Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (27): 4318-4323.doi: 10.3969/j.issn.2095-4344.2017.27.010
Previous Articles Next Articles
Treatment strategy for incision infection after internal fixation in the elderly patients with lumbar degenerative disease
Zhang Hai-jing1, Sun Xiang-jie2, Ma Hai-gang2, Zhou Zhuo1, Fang Xiu-tong3
- 1Operation Room, 3Department of Spinal Surgery, Beijing Shijitan Hospital Affiliated to Capital Medical University, Beijing 100038, China; 2Nuomanqi People’s Hospital, Tongliao 028300, Inner Mongolia Autonomous Region, China
-
Online:2017-09-28Published:2017-10-24 -
Contact:Fang Xiu-tong, Department of Spinal Surgery, Beijing Shijitan Hospital Affiliated to Capital Medical University, Beijing 100038, China -
About author:Zhang Hai-jing, Nurse-in-charge, Operation Room, Beijing Shijitan Hospital Affiliated to Capital Medical University, Beijing 100038, China
CLC Number:
Cite this article
Zhang Hai-jing, Sun Xiang-jie, Ma Hai-gang, Zhou Zhuo, Fang Xiu-tong. Treatment strategy for incision infection after internal fixation in the elderly patients with lumbar degenerative disease[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(27): 4318-4323.
share this article
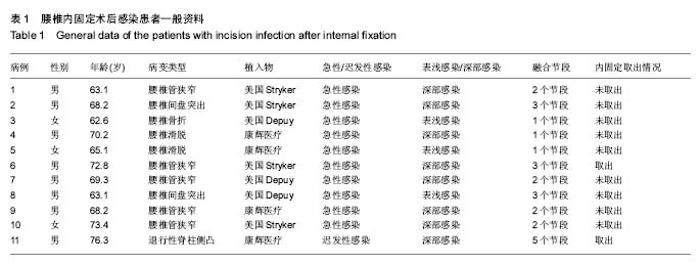
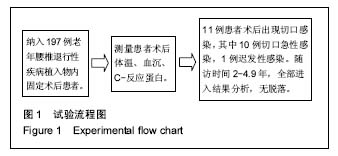
2.2 术后感染临床表现 197例老年腰椎退行性疾病内固定术后患者中,11例患者出现切口感染,其中10例切口急性感染,1例是迟发性感染。10例急性感染患者中,3例是切口表浅感染,7例是深部感染。急性感染的临床表现包括:切口渗液(10/10),切口局部疼痛(8/10),体温增高(9/10)。治疗方案给予细菌培养和药敏实验,同时静滴抗生素,感染局部清创放置闭合引流冲洗,除了1例患者取出内固定,其余患者均未取出内固定。1例迟发性感染患者临床表现包括切口局部疼痛、切口渗液及间断性发热。 2.3 术后感染患者一般资料 197例老年腰椎退行性疾病内固定术后患者,平均年龄(70.7±15.1)岁,其中49例患者融合范围为1个节段,134例患者融合范围为2个节段,14例患者融合范围为3个或者3个以上节段;后外侧融合为95例,椎间融合102例。 11例患者术后出现切口感染,平均年龄为(71.1±9.1)岁,10例切口急性感染(9.7±2.9) d,1例是迟发性感染(术后47 d出现),见表1。10例急性感染患者中,3例是切口表浅感染,7例是深部感染。老年腰椎退行性疾病患者内固定术后感染率为 5.6%(11/197)。2例患者融合范围为1个节段(均为椎间融合);6例患者融合范围为2个节段,其中4例为椎间融合,2例为后外侧融合;2例患者融合范围为3个节段,其中1例为后外侧融合,1例为椎间融合;1例患者融合范围为5个节段,为后外侧融合;融合材料均是自体骨或者异体骨。"
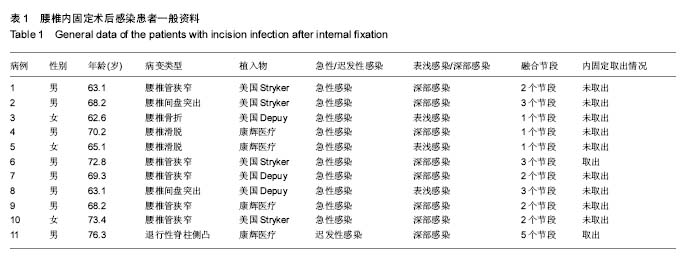
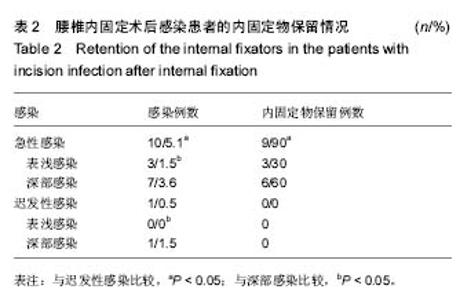
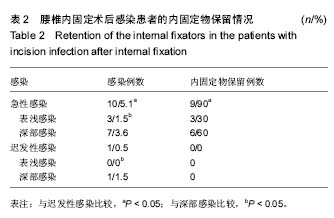
2.4 术后感染处理 切口急性表浅感染患者的处理是局部清创引流或清创后放置负压吸引,同时行细菌培养及药物敏感实验,3例切口急性表浅感染患者均治愈。7例切口急性深部感染患者的治疗行血培养检查,渗出物或者超声引导下感染区域穿刺行病原体培养,静滴光谱抗生素和万古霉素,如果患者体温升高持续不退,同时伴有切口渗出液及流脓,应立即进入手术室行切口彻底清创,保留内固定物,清创坏死组织和植骨材料,将坏死组织及渗出物培养,冲洗枪含有抗生素10 L盐水冲洗感染伤口,放置闭合冲洗管,逐层缝合切口。术后根据培养结果,选择敏感抗生素静滴4-6周,继续口服抗生素2-6周。闭合冲洗管放置三至四周,如果连续2次培养冲洗管引出液体阴性,可以拔出冲洗管。只有1例患者清创2次,持续发热,给予清除内固定物,彻底清除,感染控制,其余9例患者均保留内固定物。 1例迟发性感染患者为迟发性深部感染,给予取出内固定器械,彻底清创,放置闭合冲洗管,冲洗2周,拔除引流管治愈,术中探查无假关节形成。 术后切口感染患者中,深部感染的发生率明显高于表浅感染(P < 0.05),急性感染明显高于迟发性感染(P < 0.05),见表2。表浅感染的治疗原则无争议。切口急性深部感染与迟发性感染治疗方案并不相同,急性深部感染往往可以保留内固定器械,而迟发性感染往往要取出内固定器械。 11例切口感染患者中,4例为单一细菌感染,其中1例患者为金黄色葡萄球菌感染,3例为耐药金黄色葡萄球菌感染;3例为多种细菌混合感染,分别为大肠埃希菌和鲍曼不动杆菌,铜绿假单胞菌和粪肠球菌,产气肠杆菌和大肠埃希菌;4例感染患者未检测出细菌。 11例感染患者均行渗出物培养,并做药敏实验,根据感染科专家给予指导意见,结合培养结果,表浅感染一般选择敏感抗生素静滴2周,2周后继续口服抗生素2-4周;深部感染根据培养结果,选择敏感抗生素静滴4-6周,4-6周后继续口服抗生素2-6周。 "
| [1] Gopinathan P. Lumbar spinal canal stenosis-special features. J Orthop. 2015;12(3):123-125. [2] 史建刚,贾连顺,袁文,等.腰骶神经损害致马尾神经综合征的临床分期及早期诊断[J]. 中国矫形外科杂志,2005,13(7):491-493.[3] 赵慧毅,梅芳瑞,叶欣,等.腰椎管狭窄症的手术减压与内固定选择(259例临床分析)[J].中国脊柱脊髓杂志,2003,13(1):18-21.[4] 刘玉军,李学民,朱瑜琪. 闭式抗生素灌洗治疗腰椎间盘术后椎间隙感染的效果[J]. 中国矫形外科杂志,2007,15(7):554-556.[5] Mok JM, Pekmezci M, Piper SL, et al. Use of C-reactive protein after spinal surgery. Spine. 2008;33:415-421.[6] Hong HS, Chang MC, Liu CL, et al. Is aggressive surgery necessary for acute postoperative deep spinal wound infection? Spine. 2008;33: 2473-2478.[7] Kim JI, Suh KT, Kim SJ, et al. Implant removal for the management of infection after instrumented spinal fusion. J Spinal Disord Tech. 2010;23: 258-265.[8] Rayes M, Colen CB, Bahqat DA, et al. Safety of instrumentation in patients with spinal infection. J Neurosurg Spine. 2010;12: 647-659.[9] Sierra-Hoffman M, Jinadatha C, Carpenter JL, et al. MD-Postoperative Instrumented Spine Infections:A Retrospective Review. South Med J. 2010;1(103):25-30.[10] Turnbull F. Postoperative in?ammatory disease of lumbar discs.J Neurosurg,1953,10:469-473.[11] Rihn JA, Lee JY, Ward WT. Infection after the surgical treatment of adolescent idiopathic scoliosis: evaluation of the diagnosis, treatment, and impact on clinical outcomes. Spine. 2008;33: 289-294. [12] Kanafani ZA, Dakdouki GK, El-Dbouni O, et al. Surgical site infections following spinal surgery at a tertiary care center in Lebanon: incidence, microbiology, and risk factors. Scand J Infect Dis. 2006;38: 589-592. [13] 刘少强,齐强,刘宁,等.脊柱术后耐甲氧西林金黄色葡萄球菌感染的治疗-附8例报告[J]. 中国脊柱脊髓杂志,2014,24(2):164-167.[14] Sasso RC, Garrido BJ. Postoperative spinal wound infections. J Am Acad Orthop Surg. 2008;16:330-337.[15] An HS, Seldomridge JA. Spinal infections: diagnostic tests and imaging studies. Clin Orthop Relat Res. 2006;444:27-33.[16] Pull ter Gunne AF, Mohamed AS, Skolasky RL,et al. The presentation, incidence, etiology, and treatmentof surgical site infections after spinal surgery. Spine. 2010;35:1323-1328.[17] Enoch DA,Cargill JS, Laing R.Value of CT-guided biopsy in the diagnosis of septic discitis. J Clin Pathol. 2008;6:750–753.[18] Chaudhary SB, Vives MJ, Basra SK. Postoperative spinal wound infections and postprocedural discitis. J Spinal Cord Med. 2007;30:441-451.[19] Mok JM, Guillaume TJ, Talu U, et al. Clinical outcome of deep wound infection after instrumented posterior spinal fusion: a matched cohort analysis. Spine. 2009;34:578-583.[20] Collins I, Wilson-MacDonald J, Chami G, et al. The diagnosis and management of infection following instrumented spinal fusion. Eur Spine J. 2008;17:445-450.[21] Mehbod AA, Ogilvie JW, Pinto MR,et al. Postoperative deep infections in adults after spinal fusion: management with vacuum-assisted wound closure.J Spinal Disord Tech. 2005; 18:14-17.[22] Akins PT, Harris J, Alvarez JL, et al. Risk factors associated with 30-day readmissions after instrumented spine surgery in 14,939 patients. Spine (PhilaPa 1976). 2015;40:1022-1032.[23] Bydon M, Macki M, De la Garza-Ramos R, et al. Smoking as an independent predictor of reoperation after lumbar laminectomy: a study of 500 cases. J Neurosurg Spine. 2015;22:288-293.[24] Lim S, Edelstein AI, Patel AA, et al. Risk factors for postoperative infections following single level lumbar fusion surgery. Spine (Phila Pa 1976). 2014;40:1022-1032.[25] Chahoud J, Kanafani Z, Kanj SS. Surgical site infections following spine surgery: eliminating the controversies in the diagnosis. Front Med(Lausanne). 2014;1:7.[26] Chiang HY, Herwaldt LA, Blevins AE, et al. Effectiveness of local vancomycin powder to decrease surgical site infections: a meta-analysis. Spine J. 2014;14:397-407.[27] Srinivasan D, La Marca F, Than KD, et al. Perioperative characteristics and complications in obese patients undergoing anterior cervical fusion surgery. J Clin Neurosci. 2014;21:1159-1162.[28] Tetreault L, Nouri A, Singh A, et al. An assessment of the key predictors of perioperative complications in patients with cervical spondylotic myelopathy undergoing surgical treatment: results from a survey of 916 AO Spine International Members. World Neurosurg. 2015;83:679-690.[29] Liu X, Wang Y, Qiu G, et al. A systematic review with meta-analysis of posterior interbody fusion versus posterolateral fusion in lumbar spondylolisthesis. Eur Spine J. 2014;23:43-56.[30] Maruo K, Berven SH. Outcome and treatment of postoperative spine surgical site infections: predictors of treatment success and failure. J Orthop Sci. 2014;19: 398-404.[31] Calvert G, May LA, Theiss S. Use of permanently placed metal expandable cages for vertebral body reconstruction in the surgical treatment of spondylodiscitis. Orthopedics. 2014;37:e536-542.[32] Eder C, Schenk S, Trifinopoulos J, et al. Does intrawound application of vancomycin influence bone healing in spinal surgery? Eur Spine J. 2016;25(4):1021-1028.[33] Zebala LP, Chuntarapas T, Kelly MP, et al. Intrawound vancomycin powder eradicates surgical wound contamination: an in vivo rabbit study. J Bone Joint Surg. 2014;96:46-51. [34] Chiang HY, Herwaldt LA, Blevins AE, et al. Effectiveness of local vancomycin powder to decrease surgical site infections: a meta-analysis. Spine J. 2014;14(3):397-407. [35] Tomov M, Mitsunaga L, Durbin-Johnson B, et al. Reducing surgical site infection in spinal surgery with betadine irrigation and intrawound vancomycin powder. Spine. 2015;40:491-499. [36] Ghobrial GM, Thakkar V, Andrews E, et al. Intraoperative vancomycin use in spinal surgery: single institution experience and microbial trends. Spine. 2014;39:550-555. [37] Bakhsheshian J, Dahdaleh NS, Lam SK, et al. The use of vancomycin powder in modern spine surgery: systematic review and meta-analysis of the clinical evidence. World Neurosurgery. 2015;83:816-823. [38] Hill BW, Emohare O, Song B, et al. The use of vancomycin powder reduces surgical reoperation in posterior instrumented and noninstrumented spinal surgery. Acta neurochirurgica. 2014;156:749-754. [39] Theologis AA, Demirkiran G, Callahan M, et al. Local intrawound vancomycin powder decreases the risk of surgical site infections in complex adult deformity reconstruction: a cost analysis. Spine. 2014;39:1875-1880. [40] Martin JR, Adogwa O, Brown CR, et al. Experience with intrawound vancomycin powder for spinal deformity surgery. Spine. 2014;39:177-184. [41] Armaghani SJ, Menge TJ, Lovejoy SA, et al. Safety of topical vancomycin for pediatric spinal deformity: nontoxic serum levels with supratherapeutic drain levels. Spine. 2014,39: 1683-1687. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [3] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [4] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [5] | Song Jiawei, Yang Yongdong, Yu Xing, Yang Jizhou, Wang Fengxian, Qu Yi, Bi Lianyong. Mid-term effect of Isobar EVO non-fusion dynamic fixation in the treatment of adjacent segment disease after lumbar fusion [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 908-913. |
| [6] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [7] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [8] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [9] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [10] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [11] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [12] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [13] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| [14] | Guan Jian, Jia Yanfei, Zhang Baoxin , Zhao Guozhong. Application of 4D bioprinting in tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 446-455. |
| [15] | Huang Bo, Chen Mingxue, Peng Liqing, Luo Xujiang, Li Huo, Wang Hao, Tian Qinyu, Lu Xiaobo, Liu Shuyun, Guo Quanyi . Fabrication and biocompatibility of injectable gelatin-methacryloyl/cartilage-derived matrix particles composite hydrogel scaffold [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2600-2606. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||