Chinese Journal of Tissue Engineering Research ›› 2016, Vol. 20 ›› Issue (53): 8032-8042.doi: 10.3969/j.issn.2095-4344.2016.53.018
Previous Articles Next Articles
Autologous blood transfusion drainage versus conventional suction drainage in total knee arthroplasty: a meta-analysis of randomized controlled trials
Liu Jun1, Pan Jian-ke1, Hong Kun-hao2, Xie Hui1, Guo Da1, Xu Shu-chai1
- 1 Department of Orthopedics, Second Affiliated Hospital, Guangzhou University of Chinese Medicine (Guangdong Provincial Hospital of Traditional Chinese Medicine), Guangzhou 510120, Guangdong Province, China;2 Department of Orthopedics, Guangdong Second Traditional Chinese Medicine Hospital, Guangzhou 510095, Guangdong Province, China
-
Revised:2016-08-07Online:2016-12-23Published:2016-12-23 -
Contact:Xu Shu-chai, Chief physician, Master’s supervisor, Department of Orthopedics, Second Affiliated Hospital, Guangzhou University of Chinese Medicine (Guangdong Provincial Hospital of Traditional Chinese Medicine), Guangzhou 510120, Guangdong Province, China -
About author:Liu Jun, Chief physician, Professor, Doctoral supervisor, Department of Orthopedics, Second Affiliated Hospital, Guangzhou University of Chinese Medicine (Guangdong Provincial Hospital of Traditional Chinese Medicine), Guangzhou 510120, Guangdong Province, China -
Supported by:the National Natural Science Foundation of China, No. 81473698, 81273781; the Doctoral Scientific Research Fund Project of Higher Learning Schools of Education Ministry of China, No. 20124425110004; the Chinese Medicine Standardization Project of State Administration of Traditional Chinese Medicine, No. SATCM-2015-BZ115, SATCM-2015-BZ173; the Science and Technology Plan Program of Guangdong Province, No. 2011B031700027; a grant from Guangdong Provincial Department of Finance, No. [2014]157; the Science and Technology Research Program of Traditional Chinese Medicine of Guangdong Province Hospital of Traditional Chinese Medicine, No. YK2013B2N19, YN2015MS15
Cite this article
Liu Jun, Pan Jian-ke, Hong Kun-hao, Xie Hui, Guo Da, Xu Shu-chai. Autologous blood transfusion drainage versus conventional suction drainage in total knee arthroplasty: a meta-analysis of randomized controlled trials[J]. Chinese Journal of Tissue Engineering Research, 2016, 20(53): 8032-8042.
share this article
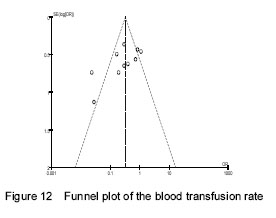
Study selection One hundred and eighty-one articles were retrieved in the study. Twelve studies[24-35], including 1 119 cases (556 cases for ABTD and 563 cases for CSD), met the inclusion criteria (Figure 1). We examined the references listed in these studies and in review articles, but did not find additional studies for evaluation."

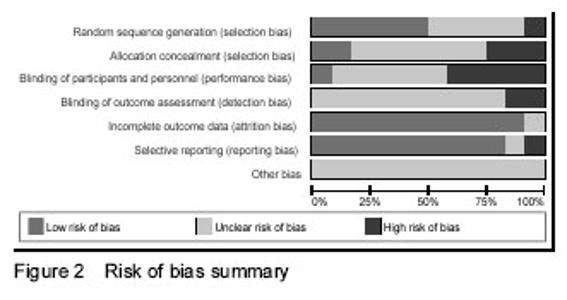
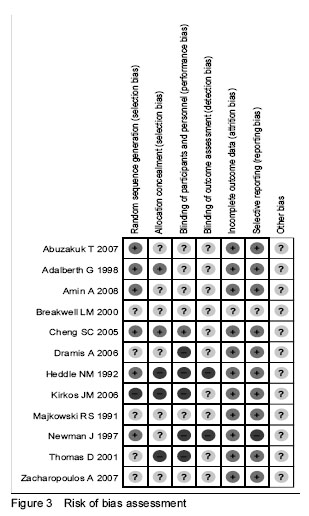
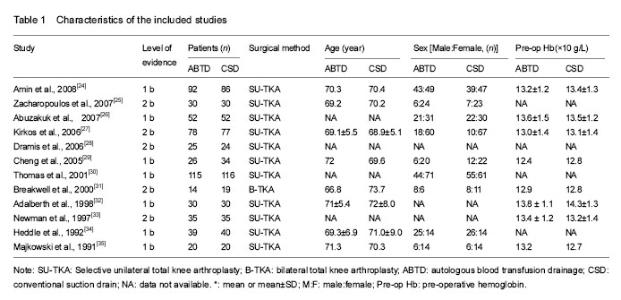
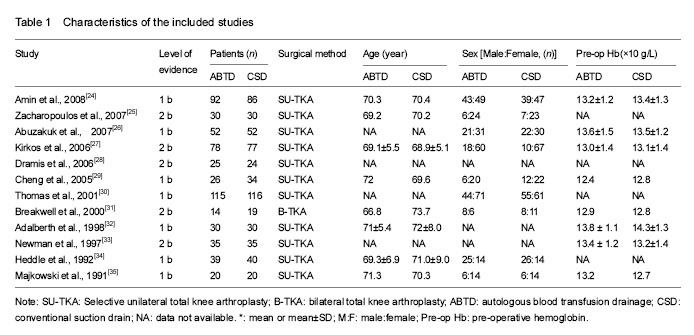
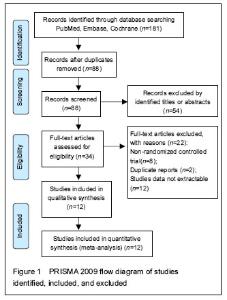
Characteristics of included studies The characteristics of the 12 included studies are summarized in Table 1. Among the included studies, there were 7 RCTs[24, 26, 29-30, 32, 34-35] with a 1b level of evidence and 5 RCTs[25, 27-28, 31, 33] with a 2b level of evidence. Patients in 11 studies[24-30, 32-35] underwent selective unilateral total knee replacement, while in the other study[31] they underwent bilateral total knee replacement. The methodological quality of all the included studies was evaluated by using the Cochrane risk of bias criteria (Figures 2, 3). Six studies[24, 26, 29, 32-34] mentioned the method of randomization. One study[27] used a quasi-randomization method. Five studies did not mention the method of randomization[25, 28, 30-31, 35]. Two studies[29, 32] mentioned the method of allocation concealment. One study[29] provided information about the blinding method. None of the 12 studies[24-35] mentioned the method of blinding the outcome assessment. Eleven studies[24-30, 32-35] reported the complete analysis. One study[33] was at high risk of selective reporting. The majority of the RCTs reviewed in this meta-analysis were moderate-quality studies. All the included studies claimed that the baseline data were comparable, including age, gender and pre-operative hemoglobin, as shown in Table 1."
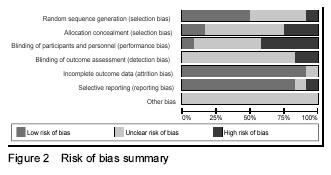

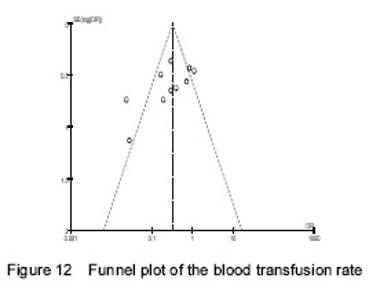
Primary outcomes of meta-analysis Blood transfusion rate Ten trials[24-26, 28-30, 32-35] compared the effects of ABTD and CSD according to changes in the number of patients requiring homologous blood transfusion. Because of the substantial heterogeneity (chi-square=34.04, P < 0.000 1; I²=74%), a random-effect model was used. The meta-analysis showed a significant beneficial effect of ABTD compared to CSD in reducing the blood transfusion rate (16.59% versus 37.47%, OR=0.28, 95%CI: 0.14-0.55, Z=3.67, P=0.000 2; Figure 4). Due to the marked heterogeneity within the evaluated blood transfusion rate, sensitivity analyses were conducted by excluding one study[33] with lower quality. This operation reduced the heterogeneity in the consistency of the trial results (I²=59%, P=0.01). The random-effects model of the meta-analysis also showed a significant beneficial effect of ABTD compared to CSD in reducing the blood transfusion rate (17.25% versus 34.03%, OR=0.37, 95%CI: 0.21-0.65, Z=3.42, P=0.000 6). Dropping any one of the studies did not alter the results that favored ABTD. Mean number of units transfused per patient Three trials[27, 32, 34], including 294 patients, reported the mean number of units transfused per patient (Figure 5). Because of the moderate heterogeneity (chi-square=3.40, P=0.18; I²=41%), a fixed-effects model was used. The meta-analysis showed a significant beneficial effect of ABTD compared to CSD in reducing the mean number of units transfused per patient (WMD=-0.56, 95%CI: -0.79- -0.33, Z=4.71, P < 0.000 01). Wound complications Data extracted from three studies[24, 30, 35] that assessed wound complications in 449 patients showed no significant difference between the ABTD and CSD groups (OR=0.98, 95%CI: 0.40-2.38; Z = 0.04, P=0.97). No significant heterogeneity was detected (P=0.66, I²=0%; Figure 6). Deep vein thrombosis Data extracted from four studies[24, 30, 32, 35] that assessed deep vein thrombosis in 509 patients showed no significant difference between the ABTD and CSD groups (OR=0.69, 95%CI: 0.21-2.24, Z=0.61, P=0.54). No significant heterogeneity was detected (P=0.64, I²=0%;Figure 7). "

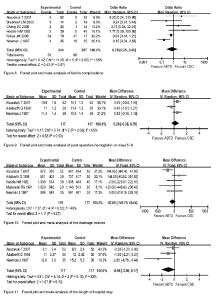
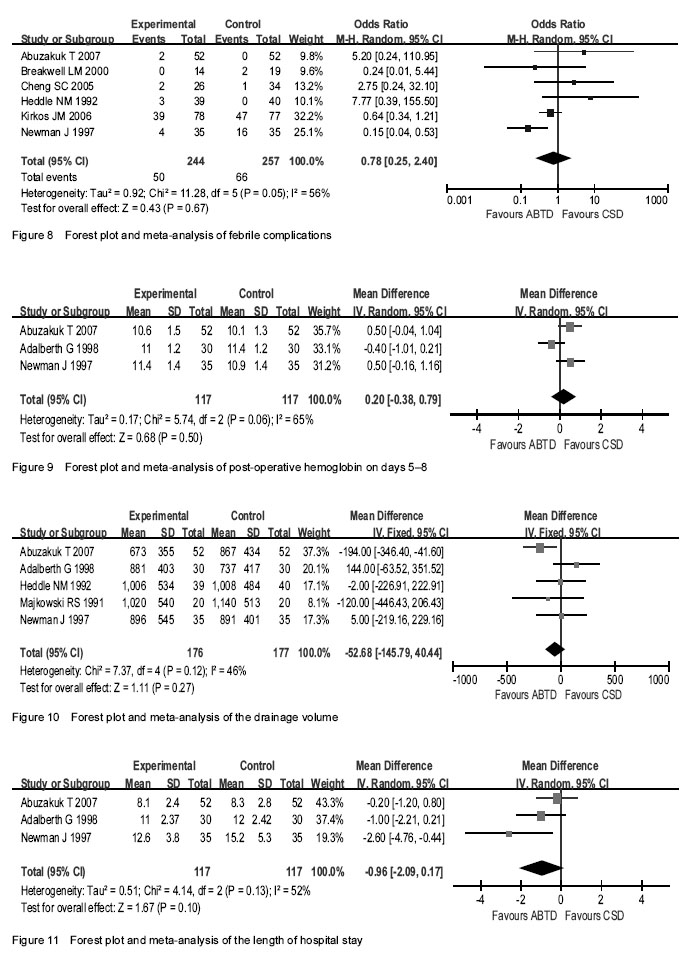
Secondary outcomes of meta-analysis Febrile complications Six trials[26-27, 29, 31, 33, 34] compared the effects of ABTD versus CSD with respect to changes in febrile complications. Because of the substantial heterogeneity (chi-square=11.28, P=0.05; I²=56%), a random-effects model was used. The meta-analysis showed no significant difference between the ABTD and CSD groups (OR=0.78, 95%CI: 0.25-2.40, Z=0.43, P=0.67; Figure 8). Due to the marked heterogeneity within the evaluated febrile complications, sensitivity analyses were conducted by excluding one study[33] with lower quality. This operation reduced the heterogeneity in the consistency of the trial results (I2=30%, P=0.22). The random-effects model of the meta-analysis also showed no significant difference between the ABTD and CSD groups (OR=1.21, 95%CI: 0.39-3.68, Z=0.33, P=0.74). Dropping any one of the studies did not alter the result that there was no significant difference between the two groups. Post-operative hemoglobin on days 5-8 Three studies[26, 32-33] reported post-operative hemoglobin on days 5-8. Among them, one study[26] reported hemoglobin on the fifth day post-operation, another study[32] reported hemoglobin on the eighth day post-operation, and the final study[33] reported hemoglobin on the seventh day post-operation. Because of the substantial heterogeneity (chi-square=5.74, P=0.06; I2=65%), a random-effects model was used. Pooling the data for the 234 patients in these three studies revealed no significant difference between the ABTD and CSD groups (WMD=0.20: -0.38-0.79, Z=0.68, P=0.50;Figure 9). Due to the marked heterogeneity within the evaluated post-operative hemoglobin at days 5-8, sensitivity analyses were conducted by excluding one study[32] with a high weight. No significant heterogeneity was then detected (P=1.00, I²=0%). The random-effects model of the meta-analysis showed a significant beneficial effect of CSD compared to ABTD in post-operative hemoglobin on days 5-8 (WMD=0.50, 95%CI: 0.08-0.92, Z=2.35, P=0.02). Drainage volume Five studies[26, 32-35] reported the post-operative drainage volume. Because of the moderate heterogeneity (chi-square=7.37, P=0.12; I2=46%), a fixed-effects model was used. The pooled data for the 353 patients in the five studies showed no significant difference between the ABTD and CSD groups (WMD=-52.68, 95%CI: -145.79-40.44, Z=1.11, P=0.27; Figure 10). Length of hospital stay Three trials[26, 32-33] compared the effects of ABTD and CSD with respect to changes in the length of hospital stay. Because of the substantial heterogeneity (chi-square=4.14, P=0.13; I2=52%), a random-effects model was used. The meta-analysis showed no significant difference between the ABTD and CSD groups for the length of hospital stay (WMD=-0.96, 95%CI: -2.09-0.17, Z=1.67, P=0.10; Figure 11). Due to the marked heterogeneity within the evaluated length of hospital stay, sensitivity analyses were conducted by excluding one study[33] with lower quality. After this operation, no significant heterogeneity was detected (P=0.32, I2=0%). The random-effects model of the meta-analysis also showed no significant difference between the ABTD and CSD groups for the hospital stay length (WMD=-0.52, 95%CI: -1.30-0.25, Z=1.33, P=0.18)."
| [1] Torres-Claramunt R, Hinarejos P, Perez-Prieto D, et al. Sealing of the intramedullar femoral canal in a TKA does not reduce postoperative blood loss: a randomized prospective study. Knee. 2014;21(4):853-857.[2] Bierbaum BE, Callaghan JJ, Galante JO, et al. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999;81(1):2-10.[3] Sehat KR, Evans RL, Newman JH. Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br. 2004;86(4): 561-565.[4] Keating EM, Meding JB, Faris PM, et al. Predictors of transfusion risk in elective knee surgery. Clin Orthop Relat Res. 1998;(357):50-59.[5] Adie S, Naylor JM, Harris IA. Cryotherapy after total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Arthroplasty. 2010;25(5):709-715.[6] Markar SR, Jones GG, Karthikesalingam A, et al. Transfusion drains versus suction drains in total knee replacement: meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2012;20(9):1766-1772.[7] Bidolegui F, Arce G, Lugones A, et al. Tranexamic acid reduces blood loss and transfusion in patients undergoing total knee arthroplasty without tourniquet: a prospective randomized controlled trial. Open Orthop J. 2014;8:250-254.[8] Tai TW, Chang CW, Yang CY. The Role of Drainage After Total Knee Arthroplasty: INTECH Open Access Publisher. 2012.[9] Drinkwater CJ, Neil MJ. Optimal timing of wound drain removal following total joint arthroplasty. J Arthroplasty. 1995;10(2):185-189.[10] Holt BT, Parks NL, Engh GA, et al. Comparison of closed-suction drainage and no drainage after primary total knee arthroplasty. Orthopedics. 1997;20(12): 1121-1125.[11] Martin A, Prenn M, Spiegel T, et al. Relevance of wound drainage in total knee arthroplasty-a prospective comparative study. Z Orthop Ihre Grenzgeb. 2004;142(1):46-50.[12] Kim YH, Cho SH, Kim RS. Drainage versus nondrainage in simultaneous bilateral total knee arthroplasties. Clin Orthop Relat Res. 1998(347): 188-193.[13] Gibbons CE, Solan MC, Ricketts DM, et al. Cryotherapy compared with Robert Jones bandage after total knee replacement: a prospective randomized trial. Int Orthop. 2001;25(4):250-252.[14] Pavelescu D, Mirea L, Grintescu I. Combined perioperative use of tranexamic acid with a postoperative reinfusion/autotransfusion drainage system dramatically decrease the allogenic transfusion needs in total knee arthroplasty (TKA). Euro J Anaesthesiol. 2014;31:103-104.[15] Kang DG, Khurana S, Baek JH, et al. Efficacy and safety using autotransfusion system with postoperative shed blood following total knee arthroplasty in haemophilia. Haemophilia. 2014;20(1):129-132.[16] Horstmann W, Kuipers B, Ohanis D, et al. Autologous re-transfusion drain compared with no drain in total knee arthroplasty: a randomised controlled trial. Blood Transfusion. 2014;12(SUPPL.1):s176-s181.[17] Thomassen BJW, Hollander PHC, Kaptijn HH, et al. Autologous wound drains have no effect on allogeneic blood transfusions in primary total hip and knee replacement: A three-arm randomised trial. Bone Joint J. 2014:765-771.[18] Cip J, Widemschek M, Benesch T, et al. Does single use of an autologous transfusion system in TKA reduce the need for allogenic blood? A prospective randomized trial general. Clin Orthop Relat Res. 2013:1319-1325.[19] Dobosz B, Dutka J, Dutka L, et al. Clinical and cost effectiveness-related aspects of retransfusion in total hip and knee arthroplasty. Ortopedia Trauma Rehabil. 2012;14(5):421-428.[20] Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009; 339:b2700.[21] Phillips B, Ball C, Sackett D, et al. Levels of evidence and grades of recommendation. Oxford Centre for Evidence-based Medicine Web site. 2009. [22] J H, S G. Cochrane handbook for systematic reviews of interventions. New York: Cochrane Collaboration, John Wiley and Sons. 2008.[23] Fan X, Lin T, Xu K, et al. Laparoendoscopic single-site nephrectomy compared with conventional laparoscopic nephrectomy: a systematic review and meta-analysis of comparative studies. Euro Urol. 2012;62(4):601-612.[24] Amin A, Watson A, Mangwani J, et al. A prospective randomised controlled trial of autologous retransfusion in total knee replacement. J Bone Joint Surg Br. 2008:451-454.[25] Zacharopoulos A, Apostolopoulos A, Kyriakidis A. The effectiveness of reinfusion after total knee replacement. A prospective randomised controlled study. Int Orthop. 2007;31(3):303-308.[26] Abuzakuk T, Senthil Kumar V, Shenava Y, et al. Autotransfusion drains in total knee replacement. Are they alternatives to homologous transfusion? Int Orthop. 2007;31(2):235-239.[27] Kirkos JM, Krystallis CT, Konstantinidis PA, et al. Postoperative re-perfusion of drained blood in patients undergoing total knee arthroplasty: is it effective and cost-efficient? Acta Orthopaedica Belgica. 2006;72(1):18-23.[28] Dramis A, Plewes J. Autologous blood transfusion after primary unilateral total knee replacement surgery. Acta Orthopaedica Belgica. 2006;72(1):15-17.[29] Cheng SC, Hung TS, Tse PY. Investigation of the use of drained blood reinfusion after total knee arthroplasty: a prospective randomised controlled study. J Orthopaedic Surg (Hong Kong). 2005: 120-124.[30] Thomas D, Wareham K, Cohen D, et al. Autologous blood transfusion in total knee replacement surgery. Br J Anaesth. 2001;86(5):669-673.[31] Breakwell LM, Getty CJM, Dobson P. The efficacy of autologous blood transfusion in bilateral total knee arthroplasty. Knee. 2000;145-147.[32] Adalberth G, Byström S, Kolstad K, et al. Postoperative drainage of knee arthroplasty is not necessary: a randomized study of 90 patients. Acta Orthop Scand. 1998:475-478.[33] Newman J, Bowers M, Murphy J. The clinical advantages of autologous transfusion a randomised, controlled study after knee replacement. J Bone Joint Surg Br. 1997;79(4):630-632.[34] Heddle NM, Brox WT, Klama LN, et al. A randomized trial on the efficacy of an autologous blood drainage and transfusion device in patients undergoing elective knee arthroplasty. Transfusion. 1992;32(8):742-746.[35] Majkowski RS, Currie IC, Newman JH. Postoperative collection and reinfusion of autologous blood in total knee arthroplasty. Ann R Coll Surg Engl. 1991: 381-384.[36] Lakshmanan P, Purushothaman B, Sharma A. Impact of reinfusion drains on hemoglobin level in total knee arthroplasty. Am J Orthop. 2010;39(2):70-74.[37] Sculco TP, Gallina J. Blood management experience: relationship between autologous blood donation and transfusion in orthopedic surgery. Orthopedics. 1999; 22(1 Suppl):129-134.[38] Bierbaum BE, Callaghan JJ, Galante JO, et al. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg. 1999;81(1):2-10.[39] Woolson ST, Wall WW. Autologous blood transfusion after total knee arthroplasty: a randomized, prospective study comparing predonated and postoperative salvage blood. J Arthrop. 2003;18(3): 243-249.[40] Munoz M, Kuhlmorgen B, Ariza D, et al. Which patients are more likely to benefit from postoperative shed blood salvage after unilateral total knee replacement? An analysis of 581 consecutive procedures. Vox Sang. 2007;92(2):136-141.[41] Andersson I, Tylman M, Bengtson JP, et al. Complement split products and pro-inflammatory cytokines in salvaged blood after hip and knee arthroplasty. Can J Anaesth. 2001;48(3):251-255.[42] Innerhofer P, Klingler A, Klimmer C, et al. Risk for postoperative infection after transfusion of white blood cell-filtered allogeneic or autologous blood components in orthopedic patients undergoing primary arthroplasty. Transfusion. 2005;45(1): 103-110.[43] Haien Z, Yong J, Baoan M, et al. Post-operative auto-transfusion in total hip or knee arthroplasty: a meta-analysis of randomized controlled trials. PLoS One. 2013;8(1):e55073. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Zhou Jihui, Li Xinzhi, Zhou You, Huang Wei, Chen Wenyao. Multiple problems in the selection of implants for patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1440-1445. |
| [3] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [4] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [5] | Zhong Hehe, Sun Pengpeng, Sang Peng, Wu Shuhong, Liu Yi. Evaluation of knee stability after simulated reconstruction of the core ligament of the posterolateral complex [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 821-825. |
| [6] | Liu Shaohua, Zhou Guanming, Chen Xicong, Xiao Keming, Cai Jian, Liu Xiaofang. Influence of anterior cruciate ligament defect on the mid-term outcome of fixed-bearing unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 860-865. |
| [7] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [8] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [9] | Liu Xin, Yan Feihua, Hong Kunhao. Delaying cartilage degeneration by regulating the expression of aquaporins in rats with knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 668-673. |
| [10] | Xie Chongxin, Zhang Lei. Comparison of knee degeneration after anterior cruciate ligament reconstruction with or without remnant preservation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 735-740. |
| [11] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [12] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| [13] | Chang Wenliao, Zhao Jie, Sun Xiaoliang, Wang Kun, Wu Guofeng, Zhou Jian, Li Shuxiang, Sun Han. Material selection, theoretical design and biomimetic function of artificial periosteum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 600-606. |
| [14] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [15] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||