Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (20): 3213-3219.doi: 10.3969/j.issn.2095-4344.1144
Previous Articles Next Articles
Causes and treatment strategies of anterior knee pain after total knee arthroplasty
Liu Xin, Xiang Chuan
- Department of Orthopedics, the Second Affiliated Hospital of Shanxi Medical University, Taiyuan 030001, Shanxi Province, China
-
Online:2019-07-18Published:2019-07-18 -
Contact:Xiang Chuan, MD, Professor, Department of Orthopedics, the Second Affiliated Hospital of Shanxi Medical University, Taiyuan 030001, Shanxi Province, China -
About author:Liu Xin, Master candidate, Physician, Department of Orthopedics, the Second Affiliated Hospital of Shanxi Medical University, Taiyuan 030001, Shanxi Province, China
CLC Number:
Cite this article
Liu Xin, Xiang Chuan. Causes and treatment strategies of anterior knee pain after total knee arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(20): 3213-3219.
share this article
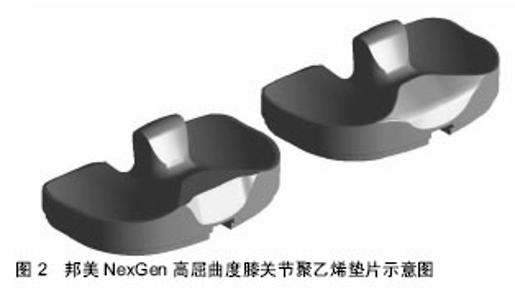
2.1 发病机制 目前,膝前痛的发病机制尚未明确,有学者认为膝前痛的发生是由多因素共同导致的[7]。大量的研究结果表明全膝关节置换术后若出现胫骨、股骨假体内旋,膝关节动态外展,股骨假体位置不良,滑车沟的大小和旋转不良等导致Q角增大及髌骨运动轨迹发生变化,使得髌股关节应力增加,显著增加膝前痛的发生率[6-10]。同时,在膝关节屈伸过程中,髌腱、髌周滑膜及脂肪垫等受到摩擦、撞击出现软组织的炎性改变,进而诱发膝前痛[11]。 Park Caroline等指出,全膝关节置换术后膝关节残余疼痛的发病机制涉及热、化学和机械刺激,这些刺激可激活周围神经系统的游离神经末梢[3-4,12]。并且在髌股关节周围有许多含大量游离神经末梢的组织结构,如股四头肌、支持带和滑膜,这些游离神经末梢一旦受到刺激,就会向中枢神经系统传递信号。A神经末梢是剧烈的急性疼痛的主要原因,而C神经末梢则传递一种迟钝的慢性疼痛。多病因都可刺激游离神经末梢,并随后导致全膝关节置换术后发生膝前痛,如低毒力细菌感染、膝关节屈曲不稳定、假体对线不良合并髌骨轨迹不良、假体无菌性松动、髌股关节症状等[13]。Breugem等[3]指出,全膝关节置换术后神经再生的过程中,若遇到瘢痕组织阻碍神经再生,则会产生神经瘤。另外,膝关节周围神经受到骨、韧带、瘢痕组织、血肿等压迫可能会引起疼痛。 2.2 发病原因 目前,大多数膝前痛的发病原因是由于多因素共同导致的,必须结合患者的病史、体征、实验室检查、影像学检查来明确诊断,进一步提供有效的治疗。 2.2.1 个体特点 许多研究报告指出,年龄、性别、体质量、身高或体质量指数与膝前痛之间没有关联,故不能用于预测全膝关节置换术后膝前痛发生的概率[14-19]。一项研究指出,全膝关节置换术后膝前痛发生的概率和严重程度与患者术后仍保持术前不良的步态相关,更大外翻角度的步态会导致髌股关节压力增高,从而增加术后膝前痛的发生率[17]。术前膝关节畸形与术后膝前痛的发生率无相关性[20],术中评估髌骨软骨受累程度与术后膝前痛之间的关系尚不确定[21-22]。Becker等[23]发现术前高于正常人的抑郁或焦虑状态、对手术过高的期望值,与膝前痛发生密切相关。越来越多的报道称有患者对金属或骨水泥过敏,局部过敏可能导致皮炎、假体无菌性松动和膝关节残余痛[24-26]。 2.2.2 假体设计 假体的设计特点与膝前痛的发生率密切相关,随着人们对膝前痛的认识,假体设计的不断改进也能有效预防膝前痛。有研究结果表明,后旋转中心股骨假体膝前痛的发生率较低[15];移动平台型假体较固定平台型假体术后膝前痛的发生率低[6]。加深滑车沟能改善髌骨的中央轨迹,从而更好地保护髌股关节,减少髌骨不稳定,同时增加膝关节屈曲的强度[27]。髌骨“非友好型”和“友好型”股骨假体在全膝关节置换术后膝前痛的发生率上无明显差异[28];后交叉韧带替换型和保留型假体在术后膝前痛发生率方面无明显差异[16];使用后稳定型胫骨假体不能明显降低术后膝前痛的发生 率[23]。边缘平滑性聚乙烯衬垫较边缘锐利型能够减少其与髌腱之间的摩擦造成的炎症反应,进而降低膝前痛的发生率,见图2。"
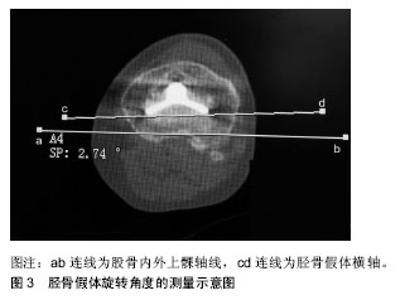
2.2.3 手术技术 (1)髌骨置换或非髌骨置换:目前全膝关节置换术中是否一期行髌骨置换仍无定论,一些学者认为置换髌骨可有效缓解由于髌骨软骨与金属假体之间相互磨擦造成的髌股关节症状,降低再次手术风险。不支持一期髌骨置换的学者则多采用髌骨成形术及环髌周去神经化,他们认为髌骨置换增加髌骨相关并发症的发生率(如髌骨骨折、髌骨脱位、假体磨损及松动等),延长手术时间,增加手术风险,影响患者术后康复[29],并且髌骨置换后翻修手术复杂。而非髌骨置换可以较好的保留原有髌骨的解剖结构,提供更好的髌骨轨迹,缩短手术时间,改善临床效果,并有效降低髌骨置换相关的并发症的发生率[30]。同时,Duan等[30]指出相比髌骨置换,髌骨去神经化更好的改善了全膝关节置换术后膝关节功能评分。Alomran[31]指出在髌骨周围电灼烧过程中,需将其距边缘距离、深度、强度标准化,以免造成过度灼烧及软骨损伤。目前没有确切的研究证实何种方法能够获得最大收益,但多数学者更倾向于选择非髌骨置换。至于髌骨置换,由于其并发症多,临床效果不确切,仍需进一步探讨、研究。 (2)髌下脂肪垫切除:髌下脂肪垫位于髌腱与胫骨前平台之间,因其影响术中胫骨平台显露,切除髌下脂肪垫可提高手术效率。但有证据表明完全去除脂肪垫可导致膝前痛及其他与髌骨相关的并发症的发生[32-34]。有分析指出完全髌下脂肪垫切除术组术后1年的膝前痛发病率高于未完全切除脂肪垫组,疼痛可能是由于缺乏脂肪垫缓冲所引起的[35]。目前,大多数学者倾向于髌下脂肪垫对预防膝前痛的发生起到积极作用。因此,建议术者在不影响手术操作的基础上,尽量保留髌下脂肪垫。 (3)其他:一项系统评价指出,膝前痛与不同的手术入路、是否使用计算机导航技术、是否行侧方松解、残余髌骨厚度无明显关联[6]。 2.2.4 机械性因素 (1)假体旋转不良:全膝关节置换术后股骨、胫骨假体存在内旋已被公认为是导致膝前痛发生的重要原因之一。Watanabe等[36]研究表明胫骨假体内旋或胫骨、股骨假体联合内旋与膝前痛有明显的相关性。胫骨假体内旋或联合内旋使得Q角增大,髌骨运动轨迹改变,髌骨及周围软组织应力增高,诱发疼痛,并增加发生髌骨脱位的风险。Nakagawa等[37]研究发现Q角增加10°可导致髌骨下方应力增加45%。同时假体旋转不良诱发的膝关节动态外翻,导致髌骨运动轨迹改变、髌股关节侧方应力增高,也可诱发疼痛[7]。研究表明,为达到最佳的膝关节功能状态,胫骨与股骨假体联合应为0°或轻度外旋3°-5°[38]。因此,术者应当熟悉各类旋转定位方法,结合患者的股骨解剖及力线特点,以求得准确的旋转对位,见图3,对改善患者的运动功能、缓解疼痛、延长膝关节的使用寿命、提高手术成功率有着重要的意义。"
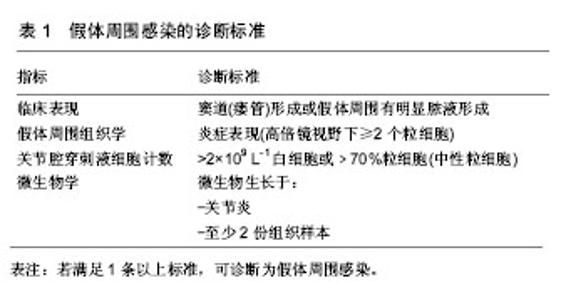
(2)胫股关节不稳:胫股关节不稳也是诱发膝前痛重要原因之一,多见于假体周围骨溶解和假体松动、过度截骨、假体破裂、假体尺寸或位置不适、聚乙烯衬垫磨损、侧副韧带损伤等。疼痛通常是胫股关节不稳的第一个迹象,常表现为关节活动及负重行走时诱发膝关节疼痛,还可出现关节肿胀、行走时步态僵硬、打软腿、外翻或内翻摆步、站立时过伸关节卡压感等[39]。屈曲中期不稳定也可导致撞击性滑膜炎和复发性关节积血等并发症。关节不稳多需行翻修手术治疗。 (3)髌股关节不稳:Kohl等[40]提出全膝关节置换术后髌股关节不稳是指髌骨轨迹不良而非指复发性关节脱位。髌骨轨迹不良已经被认为是全膝关节置换术后发生髌股关节并发症和膝前痛的一个重要原因,多由于假体对位不良、滑车沟的大小不适、软组织张力平衡不全、外翻膝关节等原因导致,这些因素可直接或间接作用影响Q角,导致膝关节生物力学发生改变,从而使得髌股关节受力不均导致膝关节撞击、卡压或疼痛。术后可通过查体及影像学检查来判断有无髌股关节不稳的发生。 (4)髌股关节过度填塞:髌股关节过度填塞是由于髌骨不对称切除、股骨前后径增大或两者共同作用的结果,可能导致膝前痛的发生。由于目前髌骨切除仍没有标准的指南或解剖标志可用来指导切割,故不对称髌骨切除造成髌股关节过度填塞。不对称髌骨切除还可导致撞击和髌骨轨迹不良。Anglin等[41]指出髌骨内、外侧超过15 mm处的髌骨厚度相差大于2 mm,一般被认为是髌骨不对称切除。另外,股骨前后径的增加多由于使用过大的股骨假体或股骨前后方截骨不足所致,这与股骨假体的设计及假体的型号有限也有关系[42]。股骨前后径增加4 mm可能导致膝关节被动屈曲4°的丢失[43]。因此,在手术时准确截骨并选择合适的股骨假体大小是至关重要的,以防发生髌股关节过度填塞。 (5)髌骨软骨溶解和髌骨坏死:未置换的髌骨软骨在全膝关节置换术后发生溶解也是诱发膝前痛的一个原因,多与髌股关节的力学改变(如髌股关节不稳、髌骨轨迹不良、假体旋转不良等)和关节退行性变密切相关。当膝前痛表现为髌骨局部压痛和骨密度改变等影像学变化时,可考虑缺血性坏死。髌骨缺血性坏死常与广泛的髌骨外侧松解相关,特别是在术前外翻畸形严重的膝关节。因此,在行髌骨外侧松解时,应注意保留膝上动 脉[13]。但Kohl等[40]研究并未发现髌骨血供减少与膝前痛存在相关性。 (6)低位髌骨:低位髌骨是膝前痛的发病原因之 一[44]。多由聚乙烯衬垫厚度较截骨的厚度过大导致关节线上移,或术后远期因髌韧带形成瘢痕挛缩造成髌骨位置下降。因此,在初次全膝关节置换术中要尽可能恢复关节线原有的位置。同时,术后应加强早期膝关节的功能活动,尽早恢复膝关节活动度,预防髌腱挛缩。 (7)软组织撞击:软组织撞击常见于Clunk综合征及滑膜增生。由于髌上的滑膜组织在髌骨上极与股四头肌腱处受到股骨髁间的摩擦,不断增生形成结节,屈膝30°-45°时,滑膜结节嵌顿于股骨髁间内,由屈曲到完全伸直的过程中,纤维结节随股四头肌腱移动而弹出股骨髁间,从而产生弹响及疼痛。滑膜增生则是在膝关节由屈曲到伸直时出现撞击,常表现为爬楼梯时引起疼痛[45]。 2.2.5 感染 感染是导致全膝关节置换术后持续性疼痛的最主要原因,也是全膝关节置换术后最严重的并发症之一。造成感染风险增加的因素主要包括自身原因(肥胖、高龄、使用激素、营养不良及合并其他内科病等)和医源性原因(如手术时间长、违反无菌操作规程、术后切口缝合不严、未合理使用抗生素等)[46]。假体周围感染所致疼痛多为静息痛和夜间痛,若术后合并关节红肿、僵硬、皮温高、渗液及窦道形成,应高度怀疑感染可能,应结合组织学及微生物学检查等明确诊断,见表1。"

2.2.6 其他 (1)牵涉痛:髋关节病变(如退行性病变、股骨头坏死等)有时可诱发膝关节疼痛。由于支配髋关节区域的神经分支也支配膝关节。通常结合患者体征及影像学检查仍无法明确诊断时,应考虑疼痛是否由髋关节病变所致,避免出现误诊。 (2)脊柱病变:由于腰椎疾病或退变引起的腰椎前凸下降可导致骨盆倾斜,进而导致膝关节伸直受限,屈曲畸形,诱发髌股关节压力升高,引起膝前痛。Tsuji等[47]把这种现象命名为膝关节-脊柱综合征。若终末期膝关节炎患者合并腰椎退行性疾病时,可出现神经根压迫症状与膝关节退变症状相重叠,难以明确引发关节疼痛的真正来源,行全膝关节置换术后有可能症状不缓解,疼痛持续存在。 (3)股四头肌肌力不足:术前股四头肌肌力不足在全膝关节置换术后对膝关节的运动模式和运动能力有着重要的影响[48]。当股四头肌肌力不平衡,股内侧肌肌力较股外侧肌减弱,导致外侧髌骨轨迹不良,加重髌股关节负荷。尽管股四头肌的肌力在全膝关节置换术后可以重新恢复,而患侧肢体的股四头肌肌力能否达到对侧健康肢体的肌力,到现在为止仍不明确[49]。而股四头肌肌力不足将影响关节的功能活动,也是导致膝前痛发生的一个因素。许多患者在全膝关节置换术后表现为避免股四头肌用力的步态,导致躯体代偿性向对侧倾斜,不利于股四头肌的锻炼和恢复,从而造成两侧造成肢体发展不平衡。另外,Merican等[50]和Sherman等[51]发现,髂胫束张力过高可导致膝关节屈曲过程中出现髌骨外移,增加了髌股关节压力。 (4)关节僵硬:关节僵硬多见于术前膝关节活动度较小、既往有膝关节手术外伤史、手术原因(如关节线抬高、过度填塞、假体位置不良等)及术后因痛拒绝早期功能锻炼者。长期膝关节活动度下降必将导致膝关节内纤维组织增生、关节僵硬。膝关节术后僵硬既是疼痛的病因,亦是疼痛的结果,易造成恶性循坏。因此,术后指导患者早期功能锻炼,恢复关节的活动度,避免发生关节僵硬至关重要。 2.3 治疗策略 全膝关节置换术后发生膝前痛的原因多种多样,一般首先考虑保守治疗,但大多数机械因素导致的膝前痛往往需手术治疗。因此,必须准确判断发病原因,制定合理的个体化治疗方案。 由患者自身原因所导致的膝前痛,术前应使患者对全膝关节置换术的利弊有正确的认识,避免产生过高的预期,必要时应给与心理疏导,有助于患者放松心情,利于术后的康复。同时,术后及时引导患者早期、规范功能锻炼,纠正术前不正确的步态姿势,可获得良好的效果。 若出现髌股关节炎加重及髌骨软骨溶解或髌骨坏死时,可考虑行二期髌骨置换术,但需严格把握手术指征及考虑手术的预期效果,据文献报道行二期髌骨置换术的成功率仅有约66%[52]。因此,行二期髌骨置换手术前,首先应排除由胫骨、股骨假体旋转不良,髌骨轨迹不良等因素导致的髌股关节应力异常增高,这些因素的持续存在往往导致二期髌骨置换术的失败[53]。 存在机械性因素的患者多合并有功能性问题,因此,对于疼痛症状轻或功能障碍不严重的患者,可以考虑先行保守治疗。而手术治疗则需严格把握适应证。当出现假体位置不正确 (偏置或旋转错误等)、膝关节不稳或假体失败(无菌性松动或破裂)时,需要考虑翻修术。一旦出现上述问题,则必须纠正病因,重建下肢的力线,改善关节活动度,恢复关节功能。同时,Pietsch等[54]指出若由股骨内旋大于4°引发的膝前痛或功能障碍,行翻修术往往能获得较好的效果。 当出现软组织撞击引发的膝前痛时,行关节镜清理能够获得较好的临床效果[55];对髌骨位置侧方偏移或倾斜角度过大者,可行关节镜下髌骨外侧松解;缺乏功能锻炼的术后膝关节僵硬也可通过松解治疗来获得较好的效果;低位髌骨,可考虑行胫骨结节截骨矫形术。 目前,针对全膝关节置换术后感染的治疗方法多种多样,包括全身或局部运用抗生素、关节腔清创灌洗、Ⅰ期或Ⅱ期翻修术、膝关节融合、截肢等[56]。由于单纯使用抗生素感染控制率低,多需要手术干预,彻底清除感染坏死组织,降低细菌量,以便彻底清除感染。若假体表面还未形成生物膜,可行关节腔清创灌洗,彻底清除感染组织,更换聚乙烯衬垫,术后大量生理盐水冲洗,联合抗生素治疗。关节腔清创灌洗虽可降低手术风险及经济负担,但其成功率较Ⅰ期或Ⅱ期翻修术低[57]。与Ⅰ期翻修相比,Ⅱ期翻修的病例常出现软组织窦道形成、耐药菌或多重感染等,虽然Ⅱ期翻修较Ⅰ期翻修感染控制率高[58-59],但其存在需行二次手术以及间隔时间较长,增加住院时间及医疗花销,降低生活质量等问题[60]。 若为髋关节、脊柱病变等因素造成膝前痛,在术前应准确做出鉴别诊断,确定疼痛来源,对因治疗,否则可能出现术后症状不缓解,患者不满意等后果。"

| [1] Mancuso CA, Ranawat AS, Meftah M, et al. Properties of the patient administered questionnaires: new scales measuring physical and psychological symptoms of hip and knee disorders. J Arthroplasty. 2012;27(4): 575-582. e6.[2] Meftah M, Ranawat AS, Ranawat CS. Ten-year follow-up of a rotating-platform, posterior-stabilized total knee arthroplasty. J Bone Joint Surgery Am. 2012;94(5): 426-432.[3] Breugem SJ, Haverkamp D. Anterior knee pain after a total knee arthroplasty: What can cause this pain? World J Orthop. 2014;5(3):163-170.[4] Grosu I, Lavand'Homme P, Thienpont E. Pain after knee arthroplasty: An unresolved issue. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1744-1758.[5] Lim HA, Song EK, Seon JK, et al. Causes of aseptic persistent pain after total knee arthroplasty. Clin Orthop Surg. 2017;9(1):50-56.[6] van Jonbergen HP, Reuver JM, Mutsaerts EL, et al. Determinants of anterior knee pain following total knee replacement: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(3):478-499.[7] Petersen W, Rembitzki IV, Bruggemann GP, et al. Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop. 2014;38(2):319-328.[8] Peersman G, Taeymans K, Jans C, et al. Malrotation deformities of the lower extremity and implications on total knee arthroplasty: a narrative review. Arch Orthop Trauma Surg. 2016;136(11):1491-1498.[9] Lavand' Homme P, Thienpont E. Pain after total knee arthroplasty: a narrative review focusing on the stratification of patients at risk for persistent pain. Bone Joint J. 2015;97-B(10 Suppl A):45.[10] Schindler OS. Basic kinematics and biomechanics of the patellofemoral joint part 2: the patella in total knee arthroplasty. Acta orthopaedica Belgica. 2012;78(1):11-29.[11] Shervin D, Pratt K, Healey T, et al. Anterior knee pain following primary total knee arthroplasty. World J Orthop. 2015;6(10):795-803.[12] Mackie A, Muthumayandi K, Shirley M, et al. Association between body mass index change and outcome in the first year after total knee arthroplasty. J Arthroplasty. 2015;30(2): 206-209.[13] Park CN, White PB, Meftah M, et al. Diagnostic algorithm for residual pain after total knee arthroplasty. Orthopedics. 2016;39(2):e246-252.[14] Lewis GN, Rice DA, Mcnair PJ, et al. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth. 2015; 114(4):551. [15] Berliner JL, Brodke DJ, Chan V, et al. Can Preoperative Patient-reported Outcome Measures Be Used to Predict Meaningful Improvement in Function After TKA? Clin Orthop Relat Res. 2016;475:1-9.[16] Lindberg MF, Miaskowski C, Rustøen T, et al. Factors that can predict pain with walking, 12 months after total knee arthroplasty. Acta Orthopaedica. 2016; 87(6):1.[17] Khatib Y, Madan A, Naylor JM, et al. Do psychological factors predict poor outcome in patients undergoing tka? a systematic review. Clin Orthop Relat Res. 2015;473(8):1-9.[18] Singh JA, Gabriel S, Lewallen D. The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res. 2008; 466(11):2717-2723.[19] Chodór P, Kruczyński J. Predicting persistent unclear pain following primary total knee arthroplasty. Ortop Traumatol Rehabil. 2016; 18(6):527-536. [20] Erak S, Rajgopal V, Macdonald SJ, et al.Ten-year results of an inset biconvex patella prosthesis in primary knee arthroplasty. Clin Orthop Relat Res. 2009;467(7): 1781-1792.[21] Zha GC, Feng S, Chen XY, et al. Does the grading of chondromalacia patellae influence anterior knee pain following total knee arthroplasty without patellar resurfacing? Int Orthop. 2018;42(3):513-518.[22] Rodriguez-Merchan EC, Gomez-Cardero P. The outerbridge classification predicts the need for patellar resurfacing in TKA. Clin Orthop Relat Res. 2010;468(5): 1254-1257.[23] Becker R, Döring C, Denecke A , et al. Expectation, satisfaction and clinical outcome of patients after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011; 19(9):1433-1441.[24] Amini M, Mayes WH, Tzeng A, et al. Evaluation and management of metal hypersensitivity in total joint arthroplasty: a systematic review. J Long Term Eff Med Implants. 2014;24(1):25-36. [25] Bergschmidt P, Bader R, Mittelmeier W. Metal hypersensitivity in total knee arthroplasty: revision surgery using a ceramic femoral component - a case report. Knee. 2012;19(2):144-147.[26] Bircher A, Friederich NF, Seelig W, et al. Allergic complications from orthopaedic joint implants: the role of delayed hypersensitivity to benzoyl peroxide in bone cement. Contact Dermatitis. 2012;66(1):20-26.[27] Indelli PF, Marcucci M, Cariello D, et al. Contemporary femoral designs in total knee arthroplasty: effects on the patello-femoral congruence. Int Orthop. 2012;36(6): 1167-1173.[28] Pavlou G, Meyer C, Leonidou A, et al. Patellar resurfacing in total knee arthroplasty: does design matter? A meta-analysis of 7075 cases. J Bone Joint Surg Am. 2011; 93(14):1301-1309.[29] Schiavone Panni A, Cerciello S, Del Regno C, et al. Patellar resurfacing complications in total knee arthroplasty. Int Orthop. 2014;38(2):313-317.[30] Duan G, Liu C, Lin W, et al. Different factors conduct anterior knee pain following primary total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2018;33(6):1962-1971.e3.[31] Alomran A. Effect of patellar denervation on mid-term results after non-resurfaced total knee arthroplasty. A randomised, controlled trial. Acta Orthopaedica Belgica. 2015;81(4):609-613.[32] Ye C , Zhang W , Wu W , et al. Influence of the infrapatellar fat pad resection during total knee arthroplasty: a systematic review and meta-analysis Plos One. 2016;11(10):e0163515.[33] Seo J, Lee S, Moon YW , et al. Infrapatellar fat pad preservation reduces wound complications after minimally invasive total knee arthroplasty. Arch Orthop Trauma Surg. 2015;135(8):1157-1162.[34] Van Beeck A, Clockaerts S, Somville J, et al. Does infrapatellar fat pad resection in total knee arthroplasty impair clinical outcome? A systematic review. Knee. 2013; 20(4):226-231.[35] ?mren Y, Dedeo?lu SS, Çakar M, et al. Infrapatellar fat pad excision during total knee arthroplasty did not alter the patellar tendon length: a 5-year follow-up study. J Knee Surg. 2016;30(05):479-483.[36] Watanabe S, Sato T, Omori G, et al. Change in tibiofemoral rotational alignment during total knee arthroplasty. J Orthop Sci. 2014;19(4):571-578.[37] Nakagawa TH, Serrao FV, Maciel CD, et al. Hip and knee kinematics are associated with pain and self-reported functional status in males and females with patellofemoral pain. Int J Sports Med. 2013;34(11):997-1002.[38] Bell SW, Young P, Drury C, et al. Component rotational alignment in unexplained painful primary total knee arthroplasty. Knee. 2014;21(1):272-277.[39] Can A, Erdogan F, Erdogan AO. Tibiofemoral instability after primary total knee arthroplasty: posterior-stabilized implants for obese patients. Orthopedics. 2017;40(5):1. [40] Kohl S, Evangelopoulos DS, Hartel M, et al. Anterior knee pain after total knee arthroplasty: does it correlate with patellar blood flow? Knee Surg Sports Traumatol Arthrosc. 2011;19(9):1453-1459. [41] Anglin C, Fu C, Hodgson AJ, et al. Finding and defining the ideal patellar resection plane in total knee arthroplasty. J Biomech. 2009;42(14):2307-2312.[42] Hamilton DF, Burnett R, Patton JT, et al. Implant design influences patient outcomeafter total knee arthroplasty. Bone Joint J. 2015;97-B(1):64.[43] Mihalko W, Fishkin Z, Krackow K. Patellofemoral overstuff and its relationship to flexion after total knee arthroplasty. Clin Orthop Relat Res. 2006;449:283-287.[44] 李建平,彭昊,陈森,等. 全膝关节置换术后膝前痛的原因分析及对策[J]. 中国矫形外科杂志, 2014, 22(19):1778-1782.[45] Dajani KA, Stuart MJ, Dahm DL, et al. Arthroscopic treatment of patellar clunk and synovial hyperplasia after total knee arthroplasty. J Arthroplasty. 2010;25(1):97-103. [46] Kalore NV, Gioe TJ, Singh JA. Diagnosis and management of infected total knee arthroplasty. Open Orthop J. 2011;5: 86-91.[47] Tsuji T, Matsuyama Y, Goto M, et al. Knee-spine syndrome: correlation between sacral inclination and patellofemoral joint pain. J Orthop Sci. 2002;7(5):519-523.[48] Moon YW, Kim HJ, Ahn HS, et al. Serial Changes of quadriceps and hamstring muscle strength following total knee arthroplasty: a meta-analysis. Plos One. 2016;11(2): e0148193.[49] Guler O, Mahirogullari M, Isyar M, et al. Comparison of quadriceps muscle volume after unilateral total knee arthroplasty with and without tourniquet use. Knee Surg Sports Traumatol Arthrosc. 2015;24(8):1-11.[50] Merican AM, Amis AA. Iliotibial band tension affects patellofemoral and tibiofemoral kinematics. J Biomech. 2009;42(10):1539-1546.[51] Sherman SL, Plackis AC, Nuelle CW. Patellofemoral anatomy and biomechanics. Clin Sports Med. 2014;33(3): 389-401.[52] Chen K, Li G, Fu D, et al. Patellar resurfacing versus nonresurfacing in total knee arthroplasty: a meta-analysis of randomised controlled trials. Int Orthop. 2013;37(6): 1075-1083.[53] 计忠伟,包倪荣,赵建宁. 人工全膝关节置换术后疼痛原因分析[J]. 中国骨伤, 2014, 27(11):970-975.[54] Pietsch M, Hofmann S. Early revision for isolated internal malrotation of the femoral component in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012; 20(6):1057-1063.[55] Dajani KA, Stuart MJ, Dahm DL, et al. Arthroscopic treatment of patellar clunk and synovial hyperplasia after total knee arthroplasty. J Arthroplasty. 2010;25(1):97-103.[56] Matthews PC, Berendt AR, McNally MA, et al. Diagnosis and management of prosthetic joint infection. BMJ. 2009; 338:b1773.[57] Engesaeter LB, Dale H, Schrama JC, et al. Surgical procedures in the treatment of 784 infected thas reported to the norwegian arthroplasty register. Acta orthopaedica. 2011;82(5):530-537.[58] Kapadia BH, Berg RA, Daley JA, et al. Periprosthetic joint infection. Lancet (London, England). 2016;387(10016): 386-394.[59] Cancienne JM, Werner BC, Bolarinwa SA, et al. Removal of an infected total hip arthroplasty: risk factors for repeat debridement, long-term spacer retention, and mortality. J Arthroplasty. 2017;32(8):2519-2522.[60] Chen KH, Tsai SW, Wu PK, et al. Partial component-retained two-stage reconstruction for chronic infection after uncemented total hip arthroplasty: results of sixteen cases after five years of follow-up. Int Orthop. 2017; 41(12):2479-2486. |
| [1] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [2] | Zhao Zhongyi, Li Yongzhen, Chen Feng, Ji Aiyu. Comparison of total knee arthroplasty and unicompartmental knee arthroplasty in treatment of traumatic osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 854-859. |
| [3] | Yuan Jun, Yang Jiafu. Hemostatic effect of topical tranexamic acid infiltration in cementless total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 873-877. |
| [4] | Mieralimu•Muertizha, Ainiwaerjiang•Damaola, Lin Haishan, Wang Li . Relationship between tibio-femoral mechanical axis deviation on coronal plane and early joint function recovery after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3300-3304. |
| [5] | Deng Zhibo, Li Zhi, Wu Yahong, Mu Yuan, Mu Yuexi, Yin Liangjun. Local infiltration anesthesia versus femoral nerve block for pain control and safety after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3401-3408. |
| [6] | Huang Chenyu, Tang Cheng, Wei Bo, Li Jiayi, Li Xuxiang, Zhang Huikang, Xu Yan, Yao Qingqiang, Wang Liming. Application of three-dimensional printing guide plate in total knee arthroplasty for patients with varus and valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2789-2793. |
| [7] | Li Shangzhi, Zheng Dezhi, Liu Jun. Early analgesia of cocktail therapy after total knee arthroplasty with enhanced recovery after surgery program [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2794-2798. |
| [8] | Liu Jinlei, Yin Li, Zhang Yi, Wang Haitao, Li Zhuangyan, Xia Peige, Qiao Renqiu. Effects of intravenous tranexamic acid combined with periarticular multipoint injection of tranexamic acid cocktail on blood loss and pain after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2833-2839. |
| [9] | Xu Hui, Kang Bingxin, Gao Chenxin, Zhao Chi, Xu Xirui, Sun Songtao, Xie Jun, Xiao Lianbo, Shi Qi. Effectiveness of Tuina in the treatment of pain after total knee arthroplasty in patients with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2840-2845. |
| [10] | Deng Bo, Hong Hainan, Fan Yongyong, Cai Guoping, Feng Xingbing, Hong Zhenghua. Efficacy and safety of tourniquet application in total knee arthroplasty and only at the time of cementing: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2908-2914. |
| [11] | Liu Kun, Xu Hao, Wang Yingzhen, Zhang Haining, Fang Yuan, Xiang Shuai, Lü Chengyu. Direct repair of medial collateral ligament injury combined with brace in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2352-2357. |
| [12] | Wang Feng, Ju Xiaocong, Wang Bing, Sun Haining. Lateral unicompartmental knee arthroplasty and total knee arthroplasty for treating lateral single compartment knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1836-1841. |
| [13] | Lin Yi, Feng Jierong, Luo Xingwen. Mobilization with movement facilitates early functional recovery after fixed-bearing posterior stabilized total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1842-1846. |
| [14] | Pei Tianlong, Wang Yongkang, Wu Wenjie, Zhao Hong, Wang Longsheng . Anatomical and morphological characteristics of knee joint in hemophilic arthritis patients with three-dimensional CT and X-ray films [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(12): 1886-1890. |
| [15] |
Yin Jiandong, Wang Xinling, Zuo Biao, Li Nongyi.
Relationship of extrusion and elevation of blood-expelling methods during
total knee arthroplasty with postoperative complications |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||