结合外部焦点训练对关节位置感错误的改善达到了51%,可以增强患者本体感觉功能。KAYA等[84]发现,对于同种异体胫骨前肌移植的患者,神经肌肉训练方案可以增强其本体感觉功能。并且发现神经肌肉训练组患者在膝关节屈曲15°,45°和75°时的关节位置感要优于标准康复组的患者。但BULOW等[85]发现,基于扰动的神经肌肉训练,对于前交叉韧带损伤后的青春期女性在本体感觉方面没有改善。其原因可能有:①该训练方法是为成年人设计,却应用于青少年患者;②患者尚处于青春期,身体处于动态发育过程,可能会影响到训练结果;③女性生理结构不同,某种特定的训练方法可能对其无效;④女性肌肉质量相对较差,或许应该先专注进行单项神经肌肉训练,以恢复肌力为主,训练中后期再加入扰动训练。 2.3.3 体感刺激训练 该训练法借助带有负责传递触觉刺激的器械、设备或环境,促进本体感觉的发展和恢复,以体感形式的刺激为主,如通过水环境训练的水疗法、利用对应仪器产生的简谐振动促使肌肉振动或全身振动训练、局部振动[86-87]。在恢复本体感觉功能之外,水疗法通过让患者尝试在水中锻炼,利用水环境刺激皮肤的感觉神经末梢并且由于感觉溢出升高了疼痛阈值,帮助患者更好地缓解疼痛,改善肿胀[26]。 水疗法是指在康复过程中为达到治疗目的而利用水环境及其特点的所有活动[78],其主要优势为,在功能恢复过程中可以更早地引入活动或锻炼,从而有可能加速恢复过程并缩短总体恢复时间[88]。与此同时,该疗法还可以有效改善前交叉韧带重建术后患者的本体感觉能力。HAJOUJ等[25]发现,经过特别设计的水疗法可以促进本体感觉康复效率。SO等[89]发现,在水中使用跑步机可以促进神经肌肉控制恢复。PEULTIER-CELLI等[90]发现,遵循了加入水疗法的创新康复方案的患者术后膝关节屈曲本体感觉障碍显著减少,本体感觉能力增强。 全身振动训练通过诱导受试者反射性肌肉收缩,以达到引起自主肌肉收缩的目的。MOEZY等[19]发现,全身振动训练可以提高关节测试角度,通过增强关节活动改善患者本体感觉。FU等[91]却发现,全身振动训练对关节位置感没有改善,但在术后3个月对本体感觉功能有积极作用。这种差异可能源于训练时间的长短,FU等[91]只进行了为期3个月的综合训练,而MOEZY等[19]则是进行了4个月综合训练且每周进行3次全身振动。膝关节本体感觉缺失会导致关节运动失去控制。PISTONE等[92]发现,全身振动训练对前交叉韧带重建患者的平衡能力相较于传统训练方法没有明显改善。这与FU等[91]和MOEZY等[19]的研究具有差异性,其原因可能与测量平衡能力的设备与方法相关,由于PISTONE等[92]仅要求患者站在压力板上进行测试,故其测量手段的静态数据可能相对不够准确。 力量对于本体感觉的恢复至关重要[93]。高强度牵拉股四头肌可以激活Ruffini末梢和Golgi感受器,促进了本体感觉功能恢复[94]。ERICKSON等[95]发现,血流限制训练可以有效改善前交叉韧带重建术后患者股四头肌肌力。HUGHES等[96]发现,血流限制训练对受伤肢体的肌肉力量提高了85%并且可以减少疼痛和积液。JACK等[97]发现,血流限制训练可减少前交叉韧带重建术后患者在12周内的肌肉流失。 2.3.4 体感辨别训练 视觉反馈或视听反馈等外部焦点注意力训练通过虚拟现实、危机跑台等设备引导的定向练习、空间练习和运动方向感知训练和连续认知任务、离散认知任务等,它们通过连续性或间歇性地将注意力从姿势控制上转移来帮助个体重新建立自身位置觉和运动方向的感知能力[98]。虚拟现实等带有游戏性质的训练方法,增加了患者训练时的趣味性,可以更好地提高患者注意力,更顺利地引导其进行训练。 MOLKA等[73]发现,基于生物反馈的康复治疗可以改善前交叉韧带损伤患者静态和动态平衡。黄礼群等[77]发现,平衡训练结合视觉反馈训练可有效改善前交叉韧带重建术后患者的本体感觉功能。施明等[23]利用VR虚拟现实技术在视觉反馈的基础上增加了听觉反馈训练,形成视觉、听觉、本体感觉和前庭觉的综合反馈,有效改善本体感觉功能。AHMADI等[99]发现,连续认知任务要比单纯的外部视觉焦点训练更能稳定前交叉韧带损伤患者的姿势稳定性。外部焦点训练是前交叉韧带重建术后康复的重要补充。GHADERI等[59]发现,神经肌肉训练结合外部焦点训练可以有效改善关节位置感,并帮助患者减少着陆时对前交叉韧带的负荷。 前交叉韧带损伤后,本体感觉功能减退,进而平衡功能下降。同时,前交叉韧带重建术后患者在闭眼条件下有着更差的稳定性。MOLKA等[73]认为,这种情况可能是由于前交叉韧带重建术后患者在平衡功能受损后,视觉系统参与代偿,故闭眼后代偿因素排除,平衡受损表现更明显,这提示锻炼视觉系统可能可以帮助患者更好地恢复平衡功能。故在本体感觉训练中,应加强视觉或视听反馈训练,使患者接收不同感官信号,增强感觉信号输入[23,100]。但也有观点认为,患者在增加视觉反馈训练后,由于过多地关注外部信息而忽略自身的本体感觉信号,可能导致平衡训练效果不佳[100]。提示应该考虑在不同阶段进行分别不同的训练模式,打好基础再进入下一环节。 2.3.5 本体感觉训练在前交叉韧带重建术后的分期论治 虽然有大量的研究证明本体感觉训练可以改善前交叉韧带重建患者的本体感觉功能,但单一的训练方式不能体现其在整体康复计划中的应用,故了解不同康复阶段该如何进行本体感觉训练将有利于临床指导。 (1)术后前期选择:水疗法应用于前交叉韧带重建术后患者在初期阶段进行康复锻炼效果最佳[88]。因为当水压高于舒张压时有利于静脉回流和淋巴系统回流,可以帮助消退炎症、减轻肿胀,并积极增加关节的活动范围。水同时还起着平衡重力的作用,由于水的浮力抵消了重力,这意味着与常规地面锻炼相比,在水中可以更早地引入功能性或运动练习,并通过调节水的深浅,以达到循序渐进的锻炼目的,如早期可以在水中由深至浅的进行步行锻炼。当患者进入到中后期康复阶段时,水疗法仍可利用自身特点起到积极作用,如水中跑步机训练或诸如泡沫轴等的一些特定训练,可明确改善患者本体感觉功能。 水疗法通常在前交叉韧带重建术后2周开始进行,需注意水的深度、水流大小等因素。LI等[26]通过水基跑步机训练发现,水中训练时由于从前到后的水流提供了更高的阻力,故伸肌锻炼效果更好,屈肌效果较差。HAJOUJ等[25]通过诸如踩泡沫轴等水中训练方式发现,患者稳定性提高,并且由于流体静力效应刺激皮肤中的感觉神经末梢,使疼痛感降低。水的深度也是影响康复计划因素的一部分,初期在大约120 cm的深度进行康复训练,此时静水压略高于舒张压,除了恢复本体感觉功能以外,还可达到改善关节肿胀及被动、主动活动范围的目的[82]。SO等[89]发现通过水上跑步机,站立阶段的股二头肌肌肉活动会随着水深的增加而增加。LI等[26]研究,患者在进行水疗法训练时,水深应位于剑突位置。数据表明水深达到人体在剑突处时体质量减轻60%,耻骨联合减轻40%;脐部则是50%,与此同时水的深度变化所带来的阻力变化和水流变化也会影响患者的动作质量,从而影响恢复效果。 血流限制训练同样适合前交叉韧带重建术早期本体感觉康复训练,它为临床医生提供了一种可以在患者尚且无法达到一定运动量和负荷情况下的安全有效的训练方法,度过早期阶段后,其也可以与有氧运动相结合,灵活地应用于热身、运动与放松之间。其通过缺血、压力两种因素改变了疼痛敏感性并且运动期间可能释放内源性阿片类药物和内源性大麻素,起到了减轻疼痛的效果[96,101]。虽然血流限制训练目前表明其可以直接改善本体感觉功能的证据较少,但在增强股四头肌力量和激活肌肉的过程中,可能会刺激关节周围的本体感受器或Piezo2机械传感器等潜在机制,间接为本体感觉恢复提供帮助。 (2)中后期选择:MA等[93]发现,力量训练是帮助患者重返运动中最重要的环节,而触觉是相对效果最差的。故在中后期阶段,水疗法等依靠环境刺激触觉的方法,应减少应用,改为辅助配合,开始更加注重本体感觉训练中神经肌肉训练和单独力量训练以及视觉反馈等认知训练对运动功能的恢复。施明等[23]在患者术后第8周引入虚拟现实技术进行本体感觉训练,通过虚拟现实下不同的虚拟游戏迫使患者努力保持关节平衡,刺激本体感觉通路,恢复本体感觉功能。汪杰等[44]在患者接受常规康复后,达到膝周肌群肌力4级以上以及膝关节主动活动度正常时引入危机模拟应激跑台,通过速度和平衡干扰,帮助患者更好地恢复本体感觉功能。MIKO等[75]在前交叉韧带重建患者术后至少6个月以后,引用双重运动及双重认知训练方法,除了可以提高患者姿势稳定性以外还发现采用双重认知训练方法可帮助运动员获得更大的灵活性并对控球类球员帮助更大。张晓辉等[102]发现,在康复计划早期进行神经肌肉训练可能会增加关节肿胀的症状,术后3-6个月进行神经肌肉训练结合力量训练在肌力和耐力等方面效果较为理想。"

| [1] SHAW G, SERPELL B, BAAR K. Rehabilitation and nutrition protocols for optimising return to play from traditional ACL reconstruction in elite rugby union players: A case study. J Sports Sci. 2019;37(15):1794-1803. [2] DAUTY M, MENU P, MESLAND O, et al. Arthrogenic muscle inhibition and return to sport after arthrofibrosis complicating anterior cruciate ligament surgery. Eur J Sport Sci. 2022;22(4):627-635. [3] KAEDING CC, LÉGER-ST-JEAN B, MAGNUSSEN RA. Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med. 2017;36(1): 1-8. [4] JAMESON SS, DOWEN D, JAMES P, et al. Complications following anterior cruciate ligament reconstruction in the English NHS. Knee. 2012;19(1):14-19. [5] 陈连旭, 付立功. 前交叉韧带断裂和重建的临床流行病学分析[J]. 中国组织工程研究,2016,20(24):3602-3608. [6] 李露祎, 厉晓杰, 黑泽明, 等. 移植物类型对前交叉韧带重建后患者膝关节功能的影响[J]. 中国组织工程研究,2024,28(17):2753-2758. [7] DEHNE E, COLONEL L. The spinal adaptation syndrome (a theory based on the study of sprains). Clin Orthop Relat Res. 1955;5:211-220. [8] CURL WW, MARKEY KL, MITCHELL WA. Agility training following anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 1983;172:133-136. [9] IWASA J, OCHI M, ADACHI N, et al. Proprioceptive improvement in knees with anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2000; (381):168-176. [10] HOFFMAN M, SCHRADER J, KOCEJA D. An investigation of postural control in postoperative anterior cruciate ligament reconstruction patients. J Athl Train. 1999;34(2):130-136. [11] JEROSCH J, SCHÄFFER C, PRYMKA M. Propriozeptive Fähigkeiten bei operativ und konservativ behandelten kreuzbandinsuffizienten Kniegelenken [Proprioceptive abilities of surgically and conservatively treated knee joints with injuries of the cruciate ligament]. Unfallchirurg. 1998;101(1):26-31. [12] JEROSCH J, PFAFF G, THORWESTEN L, et al. Auswirkungen eines propriozeptiven Trainingsprogramms auf die sensomotorischen Fähigkeiten der unteren Extremität bei Patienten mit einer vorderen Kreuzbandinstabilität [Effects of a proprioceptive training program on sensorimotor capacities of the lower extremity in patients with anterior cruciate ligament instability]. Sportverletz Sportschaden. 1998;12(4):121-130. [13] WU GK, NG GY, MAK AF. Effects of knee bracing on the sensorimotor function of subjects with anterior cruciate ligament reconstruction. Am J Sports Med. 2001;29(5):641-645. [14] ZHOU MW, GU L, CHEN YP, et al. Factors affecting proprioceptive recovery after anterior cruciate ligament reconstruction. Chin Med J (Engl). 2008; 121(22): 2224-2228. [15] REIDER B, ARCAND MA, DIEHL LH, et al. Proprioception of the knee before and after anterior cruciate ligament reconstruction. Arthroscopy. 2003;19(1):2-12. [16] KARASEL S, AKPINAR B, GÜLBAHAR S, et al. Clinical and functional outcomes and proprioception after a modified accelerated rehabilitation program following anterior cruciate ligament reconstruction with patellar tendon autograft. Acta Orthop Traumatol Turc. 2010;44(3):220-228. [17] HOPPER DM, CREAGH MJ, FORMBY PA, et al. Functional measurement of knee joint position sense after anterior cruciate ligament reconstruction. Arch Phys Med Rehabil. 2003;84(6):868-872. [18] BRUNETTI O, FILIPPI GM, LORENZINI M, et al. Improvement of posture stability by vibratory stimulation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1180-1187. [19] MOEZY A, OLYAEI G, HADIAN M, et al. A comparative study of whole body vibration training and conventional training on knee proprioception and postural stability after anterior cruciate ligament reconstruction. Br J Sports Med. 2008;42(5): 373-378. [20] ZHEN D, QIU B, WANG W, et al. Proprioceptive changes measured by histopathological and electrophysiological evaluations after NGF injection of anterior cruciate ligament reconstruction. Ann Palliat Med. 2020;9(1):37-44. [21] FEIL S, NEWELL J, MINOGUE C, et al. The effectiveness of supplementing a standard rehabilitation program with superimposed neuromuscular electrical stimulation after anterior cruciate ligament reconstruction: a prospective, randomized, single-blind study. Am J Sports Med. 2011;39(6): 1238-1247. [22] GHADERI M, LETAFATKAR A, ALMONROEDER TG, et al. Neuromuscular training improves knee proprioception in athletes with a history of anterior cruciate ligament reconstruction: A randomized controlled trial. Clin Biomech (Bristol, Avon). 2020;80:105157. [23] 施明, 潘文平, 曾明, 等. 虚拟现实平衡训练对前交叉韧带重建术后膝关节本体感觉的效果[J]. 中国康复理论与实践,2020,26(12):1458-1463. [24] GSANGAYA MR, HTWE O, SELVI NAICKER A, et al. Comparison between the effect of immersive virtual reality training versus conventional rehabilitation on limb loading and functional outcomes in patients after anterior cruciate ligament reconstruction: A prospective randomized controlled trial. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2023;34:28-37. [25] HAJOUJ E, HADIAN MR, MIR SM, et al. Effects of Innovative Aquatic Proprioceptive Training on Knee Proprioception in Athletes with Anterior Cruciate Ligament Reconstruction: A Randomized Controlled Trial. Arch Bone Jt Surg. 2021;9(5):519-526. [26] LI D, ZHANG Q, LIU X, et al. Effect of water-based walking exercise on rehabilitation of patients following ACL reconstruction: a prospective, randomised, single-blind clinical trial. Physiotherapy. 2022;115:18-26. [27] SCHULTZ RA, MILLER DC, KERR CS, et al. Mechanoreceptors in human cruciate ligaments. A histological study. JBJS. 1984;66(7):1072-1076. [28] FREEMAN MAR, WYKE B. Articular contributions to limb muscle reflexes. The effects of partial neurectomy of the knee‐joint on postural reflexes. Br J Surg. 1966;53(1):61-69. [29] BANIOS K, RAOULIS V, FYLLOS A, et al. Anterior and posterior cruciate ligaments mechanoreceptors: a review of basic science. Diagnostics. 2022; 12(2):331. [30] MOON KM, KIM J, SEONG Y, et al. Proprioception, the regulator of motor function. BMB Rep. 2021;54(8):393. [31] LEE BI, KIM CH, JANG BW, et al. Preservation of the tibial remnant in anterior cruciate ligament reconstruction may improve postoperative proprioceptive function. Orthopedics. 2020;43(4):e231-e236. [32] SHEN M, CHE S, YE D, et al. Effects of backward walking on knee proprioception after ACL reconstruction. Physiother Theory Pract. 2021;37(10):1109-1116. [33] KAPRELI E, ATHANASOPOULOS S. The anterior cruciate ligament deficiency as a model of brain plasticity. Med Hypotheses. 2006;7(3):645-650. [34] JAHN K, KREWER C. Propriozeption–Der, sechste Sinn “und seine Störungen. Dtsch Med Wochenschr. 2020;145(25):1855-1860. [35] POULET JFA, HEDWIG B. New insights into corollary discharges mediated by identified neural pathways. Trends Neurosci. 2007;30(1):14-21. [36] ÇABUK H, KUŞKU ÇABUK F, TURAN K. The time from injury to surgery is an important factor affecting the mechanoreceptors at stump of torn anterior cruciate ligament. Arch Orthop Trauma Surg. 2022;142(11):3389-3393. [37] ADACHI N, OCHI M, UCHIO Y, et al. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. 2002;73(3):330-334. [38] KAPRELI E, ATHANASOPOULOS S, GLIATIS J, et al. Anterior cruciate ligament deficiency causes brain plasticity: a functional MRI study. Am J Sports Med. 2009;37(12):2419-2426. [39] AN YW, DITRANI LOBACZ A, LEHMANN T, et al. Neuroplastic changes in anterior cruciate ligament reconstruction patients from neuromechanical decoupling. Scand J Med Sci Sports. 2019;29(2):251-258. [40] 苗欣, 黄红拾, 胡晓青, 等. 膝关节前交叉韧带断裂后单腿位置觉测试时脑电功率谱的变化特征[J]. 北京大学学报(医学版),2021,53(5): 871-876. [41] STRONG A, GRIP H, BORAXBEKK CJ, et al. Brain Response to a knee proprioception task among persons with anterior cruciate ligament reconstruction and controls. Front Hum Neurosci. 2022;16:841874. [42] AN YW, KANG Y, JUN HP, et al. Anterior cruciate ligament reconstructed patients who recovered normal postural control have dissimilar brain activation patterns compared to healthy controls. Biology. 2022;11(1):119. [43] HRYSOMALLIS C. Relationship between balance ability, training and sports injury risk. Sports Med. 2007;37:547-556. [44] 汪杰, 苏建康, 张玉婷, 等. 危机模拟应激跑台训练系统影响膝关节前交叉韧带断裂重建术后患膝本体感觉的研究[J]. 中国康复医学杂志, 2022,37(4):534-536. [45] FORSOVA OS, ZAKHAROV VV. High‐order oligomers of intrinsically disordered brain proteins BASP1 and GAP‐43 preserve the structural disorder. FEBS J. 2016;283(8):1550-1569. [46] CHEN MM, YIN ZQ, ZHANG LY, et al. Quercetin promotes neurite growth through enhancing intracellular cAMP level and GAP-43 expression. Chin J Nat Med. 2015;13(9):667-672. [47] DUSART I, GHOUMARI A, WEHRLE R, et al. Cell death and axon regeneration of Purkinje cells after axotomy: challenges of classical hypotheses of axon regeneration. Brain Res Brain Res Rev. 2005;49(2):300-316. [48] WILLIAMS KR, MCANINCH DS, STEFANOVIC S, et al. hnRNPQ1 represses nascent axon growth in cortical neurons by inhibiting Gap-43 mRNA translation. Mol Biol Cell. 2016;27(3):518-534. [49] NASCIMENTO AI, MAR FM, SOUSA MM. The intriguing nature of dorsal root ganglion neurons: linking structure with polarity and function. Prog Neurobiol. 2018;168:86-103. [50] CUPPONE AV, SQUERI V, SEMPRINI M, et al. Robot-assisted proprioceptive training with added vibro-tactile feedback enhances somatosensory and motor performance. PloS one, 2016;11(10):e0164511. [51] RANADE SS, WOO SH, DUBIN AE, et al. Piezo2 is the major transducer of mechanical forces for touch sensation in mice. Nature. 2014;516(7529): 121-125. [52] HU S, MA X, MA X, et al. Relationship of strength, joint kinesthesia, and plantar tactile sensation to dynamic and static postural stability among patients with anterior cruciate ligament reconstruction. Front Physiol. 2023;14:45. [53] HAN GY, PARK SA, KIM JH, et al. Effects of vibration on the proteome expression of anterior cruciate ligament cells. Exp Biol Med. 2011;236(7): 783-789. [54] WANG H, JI Z, JIANG G, et al. Correlation among proprioception, muscle strength, and balance. J Phys Ther Sci. 2016;28(12):3468-3472. [55] 谷莉, 周谋望, 陈亚平, 等. 前交叉韧带重建术后影响本体感觉恢复的因素[J]. 中国康复医学杂志,2007,22(12):1095-1096. [56] LORENZ DS, BAILEY L, WILK KE, et al. Blood flow restriction training. J Athl Train. 2021;56(9):937-944. [57] 杨念恩, 李世昌, 黄文英, 等. 本体感觉差异性特点及其神经机制研究[J]. 体育科学,2014,34(4):41-48. [58] 吴苏娣, 樊小力. 肌梭结构和功能的研究进展[J]. 生理科学进展,2002, 33(2):121-125. [59] GHADERI M, LETAFATKAR A, THOMAS AC, et al. Effects of a neuromuscular training program using external focus attention cues in male athletes with anterior cruciate ligament reconstruction: A randomized clinical trial. BMC Sports Sci Med Rehabil. 2021;13(1):1-11. [60] ARUMUGAM A, BJÖRKLUND M, MIKKO S, et al. Effects of neuromuscular training on knee proprioception in individuals with anterior cruciate ligament injury: a systematic review and GRADE evidence synthesis. BMJ Open. 2021;11(5):e049226. [61] LIU S, BLANCHARD S, BIGOU S, et al. Neurotrophin 3 improves delayed reconstruction of sensory pathways after cervical dorsal root injury. Neurosurgery. 2011;68(2):450-461. [62] WANG XY, GU PY, CHEN SW, et al. Endogenous neurotrophin-3 promotes neuronal sprouting from dorsal root ganglia. Neural Regen Res. 2015;10(11): 1865-1868. [63] KUO LT, TSAI SY, GROVES MJ, et al. Gene expression profile in rat dorsal root ganglion following sciatic nerve injury and systemic neurotrophin-3 administration. J Mol Neurosci. 2011;43(3):503-515. [64] TAUSZIG-DELAMASURE S, YU LY, CABRERA JR, et al. The TrkC receptor induces apoptosis when the dependence receptor notion meets the neurotrophin paradigm. PNAS. 2007;104(33):13361-13366. [65] 张磊, 祁冀, 张少群, 等. 电针对食蟹猴前交叉韧带损伤后NT-3/TrkC信号通路的调节作用[J]. 中国中西医结合杂志,2018,38(7): 859-864. [66] 张磊, 扶世杰, 周鑫, 等. NT-3/TrkC信号通路在猴前交叉韧带本体感觉损伤中的作用[J].中国康复医学杂志,2018,33(5):513-519. [67] COSTE B, MATHUR J, SCHMIDT M, et al. Piezo1 and Piezo2 are essential components of distinct mechanically activated cation channels. Science. 2010;330:55-60. [68] MAKSIMOVIC S, NAKATANI M, BABA Y, et al. Epidermal Merkel cells are mechanosensory cells that tune mammalian touch receptors. Nature. 2014;509:617-621. [69] WOO SH, LUKACS V, DE NOOIJ JC, et al. Piezo2 is the principal mechanotransduction channel for proprioception. Nat Neurosci. 2015; 18(12):1756-1762. [70] LAI HC, SEAL RP, JOHNSON JE. Making sense out of spinal cord somatosensory development. Development. 2016;143(19):3434-3448. [71] CHAPUT M, ONATE JA, SIMON JE, et al. Visual cognition associated with knee proprioception, time to stability, and sensory integration neural activity after ACL reconstruction. J Orthop Res. 2022;40(1):95-104. [72] GROOMS DR, CHAUDHARI A, PAGE SJ, et al. Visual-motor control of drop landing after anterior cruciate ligament reconstruction. J Athl Train. 2018;53(5):486-496. [73] MOLKA AZ, LISIŃSKI P, HUBER J. Visual biofeedback exercises for improving body balance control after anterior cruciate ligament reconstruction. J Phys Ther Sci. 2015;27(7):2357-2360. [74] LION A, GETTE P, MEYER C, et al. Effect of cognitive challenge on the postural control of patients with ACL reconstruction under visual and surface perturbations. Gait Posture. 2018;60:251-257. [75] MIKO SC, SIMON JE, MONFORT SM, et al. Postural stability during visual-based cognitive and motor dual-tasks after ACLR. J Sci Med Sport. 2021; 24(2):146-151. [76] 郭亚俏, 贾静, 刘静, 等. 等速肌力视觉反馈训练对半月板损伤患者关节镜术后膝关节肌力、本体感觉和关节功能康复的影响[J]. 临床与病理杂志,2022,42(9):2221-2227. [77] 黄礼群, 王晓红, 徐丹, 等. Pro-kin平衡系统对前交叉韧带重建术后患膝本体感觉和平衡功能的影响[J]. 中华物理医学与康复杂志,2022, 44(8):739-742. [78] BUCKTHORPE M, PIROTTI E, DELLA VILLA F. Benefits and use of aquatic therapy during rehabilitation after ACL reconstruction-a clinical commentary. Int J Sports Phys Ther. 2019;14(6):978. [79] 刘国龙. 平衡促进训练影响膝关节前交叉韧带损伤重建术后患膝本体感觉的研究[J]. 河北医学,2014,20(11):1885-1888. [80] 于惠贤, 杨纯生, 张冉, 等. 本体感觉训练在膝前交叉韧带重建术后康复中的应用. 国际数字医学会, Digital Chinese Medicine. 湖南中医药大学学报2016/专集:国际数字医学会数字中医药分会成立大会暨首届数字中医药学术交流会论文集. [出版者不详],2016:647. [81] BALTACI G, HARPUT G, HAKSEVER B, et al. Comparison between Nintendo Wii Fit and conventional rehabilitation on functional performance outcomes after hamstring anterior cruciate ligament reconstruction: prospective, randomized, controlled, double-blind clinical trial. Knee Surg Sports Traumatol Arthrosc. 2013;21:880-887. [82] 吴浪, 赵祥虎, 李帅, 等. 本体感觉训练在前交叉韧带重建术后的应用[J]. 按摩与康复医学,2020,11(3):36-38. [83] 季程程, 杨鹏飞, 张信波, 等. 神经肌肉训练在前交叉韧带重建术后康复中的应用进展[J]. 中国康复理论与实践,2020,26(8):917-922. [84] KAYA D, GUNEY-DENIZ H, SAYACA C, et al. Effects on lower extremity neuromuscular control exercises on knee proprioception, muscle strength, and functional level in patients with ACL reconstruction. Biomed Res Int. 2019;2019:1694695. [85] BULOW A, ANDERSON JE, LEITER JRS, et al. Safety and Effectiveness of a Perturbation-based Neuromuscular Training Program on Dynamic Balance in Adolescent Females: A Randomized Controlled Trial. Int J Sports Phys Ther. 2021;16(4):1001. [86] COULONDRE C, SOURON R, RAMBAUD A, et al. Local vibration training improves the recovery of quadriceps strength in early rehabilitation after anterior cruciate ligament reconstruction: a feasibility randomised controlled trial. Ann Phys Rehabil Med. 2022;65(4):101441. [87] ROWE PL, TAFLAN S, HAHNE AJ. Does the Addition of Whole-Body Vibration Training Improve Postural Stability and Lower Limb Strength During Rehabilitation Following Anterior Cruciate Ligament Reconstruction: A Systematic Review With Meta-analysis. Clin J Sport Med. 2022;32(6):627-634. [88] NELSON C, RAJAN L, DAY J, et al. Postoperative rehabilitation of anterior cruciate ligament reconstruction: a systematic review. Sports Med Arthrosc Rev. 2021;29(2): 63-80. [89] SO BCL, KWOK MY, CHAN YL, et al. Lower-limb muscle activity during aquatic treadmill running in individuals with anterior cruciate ligament reconstruction. J Sport Rehabil. 2022;31(7): 894-903. [90] PEULTIER-CELLI L, MAINARD D, WEIN F, et al. Comparison of an innovative rehabilitation, combining reduced conventional rehabilitation with balneotherapy, and a conventional rehabilitation after anterior cruciate ligament reconstruction in athletes. Front Surg. 2017;4:61. [91] FU CLA, YUNG SHP, LAW KYB, et al. The effect of early whole-body vibration therapy on neuromuscular control after anterior cruciate ligament reconstruction: a randomized controlled trial. Am J Sports Med. 2013;41(4): 804-814. [92] PISTONE EM, LAUDANI L, CAMILLIERI G, et al. Effects of early whole-body vibration treatment on knee neuromuscular function and postural control after anterior cruciate ligament reconstruction: a randomized controlled trial. J Rehabil Med. 2016;48(10):880-886. [93] MA X, LU L, ZHOU Z, et al. Correlations of strength, proprioception, and tactile sensation to return-to-sports readiness among patients with anterior cruciate ligament reconstruction. Front Physiol. 2022;13: 2582. [94] 朱洪江, 郭长利, 张弘毅. 股四头肌锻炼在前交叉韧带重建术后本体感觉恢复中的作用[J]. 中国老年学杂志,2016,36(14):3507-3509. [95] ERICKSON LN, LUCAS KCH, DAVIS KA, et al. Effect of blood flow restriction training on quadriceps muscle strength, morphology, physiology, and knee biomechanics before and after anterior cruciate ligament reconstruction: protocol for a randomized clinical trial. Phys Ther. 2019;99(8):1010-1019. [96] HUGHES L, ROSENBLATT B, HADDAD F, et al. Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: A UK national health service randomised controlled trial. Sports Med. 2019;49:1787-1805. [97] JACK RA, LAMBERT BS, HEDT CA, et al. Blood flow restriction therapy preserves lower extremity bone and muscle mass after ACL reconstruction. Sports Health. 2023;15(3):361-371. [98] TAYEBI A, MOHAMMADI HK, NASSADJ G, et al. Protocol for double-blinded randomized trial to enhance postural control after anterior cruciate ligament reconstruction by balance training and concurrent cognitive demands or external focus of attention. Eur J Transl Myol. 2023;33(1):11085. [99] AHMADI P, SALEHI R, MEHRAVAR M, et al. Comparing the effects of external focus of attention and continuous cognitive task on postural control in anterior cruciate ligament reconstructed athletes. Neurosci Lett. 2020;715: 134666. [100] CHAPUT M, ONATE JA, SIMON JE, et al. Visual cognition associated with knee proprioception, time to stability, and sensory integration neural activity after ACL reconstruction. J Orthop Res. 2022;40(1):95-104. [101] KOLTYN KF, BRELLENTHIN AG, COOK DB, et al. Mechanisms of exercise-induced hypoalgesia. J Pain. 2014;15(12):1294-1304. [102] 张晓辉, 廖八根, 陈速, 等. 神经肌肉训练对运动员前交叉韧带重建术后康复的影响[J]. 中国运动医学杂志,2014,33(8):772-776. [103] 陈文祥, 谢煜, 包倪荣, 等. 关节镜下LARS人工韧带与自体腘绳肌腱对前交叉韧带重建的早期疗效比较[J]. 医学研究生学报,2017,30(2):165-168. [104] HUNNICUTT J, GREGORY C, MCLEOD M, et al. Quadriceps Recovery After Anterior Cruciate Ligament Reconstruction With Quadriceps Tendon Versus Patellar Tendon Autografts. Orthop J Sports Med. 2019;7(4): 2325967119839786. [105] 覃华生, 潘玮敏, 李然, 等. 自体腘绳肌腱重建前交叉韧带后的康复策略[J]. 中国组织工程研究,2019,23(4):628-635. [106] 王雪臣, 魏威, 王力兴, 等. 关节镜下同侧腓骨长肌腱重建前交叉韧带的疗效及对踝关节、足功能的影响[J]. 河北医药,2023,45(12):1803-1806,1811. [107] SUTTON KM, BULLOCK JM. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg. 2013;21(1):41-50. [108] JIANG L, ZHANG L, HUANG W, et al. The effect of proprioception training on knee kinematics after anterior cruciate ligament reconstruction: A randomized control trial. J Back Musculoskelet Rehabil. 2022;35(5): 1085-1095. |
| [1] | Yang Junliang, Lu Tan, Xu Biao, Jiang Yaqiong, Wang Fucheng. Three-dimensional finite element analysis of effects of partial anterior cruciate ligament rupture on knee joint stress [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1347-1353. |
| [2] | Yu Weijie, Liu Aifeng, Chen Jixin, Guo Tianci, Jia Yizhen, Feng Huichuan, Yang Jialin. Advantages and application strategies of machine learning in diagnosis and treatment of lumbar disc herniation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1426-1435. |
| [3] | Bai Chen, Yang Wenqian, Meng Zhichao, Wang Yuze. Strategies for repairing injured anterior cruciate ligament and promoting graft healing [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1457-1463. |
| [4] | Zhang Xihui, Li Zhengrong, Li Shineng, Xing Zengyu, Wang Jiao. Effect of rehabilitation training guided by Pro-kin balance system on proprioception and balance function of the affected knee after anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1259-1264. |
| [5] | Lin Zeyu, Xu Lin. Research progress in gout-induced bone destruction mechanism [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1295-1300. |
| [6] | Ma Shuwei, He Sheng, Han Bing, Zhang Liaoyun. Exosomes derived from mesenchymal stem cells in treatment of animals with acute liver failure: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1137-1142. |
| [7] | Zhang Kefan, Shi Hui. Research status and application prospect of cytokine therapy for osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 961-967. |
| [8] | Xu Rong, Wang Haojie, Geng Mengxiang, Meng Kai, Wang Hui, Zhang Keqin, Zhao Huijing. Research advance in preparation and functional modification of porous polytetrafluoroethylene artificial blood vessels [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 759-765. |
| [9] | Chen Xiaofang, Zheng Guoshuang, Li Maoyuan, Yu Weiting. Preparation and application of injectable sodium alginate hydrogels [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 789-794. |
| [10] | Liu Chuang, Shan Shuo, Yu Tengbo, Zhou Huan, Yang Lei. Advantages, discomfort and challenges of clinical application of orthopedic hemostatic materials [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 795-803. |
| [11] | Li Jiaqi, Huang Yuanli, Li Yan, Wang Chunren, Han Qianqian. Mechanism and influencing factors in molecular weight degradation of non-cross-linked hyaluronic acid [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 747-752. |
| [12] | Liu Yuhan, Fan Yujiang, Wang Qiguang. Comparison of protocols for constructing animal models of early traumatic knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 542-549. |
| [13] | Zhang Ming, Wang Bin, Jia Fan, Chen Jie, Tang Wei. Application of brain-computer interface technology based on electroencephalogram in upper limb motor function rehabilitation of stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 581-586. |
| [14] | He Yuanjie, Chen Yuheng, Zhao Yongchao, Wang Zhenglong. Progress in epigenetic regulation of vascular smooth muscle cell remodeling in the occurrence and development of aortic aneurysms [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 602-608. |
| [15] | Ma Sicong, Chen Jing, Li Yunqing. Functions and roles of connective tissue growth factor in nervous systems [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 615-620. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||