Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (20): 3220-3228.doi: 10.3969/j.issn.2095-4344.1153
Previous Articles Next Articles
Newest progress in diagnosis and treatment of anterior cruciate ligament combined with medial collateral ligament injury
Wang Hao, Chen Guojian, Liang Haibo, Feng Xinjian, Cen Liangjue, Han Jie, Qin Zhi, Zhu Shengwang, Zeng Feng, Li Shuzhen
- Department of Joint and Sports Surgery, Ruikang Hospital Affiliated to Guangxi University of Chinese Medicine, Nanning 530001, Guangxi Zhuang Autonomous Region, China
-
Online:2019-07-18Published:2019-07-18 -
Contact:Li Shuzhen, Master, Associate chief physician, Department of Joint and Sports Surgery, Ruikang Hospital Affiliated to Guangxi University of Chinese Medicine, Nanning 530001, Guangxi Zhuang Autonomous Region, China -
About author:Wang Hao, Master candidate, Physician, Department of Joint and Sports Surgery, Ruikang Hospital Affiliated to Guangxi University of Chinese Medicine, Nanning 530001, Guangxi Zhuang Autonomous Region, China -
Supported by:the Natural Science Foundation of Guangxi Zhuang Autonomous Region (General Program), No. 2017JJA140564z (to LSZ)
CLC Number:
Cite this article
Wang Hao, Chen Guojian, Liang Haibo, Feng Xinjian, Cen Liangjue, Han Jie, Qin Zhi, Zhu Shengwang, Zeng Feng, Li Shuzhen. Newest progress in diagnosis and treatment of anterior cruciate ligament combined with medial collateral ligament injury[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(20): 3220-3228.
share this article
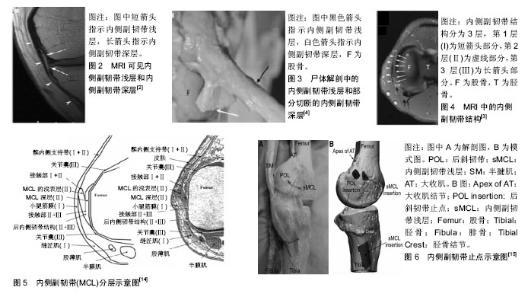
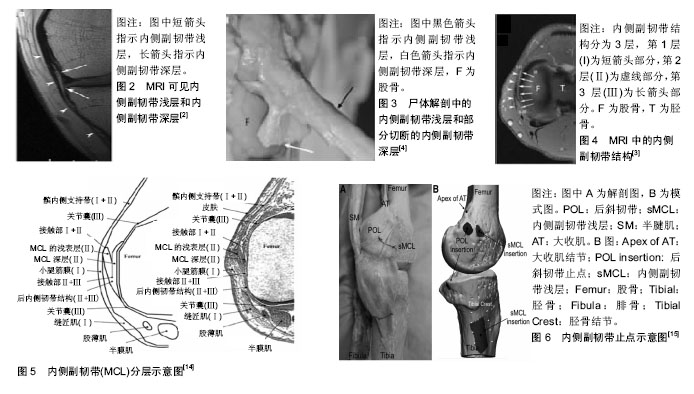
2.1 前交叉韧带和内侧副韧带的解剖结构 内侧副韧带位于膝关节的后内侧,以解剖层次划分,可分为内侧副韧带深层和内侧副韧带浅层。其中内侧副韧带浅层是稳定膝关节内侧的主要结构[2];其起自于股骨内上髁,止于内侧关节线下5-7 cm处,平均长度是11 cm,平均宽度是1.5 cm;而内侧副韧带深层起自股骨内髁,止于关节内侧边缘下方,形成半月板股骨韧带和半月板胫骨韧带,见图2[3-4]。内侧副韧带可分为3层,第1层由小腿深筋膜、深筋膜后方部分覆盖于缝匠肌肌腱上,见图3;第2层由内侧副韧带浅层、小腿深筋膜前方部分和内侧副韧带第3层的后方部分构成;第3层由内侧副韧带深层构成,这一层非常靠近膝关节囊和股骨内髁;内侧副韧带滑囊位于第2层和第3层之间,见图4,5[4]。内侧副韧带与后斜韧带及后内侧关节囊共同构成膝关节后内侧复合体,共同维持膝关节内侧的稳定性[5];后斜韧带起自于股骨远端的内收肌结节,在胫骨近端有3个附着点:①胫骨后方边缘最突出的部分;②后关节囊和腘斜韧带的边缘部分;③半膜肌肌腱的止点,见图6。前交叉韧带位于股骨髁间窝内,起自于股骨外髁内侧壁后方,向前下方分布,止于胫骨髁间嵴的前方;有研究认为前交叉韧带在解剖上呈现为带状[6-7]。?migielski等[8]通过尸体研究得出前交叉韧带中间实质部分为带状样韧带,没有出现分束结构。Mochizuki等[9]也认为前交叉韧带中间实质部分为扁平状结构。前交叉韧带可分为前内侧束和后外侧束[3],前内侧束与后外侧束呈近椭圆形,解剖位置上前内侧束更靠近下方[10];前内侧束在膝关节屈曲位时保持紧张,限制膝关节前后过度移动;而后外侧束在膝关节伸直位时保持紧张,防止膝关节过度旋转[11]。后内侧复合体与前交叉韧带形成“扣锁机制”来维持膝关节的稳定,防止膝关节过度前向或后向运动[12]。“扣锁机制”是指在膝关节屈曲过程中,胫骨会出现外旋,在膝关节屈曲90°-120°时,此时胫骨外旋角度最大,最大外旋角度为45°;当膝关节在伸直过程中,胫骨处于内旋状态,而在伸直的最后阶段,胫骨会出现外旋从而使前交叉韧带紧张,以此来维持膝关节的稳定。膝关节在屈曲到伸直过程中胫骨和股骨经历了多个方向的运动,其稳定性的保持与周围韧带的完整性关系密切。当后内侧复合体合并前交叉韧带损伤时,膝关节的前向稳定性和外翻稳定性受到破坏,同时“扣锁机制”受到破坏,从而继发膝关节多方向不稳[13]。"
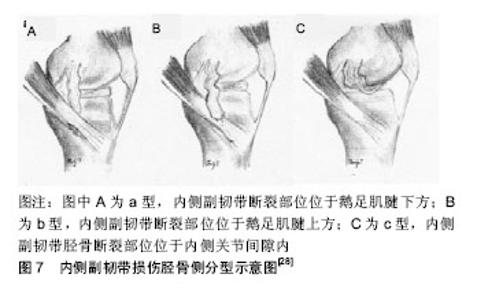
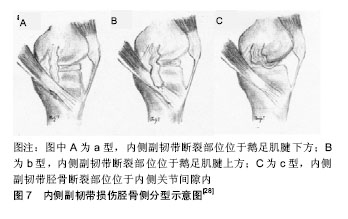
2.2 前交叉韧带和内侧副韧带的生物力学 目前对于前交叉韧带和内侧副韧带的生物力学研究已经有大量的报道。单纯前交叉韧带损伤会影响膝关节的前向稳定性,同时对周围组织有继发损伤的情况。姚杰等[16]通过对膝关节进行三维有限元研究,用计算机对膝关节进行造模,同时在屈膝0°和30°时对胫骨逐渐施加前向载荷,结果发现胫骨前移距离逐渐增加,同时内侧半月板后角部分应力增大,内侧副韧带、外侧半月板以及后交叉韧带的应力均出现不同程度的增高。单纯的内侧副韧带损伤会使膝关节的在外翻应力下出现松弛,内侧副韧带有维持膝关节外翻稳定的作用,Phisitkul等[3]在一项尸体研究中发现,在膝关节屈曲5°时,内侧副韧带提供57%的限制膝关节外翻作用;膝关节屈曲25°时,关节囊减少了限制膝关节外翻的作用,此时内侧副韧带提供了78%的限制作用。Kennedy等[17]认为内侧副韧带的最大强度可以接近前交叉韧带。Robinson等[18]通过对膝关节内侧结构进行应力进行测试后,发现内侧副韧带浅层的最大应力是534 N,内侧副韧带深层的最大应力是194 N,后斜韧带的最大应力是425 N;当以上结构分别延伸10.2,7.2,12 mm时,会发生断裂。当膝关节完全伸展时,从尸体研究中发现整个内侧副韧带复合物的最大应变位置在韧带的股骨止点附近,这与一些临床和实验室的发现相吻合,这表明内侧副韧带股骨止点是最常见的损伤部位[19-24]。在前交叉韧带联合内侧副韧带损伤时,膝关节的前向稳定性和外翻稳定性均会出现不稳。Matsumoto等[25]对6个尸体膝关节胫骨部分持续施加平均12.2 Nm的外翻转矩,没有限制胫骨内旋程度(正常为5°内旋);其中3个膝关节先切断前交叉韧带,再切断内侧副韧带进行观察,单独切断前交叉韧带时膝关节外翻角度较正常水平显著增加,继而切断内侧副韧带,发现在膝关节外翻角度较单独切断前交叉韧带时显著增加;在关节内侧间隙的观察中,单独切除前交叉韧带时,关节内侧分离程度较正常时显著增加(分离距离没有超过2.1 mm),当前交叉韧带和内侧副韧带均切断时,关节内侧分离程度则较单独切断前交叉韧带时显著增加,分离距离为2.7-6.3 mm;在胫骨内旋程度的研究中,单独切断前交叉韧带时,胫骨内旋程度较正常显著增加,当前交叉韧带和内侧副韧带均切断时,胫骨内旋程度减少;另外3个膝关节先切断内侧副韧带,再切断前交叉韧带进行观察,发现在单独切断内侧副韧带浅层时,膝关节屈曲过程中外翻角度显著增加,而当内侧副韧带浅层和前交叉韧带均切断时,关节外翻程度较单独切断内侧副韧带浅层增加,并且外翻角度在膝关节屈曲0°-30°时为单独切断内侧副韧带浅层关节外翻角度的两三倍;在关节内侧分离程度的实验中,单独切断内侧副韧带浅层时,关节内侧分离程度在屈曲过程中较正常膝关节增加1.9-7.8 mm,在膝关节屈曲20°- 40°时,关节内侧分离程度超过6 mm,当将前交叉韧带和内侧副韧带浅层均切断后,关节分离程度较单独切断内侧副韧带浅层增加0.9-2.2 mm;在胫骨旋转角度的观察中,当切断 内侧副韧带浅层后,膝关节屈曲时胫骨外旋角度较正常增加明显,在膝关节屈曲15°-45°时有超过5°的内旋,当前交叉韧带和内侧副韧带浅层同时切断时,膝关节屈曲时胫骨外旋角度较切断内侧副韧带浅层明显减少,在膝关节屈曲10°-30°时胫骨外旋角度减少最多(超过5°)。 通过以上生物力学研究,可以得出内侧副韧带和前交叉韧带对膝关节的稳定性起着至关重要的作用。如果仅强调重建前交叉韧带而忽视内侧副韧带的修复,则会影响膝关节的稳定性,导致患者重建后膝关节功能,重建后满意度下降,因此在临床上,运动医学医生应对内侧副韧带损伤予以重视。 2.3 内侧副韧带损伤的分型 通过对内侧副韧带损伤进行分型,可以指导临床对相应分型的内侧副韧带损伤选择合适的治疗方案。目前内侧副韧带损伤分型有5型,Fetto等[26]在1978年首先提出内侧副韧带损伤分型,将内侧副韧带损伤分为3级,Ⅰ级损伤定义为在膝关节屈曲0°和30°的时候没有出现外翻松弛;Ⅱ级损伤为在膝关节屈曲30°时出现外翻松弛,在屈曲0°时则没有出现松弛;Ⅲ级损伤表现为在膝关节屈曲30°和0°时均出现外翻松弛;该分型仅针对患者体征进行分类,对患者的症状没有进一步描述,Hughsyon[27]按内侧副韧带损伤严重程度(Ⅰ级、Ⅱ级、Ⅲ级)和关节松弛程度(1+,2+,3+)进行分型,内侧副韧带Ⅰ级损伤表现为韧带纤维部分撕裂,局部疼痛,没有影响膝关节稳定性;内侧副韧带Ⅱ级损伤表现为韧带纤维撕裂程度进一步增大,局部疼痛感增加,没有影响膝关节稳定性;内侧副韧带Ⅲ级损伤表现为韧带完全撕裂,影响到膝关节稳定性;而内侧副韧带Ⅲ级损伤根据膝关节在屈曲30°予以外翻应力时关节分离程度进一步分型,松弛程度1+表现为关节分离3-5 mm,松弛程度2+表现为6-10 mm,松弛程度3+表现为关节分离程度超过10 mm。近年来随着对内侧副韧带损伤的进一步研究,Taketomi等[28]对内侧副韧带损伤提出一种新的分型,发现内侧副韧带胫骨止点损伤会在MRI上呈现出“皱褶征”,认为在MRI发现“皱褶征”是诊断内侧副韧带在胫骨侧损伤的重要标志,同时通过术中观察将内侧副韧带在胫骨侧损伤分为3型,a型为内侧副韧带断裂部位位于鹅足肌腱下方;b型是内侧副韧带断裂部位位于鹅足肌腱上方;c型是内侧副韧带胫骨断裂部位位于内侧关节间隙内,见图7。"

Blanke等[29]等在Fetto等[26]分型的基础上根据是否存在关节前内侧不稳情况进行分型,存在关节前内侧不稳的膝关节为A型,不存在关节前内侧不稳的膝关节为B型,以此作为内侧副韧带手术治疗的适应证。许宏涛 等[30]在Hughsyon[27]和Fetto等[26]分型的基础上,将内侧副韧带损伤分为单独损伤和内侧副韧带合并前交叉韧带损伤2种分型。目前内侧副韧带损伤的分型有以上5型,临床上针对内侧副韧带单独损伤比较常用分型为Fettohe&Marshall分型和Hughsyon分型,因为这2种分型在临床上操作简便,同时易于诊断出内侧副韧带损伤。针对合并损伤,许宏涛分型比较直观,运动医学医生容易掌握。通过损伤分型有利于运动医学医生在临床上对内侧副韧带损伤的患者选择合适的治疗方案,有利于指导临床治疗,同时观察预后,提高患者的治疗满意度。 2.4 前交叉韧带合并内侧副韧带损伤的治疗策略 临床上确诊前交叉韧带合并内侧副韧带损伤后,应根据损伤的时间、损伤的部位和损伤程度给予不同的治疗方案,以修复损伤并维持膝关节的稳定性。许多研究显示了重建前交叉韧带联合保守治疗内侧副韧带损伤取得了满意的效果[29,31-32]。因为内侧副韧带的血供较好,其肌成纤维细胞能在内侧副韧带损伤后提供修复作用[33]。许宏涛等[30]认为针对内侧副韧带单独损伤,应进行保守治疗;针对前交叉韧带合并内侧副韧带损伤,若内侧副韧带损伤分型为HughsyonⅠ型和Ⅱ型,则先保守治疗内侧副韧带,二期行前交叉韧带重建;若内侧副韧带损伤为Hughsyon Ⅲ型,则根据Fettohe&Marshall分型,若外翻实验阴性,则保守治疗内侧副韧带,二期行前交叉韧带重建;若外翻实验阳性,则对内侧副韧带和前交叉韧带均行手术治疗。Tandogan等[34]认为几乎所有内侧副韧带Ⅰ级和Ⅱ级损伤的患者都可以保守治疗,予患肢绷带固定和冰敷3-6周,支具外翻制动,并予部分负重,以此来促进韧带修复,支具在屈伸活动上不予限制,以早期恢复膝关节的屈伸功能。Lundberg等[35]对38例内侧副韧带Ⅰ级和Ⅱ级损伤(Hughsyon分型)的患者予以保守治疗并且随访10年,有一半的患者在随访第4年Lysholm评分为100分,随访第10年有95%的患者Lysholm评分为100分,保守治疗的效果满意。Pressman等[36]认为前交叉韧带联合内侧副韧带Ⅰ级和Ⅱ级损伤应对膝关节进行支具固定2周,期间嘱咐患者主被动活动膝关节,评估内侧副韧带的愈合情况,直到膝关节的活动度、肌力恢复和关节积液减少时再进行前交叉韧带重建。Blanke等[29]认为应对前交叉韧带合并内侧副韧带损伤患者,先进行膝关节制动6周,然后通过外翻应力实验对保守治疗内侧副韧带的效果进行评估,如果仍存在关节前内侧不稳,则对内侧副韧带进行手术治疗,所有的前交叉韧带重建也在损伤后6周后执行。临床上部分保守治疗内侧副韧带的病例疗效满意[37-39],但对于内侧副韧带Ⅲ级损伤的治疗方案存在争议,主要原因是内侧副韧带Ⅲ级损伤一般联合有前交叉韧带损伤。在一些临床和动物实验的研究中发现如果单纯重建前交叉韧带而不修复内侧副韧带会影响膝关节的稳定性[40-43],因此在膝关节内侧结构损伤的病例中,选择手术还是保守治疗仍处于争论中[44-45]。目前对于内侧副韧带Ⅰ级和Ⅱ级损伤主张保守治疗,评估保守治疗效果,若效果不满意则选择手术重建,对于内侧副韧带Ⅲ级损伤也可主张保守治疗,但是当合并有其他结构的损伤,如前交叉韧带或后交叉韧带损伤时,一般主张先修复前交叉韧带或后交叉韧带损伤,后治疗内侧副韧带损伤[46-47],对于前交叉韧带损伤,国内外学者均认为韧带重建是最合适的治疗方法,通过手术治疗能够最大程度的恢复膝关节的外旋和前向稳定性。 作者根据临床经验认为在合并伤中,所有的前交叉韧带损伤均应进行韧带重建,内侧副韧带Ⅰ级和Ⅱ级损伤,可保守治疗6周,若保守治疗后外翻应力实验仍为阳性,则考虑手术治疗;而内侧副韧带Ⅲ级损伤,均予手术治疗,若是外翻应力实验阳性则一期手术治疗,外翻应力实验阴性则一期行前交叉韧带重建,二期行内侧副韧带手术治疗。 2.4.1 前交叉韧带损伤的手术方式选择 目前对于前交叉韧带损伤临床首选韧带重建,韧带重建能最大程度恢复膝关节外旋和前向稳定性,目前前交叉韧带重建技术有“等长重建”和“解剖重建”两种。传统的等长重建是指韧带重建后移植物在膝关节屈伸活动时保持长度不变,从而使移植物在腱骨界面保持稳定[48],但是该技术存在各方面的局限性,如骨道选取的进针点难以把控[49],很难实现等长重建,同时该重建技术难以恢复前交叉韧带的张 力[50],重建后膝关节的外旋存在不稳的情况[51],而解剖重建可以解决这些问题,即按原前交叉韧带的解剖位置进行重建,该重建技术可以既可以解决前交叉韧带的张力问题,同时能够恢复膝关节的外旋稳定性[52],实现解剖重建要在重建前对前交叉韧带的直径、双束或是单束重建、患者生活方式等进行综合考虑[53-54]。有研究认为适合单束解剖重建的韧带止点前后径应 < 14 mm,如果大于14 mm则适合双束重建[55];此外,有生物力学研究证实解剖重建能够恢复前交叉韧带原有的生物力学状态,进而改善膝关节外旋不稳定的情况[56]。 解剖重建前交叉韧带面临骨道钻取问题,特别是股骨隧道,目前针对股骨隧道有大量研究报道,Pearle等[57]针对股骨骨道特点提出了IDEAL原则,即骨道的位置在应该与原先股骨骨道位置等距(I),移植物应该完全覆盖骨道(D),骨道的偏心距应该位于足印区的前下方(E),骨道应解剖重建(A),应该尽可能恢复移植物在膝关节屈伸时的张力(L)。传统制备骨道的方法为经胫骨隧道入路,即先钻取胫骨隧道,经胫骨钻取股骨隧道,此法制作的股骨隧道的优点是基于解剖、降低撞击、操作时便于过线,钻取骨道时不需极度屈曲膝关节,但是过分依赖胫骨定位,容易造成股骨隧道定位不佳。Kopf等[58]通过对比经胫骨隧道入路技术钻取的骨道和原前交叉韧带足印区的解剖位置,发现无论是胫骨隧道还是股骨隧道,经胫骨隧道入路技术均不能使钻取的隧道接近解剖位置。由于经胫骨隧道入路技术存在缺陷,前内侧入路技术被应用于前交叉韧带重建中,该技术便于操作,能够降低撞击,同时临床效果好。在经胫骨隧道入路技术与前内侧入路技术的比较中,Takeda等[59]在尸体研究中发现,相较于经胫骨隧道入路技术,前内侧入路技术钻取的股骨隧道更加靠近足印区的中心,同时隧道的长度更短。Tashiro等[60]在同样的研究中发现利用经胫骨隧道入路技术钻取的股骨隧道前内侧隧道位置浅、孔径大,隧道重叠频率高,而用前内侧入路技术更有利于股骨隧道的解剖制备,避免隧道外观椭圆化和重叠。de Abreu-e-Silva等[61]对行经胫骨隧道入路技术和前内侧入路技术重建前交叉韧带的患者进行随访,重建后2年体格检查发现前内侧入路组在Lachman实验、轴移试验、前抽屉实验和关节活动度方面均优于经胫骨隧道入路组,在三维CT观察中发现前内侧入路组钻取的骨道更加接近解剖位置。Venosa等[62]通过研究表明辅助内侧入路技术相比经胫骨隧道入路技术可以给移植物提供更接近解剖位置的骨道。Shetty等[63]将经胫骨隧道入路技术和前内侧入路技术钻取的骨道进行研究,X射线正位片显示前内侧入路组的股骨角度比经胫骨隧道入路组大;在X射线侧位片显示,与经胫骨隧道入路组相比,前内侧入路组股骨角度较大,股骨隧道置入螺钉角度较小,移植物角度更加水平。预后方面,Sukur等[64]通过研究显示前内侧入路组能更快的恢复正常生活和慢跑,目测类比评分较经胫骨隧道入路组明显降低,同时前内侧入路组有51例股骨隧道位置符合解剖学要求,而经胫骨隧道入路组仅有5例。Liu等[65]也通过研究得出通过前内侧入路技术钻取的股骨隧道重建前交叉韧带后,显著高于经胫骨隧道入路技术重建前交叉韧带的患者,Lachman实验的阴性率前内侧入路组也高于经胫骨隧道入路组。在其他前交叉韧带股骨隧道的研究中,Kim等[66]发现,相比于传统经胫骨隧道入路技术,移植物在由外向内技术制备的股骨隧道中弯曲的角度更小,骨道的长度更长,并且关节内的骨道位置更接近解剖位置。在其他股骨隧道钻取技术的研究中,辅助内侧入路技术重新被提及[67-68],位于传统内侧入路偏内侧 2 cm、偏下5 mm,此入路的优势是在观察前交叉韧带股骨足印区时视野更佳,由此入路钻取股骨骨道能够最大程度接近解剖位置[69]。Tompkins等[70]对辅助内侧入路技术入路和经胫骨隧道入路入路制备的股骨隧道特点进行研究,发现前者制备的骨道位置更偏前,更加水平,重建后的前交叉韧带在控制膝关节旋转和前向移动具有较大优势。Burnham等[71]通过在对比前内侧入路技术和由外向内技术时发现对于年轻、体质量较轻的患者可以选择前内侧入路重建前交叉韧带,而对于前交叉韧带翻修的患者则选择由外向内技术更好。da Silva等[72]通过对改良版经胫骨隧道入路技术与其他技术重建前交叉韧带股骨隧道的研究,发现改良版经胫骨隧道入路技术对解剖重建股骨隧道效果不明显,但总体上仍优于传统经胫骨隧道入路技术,而由外向内技术钻取的股骨隧道更加靠近解剖位置。Gadikota等[73]研究得出前交叉韧带后外侧束经辅助内侧入路技术和由外向内技术重建后,覆盖面积比经胫骨隧道入路技术大,此外,辅助内侧入路技术和由外向内技术创建的隧道中心比经胫骨隧道入路技术隧道中心更接近原始前交叉韧带足印中心,经胫骨隧道入路技术中股骨隧道出口的并发症高于由外向内技术和经胫骨隧道入路技术。 2.4.2 内侧副韧带损伤的手术方式选择 内侧副韧带损伤一般分为止点损伤和中部损伤。在内侧副韧带中部损伤较轻的患者中,无论是内侧副韧带浅层还是深层损伤,均可采取断端修补,同时予以减张缝合较少张力;如果损伤较严重,可以采取半肌腱转位技术,在内侧副韧带的起止点处加强固定,防止固定不牢靠。内侧副韧带止点损伤的部位一般以股骨止点处损伤多见,如果该损伤处理不当,则会影响关节稳定性,继发创伤性关节炎[74]。目前内侧副韧带止点损伤大多采用带线锚定缝合治疗,即在股骨内收肌结节上方2 cm沿关节内侧至关节线下5 mm做一切口,逐层切开,用带线锚钉在韧带断裂处垂直打入,拧入深度2.0-3.0 mm,利用钉尾的不可吸收缝合线对韧带进行缝合打结,韧带损伤程度严重的用2枚锚钉。明文义等[74]对27例膝关节内侧副韧带股骨止点处Ⅲ级损伤的患者采用带线锚定缝合技术进行治疗,修复后随访6-18个月,恢复效果均良好,Lysholm 评分由修复前的(33.8±3.6)分提高至 (87.6±8.1)分。张中兴等[75]对24例膝关节内侧副韧带股骨止点处Ⅲ级损伤的患者用带线锚钉缝合治疗,修复后随访时间平均14.2个月,Lysholm评分由修复前的(58.4±7.1)分提高至修复后的(87.4±8.1)分,修复后恢复效果满意。张明勇等[76]对20例膝关节内侧副韧带止点损伤的患者进行治疗,修复后平均随访12个月,Lysholm评分由修复前(62.3±3.4)分提高至修复后(93.6±2.8)分,修复后患者均未出现不适,效果满意。刘敏等[77]用同样的方法对35例内侧副韧带止点损伤的患者进行治疗, Lysholm评分修复前为(54.5±6.3)分,修复后1年为(88.1±4.2)分。牛海明[78]对23例内侧副韧带止点损伤的患者进行治疗,修复后依据Lysholm评分得出手术优良率为91%。杨晓明等[79]治疗57例膝关节内侧副韧带止点损伤的患者,Lysholm评分由修复前(67.62±2.31)分提高至修复后的(97.10±1.94)分,国际膝部文件委员会主观评分(International Knee Documentation Committee,IKDC)由修复前的(42.48± 7.45)分提高至修复后的(87.27±2.16)分,修复后膝关节外翻稳定性正常,膝关节功能显著增高。 此外,Dong等[80]提出了“三角矢量重建内侧副韧带”的方法,该方法是在胫骨平台前下方4.5 cm和后下方2.5 cm做一骨道,将移植物从胫骨前下方拉至后下方,最后在股骨内侧髁后上方固定,形似三角;前方力臂和后方力臂分别模拟内侧副韧带浅层前束和内侧副韧带浅层后束、后斜韧带的功能,该方法较Borden等[81]提出双束平行重建内侧副韧带浅层的方法能更好的解决膝关节外旋不稳的问题。蔡国栋等[82]提出用骨-髌腱-骨重建内侧副韧带,在临床观察中膝关节外翻稳定和旋转稳定良好,效果满意。 2.4.3 前交叉韧带合并内侧副韧带损伤急性期的手术治疗 Ateschrang等[83]对前交叉韧带断裂合并内侧副韧带Ⅱ级或Ⅲ级(Fettohe和Marshall分型)损伤处于急性期(伤后14 d)的患者予以手术治疗,对前交叉韧带损伤予以关节镜下前交叉韧带单束重建,而内侧副韧带损伤予以新型微创韧带支撑技术,即在屈膝20°位在胫骨鹅足肌腱附着点上方做一切口,将直径1.5 mm可吸收缝合线从该切口引入,在股骨内髁膝关节活动中心处拧入直径3.5 mm皮质骨螺钉(利用原先前交叉韧带重建所做的股骨内髁处的切口),将可吸收缝合线绕过股骨侧螺钉,在胫骨原内侧副韧带浅层止点处拧入皮质骨螺钉,将可吸收缝合线在胫骨螺钉处打结,修复后予以支具制动。在修复后的随访和影像学评估中,内侧关节间隙在屈曲20°位时从修复前的(2.5±0.5)(2-3) mm减少为修复后的(0.1±0.2)(0-1) mm,内侧关节的稳定性在屈曲0°时与健侧比较在修复后1年为平均1.1 mm;在膝关节屈曲30°和90°时,与健侧比较患侧没有出现内旋和外旋不稳;在矢状位稳定性的评估中,修复后1年胫骨的平均前移距离为2.6 mm(1-4 mm),Lysholm评分平均为89.1分。董江涛等[84]将急性内侧副韧带Ⅲ级损伤合并前交叉韧带损伤的患者分别进行内侧副韧带解剖重建和内侧副韧带三角矢量重建,所有患者均进行前交叉韧带单束解剖重建,2组的膝关节内侧间隙重建后显著减少,在随访中内侧副韧带三角矢量重建组比内侧副韧带解剖重建组膝关节前内侧旋转不稳的发生率低,IKDC客观评分中内侧副韧带解剖重建组和内侧副韧带三角矢量重建组分别有87.5%和90.6%的患者达到正常或者接近正常水平,2组IKDC客观评分重建后均显著改善;IKDC活动评分中2组患者在重建后均能达到满意的伸直和屈曲水平。对于新鲜合并伤,作者建议对内侧副韧带损伤应用Hughsyon分型进行评估,内侧副韧带Ⅰ型和Ⅱ型损伤建议保守治疗4-6周,予外翻应力试验评估,外翻应力试验阳性则同期行内侧副韧带和前交叉韧带手术治疗,外翻应力试验阴性,则单纯行前交叉韧带重建手术,二期手术可降低感染概率,同时予患肢消肿及炎症消退时间,有利于术中操作及术后康复。 2.4.4 前交叉韧带合并内侧副韧带损伤陈旧期的手术治疗 唐继仁等[85]对51例前交叉韧带合并内侧副韧带陈旧性损伤(伤后5-40周)的患者进行手术治疗,对损伤的前交叉韧带取股薄肌、半腱肌进行关节镜下单束重建,然后在膝关节内髁处做一个6 cm切口,将预留移植肌腱的至股骨内髁以重建内侧副韧带,在内髁处钻取 4 mm骨道,用引线技术肌将腱拉入骨道,用Intrafix(美国Johnson公司)固定,发现Lysholm评分从重建前的(55.81±4.82)分增加至重建后的(93.22±3.90)分,IKDC评分从重建前的(63.12±3.91)分增加至重建后的(94.11±5.50)分,重建后效果满意。董江涛等[84]对29例晚期内侧副韧带合并前交叉韧带损伤(损伤时间> 12周)的患者用异体韧带双束重建技术治疗前交叉韧带损伤,用三角矢量重建技术重建内侧副韧带,重建后IKDC评分有87%(21/29)的治疗效果达到优良,Lysholm评分从重建前的(48.4±3.4)分增加至重建后的(87.1±2.2)分,晚期进行手术恢复效果满意。对于陈旧性的合并损伤,建议立即行前交叉韧带韧带重建,内侧副韧带损伤可通过外翻应力实验进行评估,若外翻应力试验阴性,可保守治疗,若外翻应力试验阳性,则考虑手术治疗。"

| [1] Roach CJ, Haley CA, Cameron KL, et al. The epidemiology of medial collateral ligament sprains in young athletes. Am J Sports Med. 2014;42(5):1103-1109. [2] Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am. 1979;61(1):56-62. [3] Phisitkul P, James SL, Wolf BR, et al. MCL injuries of the knee: current concepts review. Iowa Orthop J. 2006;26:77-90. [4] Schein A, Matcuk G, Patel D, et al. Structure and function, injury, pathology, and treatment of the medial collateral ligament of the knee. Emerg Radiol. 2012;19(6):489-498. [5] Lundquist RB, Matcuk GR Jr, Schein AJ, et al. Posteromedial Corner of the Knee: The Neglected Corner. Radiographics. 2015; 35(4):1123-1137. [6] Sasaki N, Ishibashi Y, Tsuda E, et al. The femoral insertion of the anterior cruciate ligament: discrepancy between macroscopic and histological observations. Arthroscopy. 2012;28(8):1135-1146. [7] Iwahashi T, Shino K, Nakata K, et al. Direct anterior cruciate ligament insertion to the femur assessed by histology and 3-dimensional volume-rendered computed tomography. Arthroscopy. 2010;26(9 Suppl):S13-20. [8] ?migielski R, Zdanowicz U, Drwi?ga M, et al. Ribbon like appearance of the midsubstance fibres of the anterior cruciate ligament close to its femoral insertion site: a cadaveric study including 111 knees. Knee Surg Sports Traumatol Arthrosc. 2015; 23(11):3143-3150. [9] Mochizuki T, Muneta T, Nagase T, et al. Cadaveric knee observation study for describing anatomic femoral tunnel placement for two-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2006;22(4):356-361. [10] Siebold R, Ellert T, Metz S, et al. Tibial insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry, arthroscopic landmarks, and orientation model for bone tunnel placement. Arthroscopy. 2008;24(2): 154-161. [11] 韦钊岚,李富明,徐攀峰,等.经前内侧入路关节镜下行前交叉韧带单束解剖重建术的临床应用[J].微创医学,2013,8(5):608-610.[12] 单云官,王连鹏,张金波,等.股胫关节面的形态与扣锁机制的解剖学基础[J].中国临床解剖学杂志,2007,25(6):650-652.[13] Kim HY, Kim KJ, Yang DS, et al. Screw-Home Movement of the Tibiofemoral Joint during Normal Gait: Three-Dimensional Analysis. Clin Orthop Surg. 2015;7(3):303-309. [14] 王海鹏,王友.膝内侧副韧带功能解剖和生物力学特性的研究进展[J].医用生物力学,2007,22(4):412-416.[15] Saigo T, Tajima G, Kikuchi S, et al. Morphology of the Insertions of the Superficial Medial Collateral Ligament and Posterior Oblique Ligament Using 3-Dimensional Computed Tomography: A Cadaveric Study. Arthroscopy. 2017;33(2):400-407. [16] 姚杰,樊瑜波,张明,等.前交叉韧带损伤的继发性生物力学影响[J].力学学报,2010,42(1):102-108.[17] Kennedy JC, Hawkins RJ, Willis RB, et al. Tension studies of human knee ligaments. Yield point, ultimate failure, and disruption of the cruciate and tibial collateral ligaments. J Bone Joint Surg Am. 1976;58(3):350-355. [18] Robinson JR, Bull AM, Amis AA. Structural properties of the medial collateral ligament complex of the human knee. J Biomech. 2005;38(5):1067-1074. [19] Ellsasser JC, Reynolds FC, Omohundro JR. The non-operative treatment of collateral ligament injuries of the knee in professional football players. An analysis of seventy-four injuries treated non-operatively and twenty-four injuries treated surgically. J Bone Joint Surg Am. 1974;56(6):1185-1190. [20] Gardiner JC, Weiss JA, Rosenberg TD. Strain in the human medial collateral ligament during valgus loading of the knee. Clin Orthop Relat Res. 2001(391):266-274. [21] Gardiner JC, Weiss JA. Subject-specific finite element analysis of the human medial collateral ligament during valgus knee loading. J Orthop Res. 2003;21(6):1098-1106. [22] Kawada T, Abe T, Yamamoto K, et al. Analysis of strain distribution in the medial collateral ligament using a photoelastic coating method. Med Eng Phys. 1999;21(5):279-291. [23] Nakamura N, Horibe S, Toritsuka Y, et al. Acute grade III medial collateral ligament injury of the knee associated with anterior cruciate ligament tear. The usefulness of magnetic resonance imaging in determining a treatment regimen. Am J Sports Med. 2003;31(2): 261-267. [24] Bergfeld J. Symposium: functional rehabilitation of isolated medial collateral ligament sprains. First-, second-, and third-degree sprains. Am J Sports Med. 1979;7(3):207-209. [25] Matsumoto H, Suda Y, Otani T, et al. Roles of the anterior cruciate ligament and the medial collateral ligament in preventing valgus instability. J Orthop Sci. 2001;6(1):28-32. [26] Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res. 1978; (132):206-218. [27] Hughston JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Joint Surg Am. 1994;76(9):1328-1344. [28] Taketomi S, Uchiyama E, Nakagawa T, et al. Clinical features and injury patterns of medial collateral ligament tibial side avulsions: "wave sign" on magnetic resonance imaging is essential for diagnosis. Knee. 2014;21(6):1151-1155. d[29] Blanke F, Paul J, Haenle M, et al. Results of a New Treatment Concept for Concomitant Lesion of Medial Collateral Ligament in Patients with Rupture of Anterior Cruciate Ligament. J Knee Surg. 2017;30(7):652-658. [30] 许宏涛,董江涛,王娟,等.内侧副韧带合并前交叉韧带损伤的临床治疗策略[J].中国矫形外科杂志,2017,25(2):132-135.[31] Nagineni CN, Amiel D, Green MH, et al. Characterization of the intrinsic properties of the anterior cruciate and medial collateral ligament cells: an in vitro cell culture study. J Orthop Res. 1992;10(4): 465-475. [32] Woo SL, Inoue M, McGurk-Burleson E, et al. Treatment of the medial collateral ligament injury. II: Structure and function of canine knees in response to differing treatment regimens. Am J Sports Med. 1987;15(1):22-29. [33] Menetrey J, Laumonier T, Garavaglia G, et al. α-Smooth muscle actin and TGF-β receptor I expression in the healing rabbit medial collateral and anterior cruciate ligaments. Injury. 2011;42(8):735-741. [34] Tandogan NR, Kayaalp A. Surgical treatment of medial knee ligament injuries: current indications and techniques. EFORT Open Rev. 2017;1(2):27-33. [35] Lundberg M, Messner K. Long-term prognosis of isolated partial medial collateral ligament ruptures. A ten-year clinical and radiographic evaluation of a prospectively observed group of patients. Am J Sports Med. 1996;24(2):160-163. [36] Pressman A, Johnson DH. A review of ski injuries resulting in combined injury to the anterior cruciate ligament and medial collateral ligaments. Arthroscopy. 2003;19(2):194-202. [37] Ohno K, Pomaybo AS, Schmidt CC, et al. Healing of the medial collateral ligament after a combined medial collateral and anterior cruciate ligament injury and reconstruction of the anterior cruciate ligament: comparison of repair and nonrepair of medial collateral ligament tears in rabbits. J Orthop Res. 1995;13(3):442-449. [38] Shelbourne KD, Porter DA. Anterior cruciate ligament-medial collateral ligament injury: nonoperative management of medial collateral ligament tears with anterior cruciate ligament reconstruction. A preliminary report. Am J Sports Med. 1992;20(3): 283-286. [39] Ma CB, Papageogiou CD, Debski RE, et al. Interaction between the ACL graft and MCL in a combined ACL+MCL knee injury using a goat model. Acta Orthop Scand. 2000;71(4):387-393. [40] Abramowitch SD, Yagi M, Tsuda E, et al. The healing medial collateral ligament following a combined anterior cruciate and medial collateral ligament injury--a biomechanical study in a goat model. J Orthop Res. 2003;21(6):1124-1130. [41] Kanamori A, Sakane M, Zeminski J, et al. In-situ force in the medial and lateral structures of intact and ACL-deficient knees. J Orthop Sci. 2000;5(6):567-571. [42] Sakane M, Livesay GA, Fox RJ, et al. Relative contribution of the ACL, MCL, and bony contact to the anterior stability of the knee. Knee Surg Sports Traumatol Arthrosc. 1999;7(2):93-97. [43] Zhu J, Dong J, Marshall B, et al. Medial collateral ligament reconstruction is necessary to restore anterior stability with anterior cruciate and medial collateral ligament injury. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):550-557. [44] Fanelli GC, Edson CJ. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthroscopy. 2002;18(7): 703-714. [45] Frölke JP, Oskam J, Vierhout PA. Primary reconstruction of the medial collateral ligament in combined injury of the medial collateral and anterior cruciate ligaments. Short-term results. Knee Surg Sports Traumatol Arthrosc. 1998;6(2):103-106. [46] Edson CJ. Conservative and postoperative rehabilitation of isolated and combined injuries of the medial collateral ligament. Sports Med Arthrosc Rev. 2006;14(2):105-110. [47] Azar FM. Evaluation and treatment of chronic medial collateral ligament injuries of the knee. Sports Med Arthrosc Rev. 2006; 14(2):84-90. [48] Song EK, Kim SK, Lim HA, et al. Comparisons of tunnel-graft angle and tunnel length and position between transtibial and transportal techniques in anterior cruciate ligament reconstruction. Int Orthop. 2014;38(11):2357-2362. [49] Robin BN, Lubowitz JH. Disadvantages and advantages of transtibial technique for creating the anterior cruciate ligament femoral socket. J Knee Surg. 2014;27(5):327-330. [50] Araujo PHM, Asai S, Pinto MP, et al. The ACL Graft Inclination Angle Effects in In Situ Force. Arthroscopy. 2013;29:e40. [51] Wang H, Fleischli JE, Zheng NN. Transtibial versus anteromedial portal technique in single-bundle anterior cruciate ligament reconstruction: outcomes of knee joint kinematics during walking. Am J Sports Med. 2013;41(8):1847-1856. [52] Webster KE, Palazzolo SE, McClelland JA, et al. Tibial rotation during pivoting in anterior cruciate ligament reconstructed knees using a single bundle technique. Clin Biomech (Bristol, Avon). 2012;27(5):480-484. [53] Hofbauer M, Muller B, Murawski CD, et al. The concept of individualized anatomic anterior cruciate ligament (ACL) reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22(5): 979-986. [54] Rabuck SJ, Middleton KK, Maeda S, et al. Individualized anatomic anterior cruciate ligament reconstruction. Arthrosc Tech. 2012;1(1):e23-29. [55] Kopf S, Pombo MW, Szczodry M, et al. Size variability of the human anterior cruciate ligament insertion sites. Am J Sports Med. 2011;39(1):108-113. [56] Tang J, Thorhauer E, Marsh C, et al. Knee rotation influences the femoral tunnel angle measurement after anterior cruciate ligament reconstruction: a 3-dimensional computed tomography model study. Knee Surg Sports Traumatol Arthrosc. 2014;22(7):1505-1510. [57] Pearle AD, McAllister D, Howell SM. Rationale for Strategic Graft Placement in Anterior Cruciate Ligament Reconstruction: I. D. E. A. L. Femoral Tunnel Position. Am J Orthop. 2015;44(5):253-258. [58] Kopf S, Forsythe B, Wong AK, et al. Nonanatomic tunnel position in traditional transtibial single-bundle anterior cruciate ligament reconstruction evaluated by three-dimensional computed tomography. J Bone Joint Surg Am. 2010;92(6):1427-1431. [59] Takeda Y, Iwame T, Takasago T, et al. Comparison of tunnel orientation between transtibial and anteromedial portal techniques for anatomic double-bundle anterior cruciate ligament reconstruction using 3-dimensional computed tomography. Arthroscopy. 2013;29(2):195-204. [60] Tashiro Y, Okazaki K, Uemura M, et al. Comparison of transtibial and transportal techniques in drilling femoral tunnels during anterior cruciate ligament reconstruction using 3D-CAD models. Open Access J Sports Med. 2014;5:65-72. [61] de Abreu-e-Silva GM, Baumfeld DS, Bueno EL, et al. Clinical and three-dimensional computed tomographic comparison between ACL transportal versus ACL transtibial single-bundle reconstructions with hamstrings. Knee. 2014;21(6):1203-1209. [62] Venosa M, Delcogliano M, Padua R, et al. Femoral Tunnel Positioning in Anterior Cruciate Ligament Reconstruction: Anteromedial Portal versus Transtibial Technique-A Randomized Clinical Trial. Joints. 2017;5(1):34-38. [63] Shetty SM, Shetty V, Ballal A, et al. A radiological comparative study between transtibial & anteromedial portal drilling of femoral tunnel in single bundle anterior cruciate ligament reconstruction: A comparison of four angles. J Arthroscopy Joint Surg. 2016;3:22-27. [64] Sukur E, Akman YE, Senel A, et al. Comparing Transtibial and Anteromedial Drilling Techniques for Single-bundle Anterior Cruciate Ligament Reconstruction. Open Orthop J. 2016;10:481-489. [65] Liu A, Sun M, Ma C, et al. Clinical outcomes of transtibial versus anteromedial drilling techniques to prepare the femoral tunnel during anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2751-2759. [66] Kim JG, Wang JH, Lim HC, et al. Femoral graft bending angle and femoral tunnel geometry of transportal and outside-in techniques in anterior cruciate ligament reconstruction: an in vivo 3-dimensional computed tomography analysis. Arthroscopy. 2012;28(11):1682-1694. [67] Harner CD, Honkamp NJ, Ranawat AS. Anteromedial portal technique for creating the anterior cruciate ligament femoral tunnel. Arthroscopy. 2008;24(1):113-115. [68] Holt M. Five-year results of single-incision arthroscopic anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 1999;27(3):390. [69] Pombo MW, Shen W, Fu FH. Anatomic double-bundle anterior cruciate ligament reconstruction: where are we today? Arthroscopy. 2008;24(10):1168-1177. [70] Tompkins M, Cosgrove CT, Milewski MD, et al. Anterior cruciate ligament reconstruction femoral tunnel characteristics using an accessory medial portal versus traditional transtibial drilling. Arthroscopy. 2013;29(3):550-555. [71] Burnham JM, Malempati CS, Carpiaux A, et al. Anatomic Femoral and Tibial Tunnel Placement During Anterior Cruciate Ligament Reconstruction: Anteromedial Portal All-Inside and Outside-In Techniques. Arthrosc Tech. 2017;6(2):e275-e282. [72] da Silva RR, Matos MA, Costa VCNB, et al. Tomographic Study of Femoral Positioning in Anterior Cruciate Ligament Reconstruction Using the Transtibial Technique. Knee Surg Relat Res. 2017;29(3):195-202. [73] Gadikota HR, Sim JA, Hosseini A, et al. The relationship between femoral tunnels created by the transtibial, anteromedial portal, and outside-in techniques and the anterior cruciate ligament footprint. Am J Sports Med. 2012;40(4):882-888. [74] 明文义,沈万祥,吴旭东,等.带线锚钉缝合固定治疗Ⅲ度膝关节内侧副韧带股骨髁止点处损伤[J].中医正骨,2013,25(1):53-55.[75] 张中兴,许峰,陈焕诗.带线锚钉治疗膝关节内侧副韧带止点Ⅲ度损伤[J].骨科,2014,5(3):140-142.[76] 张明勇,梁军,涂敏,等.带线锚钉治疗膝关节内侧副韧带止点断裂[J].中华创伤骨科杂志,2009,11(11):1092-1093.[77] 刘敏,杨国敬,林瑞新,等.带线锚钉治疗膝内侧副韧带止点撕脱损伤[J].实用骨科杂志,2010,16(1):29-31.[78] 牛海明.带线锚钉治疗膝内侧副韧带Ⅲ度损伤的临床观察[J].医学临床研究,2014,31(11):2260-2261.[79] 杨晓明,孙超,潘昭勋,等.锚钉缝线桥技术治疗膝关节内侧副韧带上止点损伤[J].中国矫形外科杂志,2017,25(24):2278-2281.[80] Dong JT, Chen BC, Men XQ, et al. Application of triangular vector to functionally reconstruct the medial collateral ligament with double-bundle allograft technique. Arthroscopy. 2012;28(10): 1445-1453. [81] Borden PS, Kantaras AT, Caborn DN. Medial collateral ligament reconstruction with allograft using a double-bundle technique. Arthroscopy. 2002;18(4):E19. [82] 蔡国栋,唐新元,王俊勤.关节镜下自体骨-髌腱-骨重建膝前交叉韧带[J].实用骨科杂志,2009,15(5):344-347.[83] Ateschrang A, Döbele S, Freude T, et al. Acute MCL and ACL injuries: first results of minimal-invasive MCL ligament bracing with combined ACL single-bundle reconstruction. Arch Orthop Trauma Surg. 2016;136(9):1265-1272. [84] 董江涛,王飞,陈百成,等.双束异体韧带三角形矢量重建内侧副韧带的临床研究[J].中华外科杂志,2011,49(12):1114-1118.[85] 唐继仁,吕帧贤,林世荣,等.关节镜下联合重建前交叉韧带与内侧副韧带陈旧性损伤[J].中国骨与关节损伤杂志,2016(s1):54-55. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [3] | Ji Zhixiang, Lan Changgong. Polymorphism of urate transporter in gout and its correlation with gout treatment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1290-1298. |
| [4] | Wan Ran, Shi Xu, Liu Jingsong, Wang Yansong. Research progress in the treatment of spinal cord injury with mesenchymal stem cell secretome [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1088-1095. |
| [5] | Jiao Hui, Zhang Yining, Song Yuqing, Lin Yu, Wang Xiuli. Advances in research and application of breast cancer organoids [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1122-1128. |
| [6] | Zhong Hehe, Sun Pengpeng, Sang Peng, Wu Shuhong, Liu Yi. Evaluation of knee stability after simulated reconstruction of the core ligament of the posterolateral complex [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 821-825. |
| [7] | Liu Shaohua, Zhou Guanming, Chen Xicong, Xiao Keming, Cai Jian, Liu Xiaofang. Influence of anterior cruciate ligament defect on the mid-term outcome of fixed-bearing unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 860-865. |
| [8] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [9] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [10] | Xie Chongxin, Zhang Lei. Comparison of knee degeneration after anterior cruciate ligament reconstruction with or without remnant preservation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 735-740. |
| [11] | Liu Xin, Yan Feihua, Hong Kunhao. Delaying cartilage degeneration by regulating the expression of aquaporins in rats with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 668-673. |
| [12] | Li Chenjie, Lü Linwei, Song Yang, Liu Jingna, Zhang Chunqiu. Measurement and statistical analysis of trabecular morphological parameters of titanium alloy peri-prosthesis under preload [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 516-520. |
| [13] | Ma Ziyue, Ju Xiaochen, Zhang Lei, Sun Rongxin. Tendon-bone healing in anterior cruciate ligament reconstruction with and without remnant preservation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 582-587. |
| [14] | Zhang Yu, Feng Shuo, Yang Zhi, Zhang Ye, Sun Jianning, An Lun, Chen Xiangyang. Three-dimensional gait of patients with developmental dysplasia of hip undergoing total hip arthroplasty with high hip center [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 350-355. |
| [15] | Wang Weigang, Yang Zhidong, Feng Zongquan, Wang Ding. A mid-term clinical follow-up of unicompartmental knee arthroplasty with fixed bearing [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 368-373. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||