[1] SHARMA L. Osteoarthritis of the Knee. N Engl J Med. 2021;384(1):51-59.
[2] BORTOLUZZI A, FURINI F, SCIRÈ CA. Osteoarthritis and its management - Epidemiology, nutritional aspects and environmental factors. Autoimmun Rev. 2018;17(11):1097-1104.
[3] HARRIS H, CRAWFORD A. Recognizing and managing osteoarthritis. Nursing. 2015;45(1): 36-42.
[4] DHILLON MS, PATEL S, BANSAL T. Improvising PRP for use in osteoarthritis knee- upcoming trends and futuristic view. J Clin Orthop Trauma. 2019;10(1):32-35.
[5] O’CONNELL B, WRAGG NM, WILSON SL. The use of PRP injections in the management of knee osteoarthritis. Cell Tissue Res. 2019;376(2):143-152.
[6] HOSSEINI S, SOLTANI-ZANGBAR MS, ZAMANI M, et al. Comparative evaluation of autologous platelet-rich plasma and platelet lysate in patients with knee osteoarthritis.Growth Factors. 2023;41(3):165-177.
[7] DAI WL, ZHOU AG, ZHANG H, et al. Efficacy of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis: A Meta-analysis of Randomized Controlled Trials. Arthroscopy. 2017;33(3):659-670.
[8] KARIMI K, ROCKWELL H. The Benefits of Platelet-Rich Fibrin. Facial Plast Surg Clin North Am. 2019;27(3):331-340.
[9] MIJIRITSKY E, ASSAF HD, PELEG O, et al. Use of PRP, PRF and CGF in Periodontal Regeneration and Facial Rejuvenation-A Narrative Review. Biology (Basel). 2021;10(4):317.
[10] SEMMARATH W, SRISAWAD K, ARJSRI P, et al. Protective Effects of Proanthocyanidin-Rich Fraction from Red Rice Germ and Bran on Lung Cell Inflammation via Inhibition of NF-κB/NLRP3 Inflammasome Pathway. Nutrients. 2023;15(17):3793.
[11] TANAN KARACA G, DUYGU G, ER N, et al. Comparative Investigation of Anti-Inflammatory Effect of Platelet-Rich Fibrin after Mandibular Wisdom Tooth Surgery: A Randomized Controlled Study. J Clin Med. 2023;12(13):4250.
[12] XING R, WANG P, ZHAO L, et al. Mechanism of TRPA1 and TRPV4 Participating in Mechanical Hyperalgesia of Rat Experimental Knee Osteoarthritis. Arch Rheumatol. 2017;32(2):96-104.
[13] LI Z, CHEN B. DUSP4 alleviates LPS-induced chondrocyte injury in knee osteoarthritis via the MAPK signaling pathway. Exp Ther Med. 2021;22(6):1401.
[14] LI GS, CUI L, WANG GD. miR-155-5p regulates macrophage M1 polarization and apoptosis in the synovial fluid of patients with knee osteoarthritis. Exp Ther Med. 2021;21(1):68.
[15] LI Z, HUANG Z, ZHANG H, et al. P2X7 Receptor Induces Pyroptotic Inflammation and Cartilage Degradation in Osteoarthritis via NF-κB/NLRP3 Crosstalk. Oxid Med Cell Longev. 2021:2021:8868361.
[16] ZHAO LR, XING RL, WANG PM, et al. NLRP1 and NLRP3 inflammasomes mediate LPS/ATP‑induced pyroptosis in knee osteoarthritis. Mol Med Rep. 2018;17(4):5463-5469.
[17] DAINESE P, WYNGAERT KV, DE MITS S, et al. Association between knee inflammation and knee pain in patients with knee osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2022;30(4):516-534.
[18] DU C, SMITH A, AVALOS M, et al. Blueberries Improve Pain, Gait Performance, and Inflammation in Individuals with Symptomatic Knee Osteoarthritis. Nutrients. 2019;11(2):290.
[19] LIU Y, XU S, ZHANG H, et al. Stimulation of α7-nAChRs coordinates autophagy and apoptosis signaling in experimental knee osteoarthritis. Cell Death Dis. 2021;12(5):448.
[20] ZHANG L, XING R, HUANG Z, et al. Inhibition of Synovial Macrophage Pyroptosis Alleviates Synovitis and Fibrosis in Knee Osteoarthritis. Mediators Inflamm. 2019;2019:2165918.
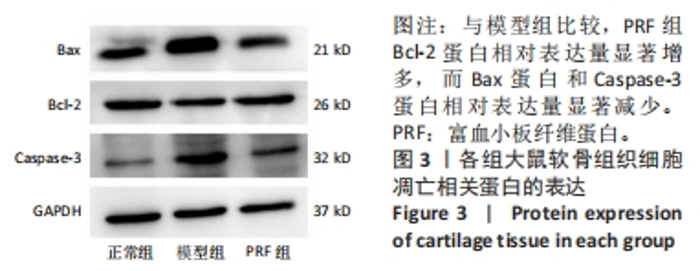
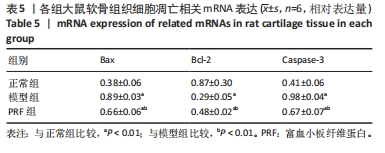
[21] ZHANG J, LI Q, CHANG S. The effects of particle density in moxa smoke on the ultrastructure of knee cartilage and expressions of TNF-α, IL-1b, BAX, and Bcl-2 mRNA in a rat model for osteoarthritis. J Cell Biochem. 2019;120(4):6589-6595.
[22] AL-MAAWI S, BECKER K, SCHWARZ F, et al. Efficacy of platelet-rich fibrin in promoting the healing of extraction sockets: a systematic review. Int J Implant Dent. 2021;7(1):117.
[23] FAN Y, PEREZ K, DYM H. Clinical Uses of Platelet-Rich Fibrin in Oral and Maxillofacial Surgery. Dental Dent Clin North Am. 2020;64(2):291-303.
[24] KOBAYASHI E, FLÜCKIGER L, FUJIOKA-KOBAYASHI M, et al. Comparative release of growth factors from PRP, PRF, and advanced-PRF. Clin Oral Investig. 2016;20(9):2353-2360.
[25] PITZURRA L, JANSEN IDC, DE VRIES TJ, et al. Effects of L-PRF and A-PRF+ on periodontal fibroblasts in in vitro wound healing experiments. J Periodontal Res. 2020;55(2):287-295.
[26] 朱琦. 注射型富血小板纤维蛋白治疗颞下颌关节骨关节炎的临床应用研究[D].昆明:昆明医科大学,2022.
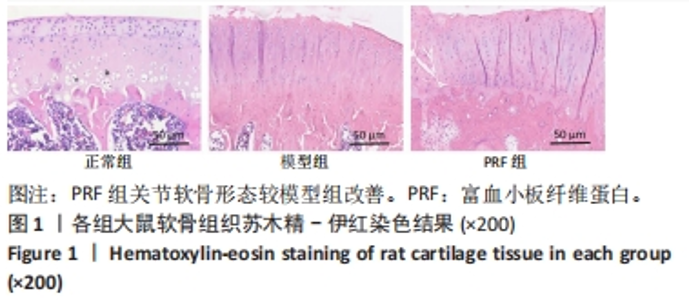
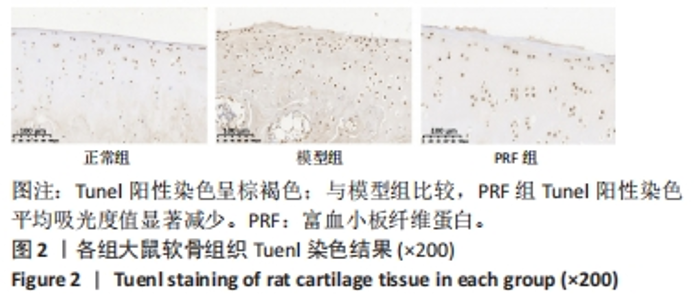
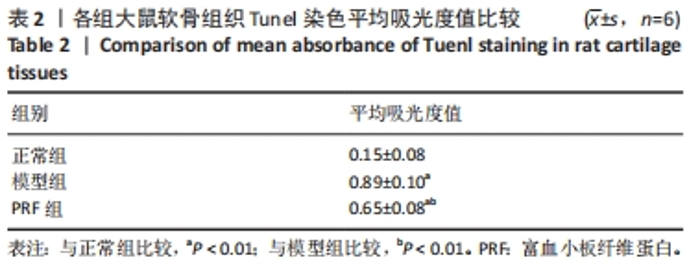
[27] 王亚全,黄富国,周德春,等.富血小板纤维蛋白修复创伤性膝关节炎模型兔的价值[J].临床和实验医学杂志,2019,18(14):1475-1479.
[28] ALRAYYES Y, AL-JASSER R. Regenerative Potential of Platelet Rich Fibrin (PRF) in Socket Preservation in Comparison with Conventional Treatment Modalities: A Systematic Review and Meta-Analysis. Tissue Eng Regen Med. 2022;19(3):463-475.
[29] FARSHIDFAR N, AMIRI MA, JAFARPOUR D, et al. The feasibility of injectable PRF (I-PRF) for bone tissue engineering and its application in oral and maxillofacial reconstruction: From bench to chairside. Biomater Adv. 2022:134:112557.
[30] SIELSKI M, CHĘCIŃSKA K, CHĘCIŃSKI M, et al. Injectable Platelet-Rich Fibrin (I-PRF) Administered to Temporomandibular Joint Cavities: A Scoping Review. J Clin Med. 2023;12(9):3326.
[31] YE JN, SU CG, JIANG YQ, et al. Effects of acupuncture on cartilage p38MAPK and mitochondrial pathways in animal model of knee osteoarthritis: A systematic evaluation and meta-analysis.Front Neurosci. 2023:16:1098311.
[32] VAN OPDENBOSCH N, LAMKANFI M. Caspases in Cell Death, Inflammation, and Disease. Immunity. 2019;50(6):1352-1364.
|