Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (9): 2226-2235.doi: 10.12307/2026.600
Previous Articles Next Articles
Biomechanical performance of short-segment screw fixation combined with expandable polyetheretherketone vertebral body replacement in osteoporotic vertebrae
Chen Long1, 2, Wang Xiaozhen1, Xi Jintao1, Lu Qilin1
- 1Department of Spine Surgery, Wuhan Integrated Traditional Chinese and Western Medicine Hospital (Affiliated Hospital of Wuhan Sports University), Wuhan 430070, Hubei Province, China; 2Medical School, University of Rostock, Mecklenburg-Vorpommern 18057, Germany
-
Received:2024-12-23Accepted:2025-02-26Online:2026-03-28Published:2025-09-05 -
Contact:Lu Qilin, MD, Associate chief physician, Department of Spine Surgery, Wuhan Integrated Traditional Chinese and Western Medicine Hospital (Affiliated Hospital of Wuhan Sports University), Wuhan 430070, Hubei Province, China -
About author:Chen Long, MS, Attending physician, Department of Spine Surgery, Wuhan Integrated Traditional Chinese and Western Medicine Hospital (Affiliated Hospital of Wuhan Sports University), Wuhan 430070, Hubei Province, China; Medical School, University of Rostock, Mecklenburg-Vorpommern 18057, Germany -
Supported by:Hubei Natural Science Foundation, No. 2023AFB645 (to LQL); 2024 Hospital-level Project Affiliated Hospital of Wuhan Sports University, No. WTFY202401 (to CL)
CLC Number:
Cite this article
Chen Long, Wang Xiaozhen, Xi Jintao, Lu Qilin. Biomechanical performance of short-segment screw fixation combined with expandable polyetheretherketone vertebral body replacement in osteoporotic vertebrae[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2226-2235.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
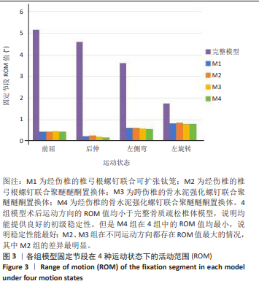
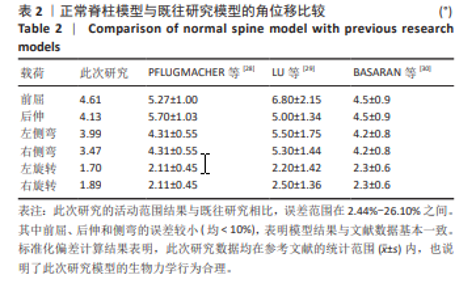
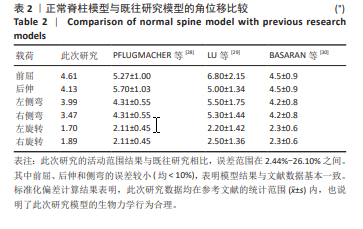
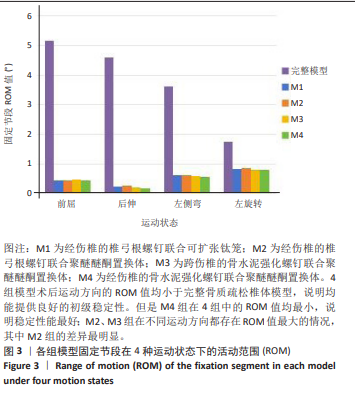
2.2 各模型T11-L1节段在4种运动状态下的ROM值 此次研究结果显示,4组模型术后T11-L1固定节段在4个运动状态下的ROM值较术前完整骨质疏松模型(5.17°,4.61°,3.63°,1.76°)均显著减小,说明4种内固定方式都能获得良好的初级稳定。M1组在4个运动状态下的ROM值(0.44°,0.23°,0.62°,0.83°)均小于M2组,分别降低了2.67%,10.36%,0.16%,2.92%,说明了M1组稳定性更高,尤其是后伸运动。比较M2、M3及M4组,M4组在前屈、后伸、左侧弯、左旋转4个运动方向的ROM值最小,分别为0.43°,0.18°,0.56°,0.78°;M3组在前屈状态下的ROM值最大,为0.46°,较M4组增加了7.26%;M2组在伸、左侧弯、左旋转状态下的ROM值最大,分别为0.25°,0.62°,0.86°,较M4组增加了37.91%,10.34%及9.31%。说明M2组的差异最明显,但相差不超过1°。具体见图3。"

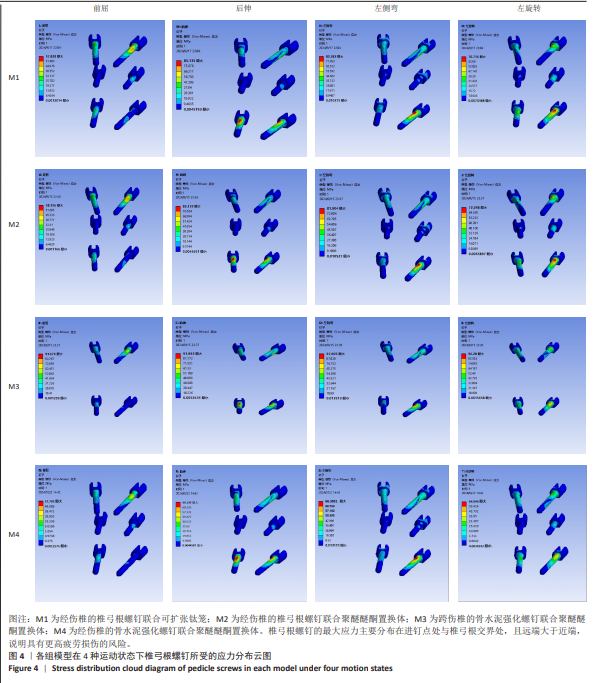
2.3 各模型在4种运动状态下内固定装置的应力情况 比较M1与M2组,M1组在4个运动状态下椎弓根螺钉(57.83,85.14,80.38,70.72 MPa)及连接棒(39.21,104.09,129.52,98.99 MPa)的最大应力值均较小,分别较M2组减少了(0.57%,1.17%,1.89%,2.24%)及(12.93%,2.19%,4.08%,2.96%)。但是,M1组置换体的最大应力值最大,在前屈、后伸、左侧弯、左旋转分别为29.60,29.17,29.31,27.29 MPa,较M2组分别增加了8.61%,13.53%,6.79%,6.36%。 在M2、M3、M4组中,M4组椎弓根螺钉的最大应力值在4个运动状态下均最小,分别为57.71,69.14,66.39,64.10 MPa。M3组椎弓根螺钉的最大应力值最大,较M4组分别增加了62.34%,33.06%,47.48%,50.21%;而M2组较M4组也分别增加了0.78%,24.58%,23.38%,12.80%。M3组椎弓根螺钉的最大应力值明显增加,预示着更高螺钉疲劳损伤的风险。而且椎弓根螺钉的最大应力值主要分布在进钉点与椎弓根螺钉的交界处,两端较中间螺钉承载了更多的应力。具体见图4。M4组连接棒的最大应力值在4个运动状态下最小,分别为37.35,102.28,127.54,94.99 MPa。M3组连接棒在前屈时的应力值最大(46.76 MPa),较M4组增加了25.18%;M2组连接棒在后伸(106.37 MPa)、左侧弯(134.81 MPa)、左旋转(101.92 MPa)时的应力值最大,分别较M4组增加了4.00%,5.70%,7.30%。M4组置换体的最大应力值在4个运动状态下也最小,分别为26.66,25.38,27.09,24.82 MPa。M2组则最大,较M4组分别增加了2.22%,1.23%,1.33%,3.35%。3组之间差异不明显。具体见图5。"
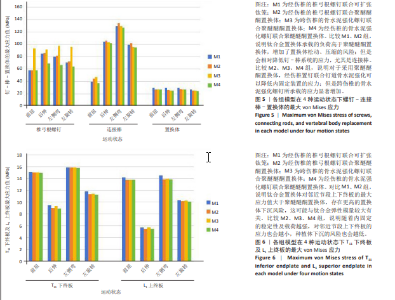
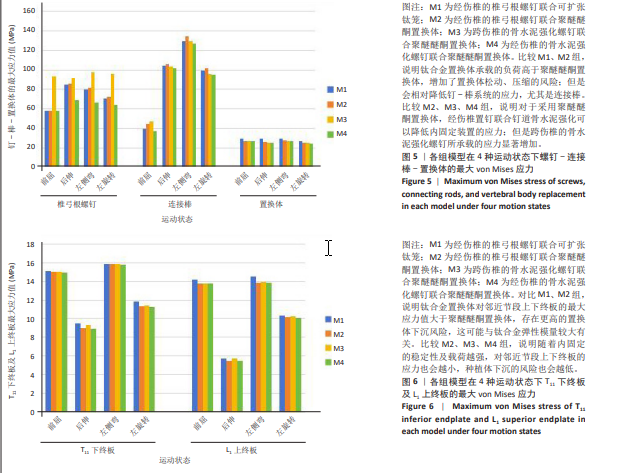
2.4 各模型在4种运动状态下T11下终板及L1上终板应力分布情况 比较M1与M2组,M1组T11下终板在前屈(15.14 MPa)、后伸(9.51 MPa)、左侧弯(15.87 MPa)、左旋转(11.82 MPa)时的应力值最大,较M2组分别增加了1.06%, 5.55%,0.28%,4.59%;同样,M1组L1上终板的最大应力值在4个运动状态下(14.19,5.70,14.52,10.33 MPa)也大于M2组,分别增加了3.18%,4.69%,4.60%,1.89%。说明M1组置换体对邻近节段终板的应力更大,发生种植体下沉的风险也会更高。 M2、M3、M4组之间比较时,M4组在4种运动状态下T11下终板的最大应力值(14.96,8.93,15.76,11.27 MPa)及L1上终板的最大应力值(13.74,5.43,13.86,10.04 MPa)均最小。M3组在4种运动状态下T11下终板及L1上终板的最大应力值均最大。其中,M3组T11下终板的最大应力值较M4组分别增加了0.17%,4.10%,0.51%,1.30%;而M3组L1上终板较M4组分别增加了0.34%,4.70%,0.25%,2.42%。说明M4组发生终板骨折、种植体下沉的风险最小,而M3组最大,但是3组差异并不显著。具体见图6。"
| [1] RAJASEKARAN S, KANNA RM, SCHNAKE KJ, et al. Osteoporotic thoracolumbar fractures-how are they different?-Classification and treatment algorithm. J Orthop Trauma. 2017;31(Suppl 4):S49-S56. [2] TSUJIO T, NAKAMURA H, TERAI H, et al. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: A prospective multi center study. Spine (Phila Pa 1976). 2011;36(15):1229-1235. [3] HOFFMANN J, PRESTON G, WHALEY J, et al. Vertebral Augmentation in Spine Surgery. J Am Acad Orthop Surg. 2023;31(10):477-489. [4] KASAPOVIC A, BORNEMANN R, PFLUGMACHER R, et al. Implants for Vertebral Body Replacement - Which Systems are Available and Have Become Established. Z Orthop Unfall. 2021;159(1):83-90. [5] TAKEUCHI T, YAMAGISHI K, KONISHI K, et al. Radiological Evaluation of Combined Anteroposterior Fusion with Vertebral Body Replacement Using a Minimally Invasive Lateral Approach for Osteoporotic Vertebral Fractures: Verification of Optimal Surgical Procedure. J Clin Med. 2022;11(3):629. [6] 苏佳灿, 刘昌胜, 张英泽, 等. 骨质疏松性椎体压缩骨折骨修复策略专家共识(2024版)[J]. 临床外科杂志,2024,41(3):476-482. [7] 徐宝山, 黎宁, 许海委, 等. 胸腰椎骨质疏松性椎体压缩骨折伴后凸畸形的分级手术策略[J]. 中华骨科杂志,2023,43(11):677-686. [8] 陈建, 李青青, 顾军, 等. 老年骨质疏松性胸腰段椎体骨折伴后凸畸形诊疗指南(2024版)[J]. 中华创伤杂志,2024,40(11):961-973. [9] SCHWENDER M, MOTOV S, RYANG YM, et al. Dorsal instrumentation with and without vertebral body replacement in patients with thoracolumbar osteoporotic fractures shows comparable outcome measures. Eur Spine J. 2022;31(5):1138-1146. [10] ALHASHASH M, SHOUSHA M. Minimally Invasive Short-Segment Anteroposterior Surgery for Thoracolumbar Osteoporotic Fractures with Canal Compromise: A Prospective Study with a Minimum 2-Year Follow-up. Asian Spine J. 2022;16(1):28-37. [11] 许勇, 官众, 李永霞, 等. 经伤椎和跨伤椎置钉内固定治疗胸腰椎骨折的早中期效果分析[J]. 中国组织工程研究,2020,24(12):1823-1828. [12] POKORNI AJ, TURBUCZ M, KISS RM, et al. Comparison of anterior column reconstruction techniques after en bloc spondylectomy: a finite element study. Sci Rep. 2023;13(1):18767. [13] DEML MC, MAZURET SEPULVEDA CA, ALBERS CE, et al. Anterior column reconstruction of the thoracolumbar spine with a new modular PEEK vertebral body replacement device: retrospective clinical and radiologic cohort analysis of 48 cases with 1.7-years follow-up. Eur Spine J. 2020; 29(12):3194-3202. [14] SCHWENDNER M, ILLE S, KIRSCHKE JS, et al. Clinical evaluation of vertebral body replacement of carbon fiber-reinforced polyetheretherketone in patients with tumor manifestation of the thoracic and lumbar spine. Acta Neurochir (Wien). 2023;165(4):897-904. [15] LIAO JC. Impact of osteoporosis on different type of short-segment posterior instrumentation for thoracolumbar burst fracture-a finite element analysis. World Neurosurg. 2020;139:e643-e651. [16] KANG S, PARK CH, JUNG H, et al. Analysis of the physiological load on lumbar vertebrae in patients with osteoporosis: a finite element study. Sci Rep. 2022;12(1):11001. [17] SHIRAZI SA, SHRIVASTAVA SC, AHMED AM. Stress analysis of the lumbar disc-body unit in compression. A three-dimensional nonlinear finite element study. Spine (Phila Pa 1976). 1984;9(2):120-134. [18] XILONG C, JUNJUN Z, YULIANG S, et al. Biomechanical Comparison of Different Treatment Strategies for Thoracolumbar Burst Fracture: A Finite Element Study. World Neurosurg. 2023;180:e429-e439. [19] WANG W, BARAN GR, GARG H, et al. The Benefits of Cement Augmentation of Pedicle Screw Fixation Are Increased in Osteoporotic Bone: A Finite Element Analysis. Spine Deform. 2014;2(4):248-259. [20] GUO HZ, ZHANG SC, GUO DQ, et al. Influence of cement-augmented pedicle screws with different volumes of polymethylmethacrylate in osteoporotic lumbar vertebrae over the adjacent segments: a 3D finite element analysis. BMC Musculoskelet Disord. 2020;21(1):460. [21] GOEL VK, RAMIREZ SA, KONG W, et al. Cancellous bone Young’s modulus variation within the vertebral body of a ligamentous lumbar spine--application of bone adaptive remodeling concepts. J Biomech Eng. 1995;117(3):266-271. [22] SHIRAZI A, AHMED AM, SHRIVASTAVA SC. A finite element study of a lumbar motion segment subjected to pure sagittal plane moments. J Biomech. 1986;19(4):331-350. [23] POLIKEIT A, NOLTE LP, FERGUSON SJ. The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit: finite-element analysis. Spine (Phila Pa 1976). 2003;28(10):991-996. [24] KIM Y. Finite element analysis of anterior lumbar interbody fusion: threaded cylindrical cage and pedicle screw fixation. Spine (Phila Pa 1976). 2007;32(23):2558-2568. [25] CHEN G, XIN B, YIN M, et al. Biomechanical analysis of a novel height-adjustable nano-hydroxyapatite/polyamide-66 vertebral body: a finite element study. J Orthop Surg Res. 2019;14(1):368. [26] ZHANG GD, DU YK, JIANG GZ, et al. Biomechanical evaluation of different posterior fixation techniques for treating thoracolumbar burst fractures of osteoporosis old patients: a finite element analysis. Front Bioeng Biotechnol. 2023;11:1268557. [27] WU Y, CHEN CH, TSUANG FY, et al. The stability of long-segment and short-segment fixation for treating severe burst fractures at the thoracolumbar junction in osteoporotic bone: A finite element analysis. PLoS One. 2019;14(2):e0211676. [28] PFLUGMACHER R, SCHLEICHER P, SCHAEFER J, et al. Biomechanical comparison of expandable cages for vertebral body replacement in the thoracolumbar spine. Spine (Phila Pa 1976). 2004;29(13):1413-1419. [29] LU H, ZHANG Q, DING F, et al. Finite Element Analysis of Unilateral versus Bipedicular Bone-Filling Mesh Container for the Management of Osteoporotic Compression Fractures. Biomed Res Int. 2022;2022: 6850089. [30] BASARAN R, EFENDIOGLU M, KAKSI M, et al. Finite element analysis of short- versus long-segment posterior fixation for thoracolumbar burst fracture. World Neurosurg. 2019;128:e1109-e1117. [31] SHIN SR, LEE SS, KIM JH, et al. Thoracolumbar burst fractures in patients with neurological deficit: Anterior approach versus posterior percutaneous fixation with laminotomy. J Clin Neurosci. 2020;75: 11-18. [32] SCHNAKE KJ, BLATTERT TR, HAHN P, et al. Classification of Osteoporotic Thoracolumbar Spine Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J. 2018;8(2 Suppl):46S-49S. [33] WANG K, ZHANG F, ZHAI Y, et al. Can preoperative magnetic resonance imaging be used for sagittal kyphotic flexibility assessment in patients with kyphosis secondary to symptomatic old osteoporotic thoracolumbar fracture? J Orthop Surg Res. 2023;18(1):133. [34] 眭涛, 陈建, 黄振飞, 等. 老年骨质疏松性胸腰椎骨折后脊柱重建临床指南(2022版)[J]. 中华创伤杂志,2022,38(12):1057-1066. [35] ULLRICH BW, SCHENK P, SCHEYERER MJ, et al. Georg Schmorl prize of the German spine society (DWG) 2022: current treatment for inpatients with osteoporotic thoracolumbar fractures-results of the EOFTT study. Eur Spine J. 2023;32(5):1525-1535. [36] SPIEGL UJA, SCHENK P, SCHNAKE KJ, et al. Working Group Osteoporotic Fractures of the Spine Section of the German Society of Orthopaedics and Trauma. Treatment and Outcome of Osteoporotic Thoracolumbar Vertebral Body Fractures With Deformation of Both Endplates With or Without Posterior Wall Involvement (OF 4): Short-Term Results from the Prospective EOFTT Multicenter Study. Global Spine J. 2023; 13(1_suppl):36S-43S. [37] ADLER D, AKBAR M, SPICHER A, et al. Biomechanical Study of a Novel, Expandable, Non-Metallic and Radiolucent CF/PEEK Vertebral Body Replacement (VBR). Materials (Basel). 2019;12(17):2732. [38] SIRCAR K, WEBER M, WALTER SG, et al. Torque forces of expandable titanium vertebral body replacement cages during expansion and subsidence in the osteoporotic lumbar spine. Clin Biomech (Bristol, Avon). 2024;114:106239. [39] XU C, BAI X, RUAN D, et al. Comparative finite element analysis of posterior short segment fixation constructs with or without intermediate screws in the fractured vertebrae for the treatment of type a thoracolumbar fracture. Comput Methods Biomech Biomed Engin. 2024;27(11):1398-1409. [40] GUO HZ, TANG YC, GUO DQ, et al. The cement leakage in cement-augmented pedicle screw instrumentation in degenerative lumbosacral diseases: a retrospective analysis of 202 cases and 950 augmented pedicle screws. Eur Spine J. 2019;28(7):1661-1669. [41] 郑雪静, 梅伟, 朱彦谕, 等. 伤椎置钉结合经椎弓根打压植骨治疗Ⅲ期Kümmell病:快速恢复脊柱稳定[J]. 中国组织工程研究, 2024,28(18):2865-2870. [42] 冷俊胜, 曾岩, 陈仲强. 骨水泥强化椎弓根螺钉技术在脊柱手术中的应用[J]. 中华骨科杂志,2019,39(10):637-644. [43] TSUANG FY, LI MJ, CHU PH, et al. Mechanical performance of porous biomimetic intervertebral body fusion devices: an in vitro biomechanical study. J Orthop Surg Res. 2023;18(1):71. [44] LIMTHONGKUL W, WANNARATSIRI N, SUKJAMSRI C, et al. Biomechanical Comparison Between Posterior Long-Segment Fixation, Short-Segment Fixation, and Short-Segment Fixation With Intermediate Screws for the Treatment of Thoracolumbar Burst Fracture: A Finite Element Analysis. Int J Spine Surg. 2023;17(3):442-448. [45] MIRZAALI MJ, SCHWIEDRZIK JJ, THAIWICHAI S, et al. Mechanical properties of cortical bone and their relationships with age, gender, composition and microindentation properties in the elderly. Bone. 2016;93:196-211. |
| [1] | Chen Huiting, Zeng Weiquan, Zhou Jianhong, Wang Jie, Zhuang Congying, Chen Peiyou, Liang Zeqian, Deng Weiming. Tail anchoring technique of vertebroplasty in treatment of osteoporotic vertebral compression fractures with intravertebral cleft: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2145-2152. |
| [2] | Zeng Xuan, Weng Rui, Ye Shicheng, Tang Jiadong, Mo Ling, Li Wenchao. Two lumbar rotary manipulation techniques in treating lumbar disc herniation: a finite element analysis of biomechanical differences [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2153-2161. |
| [3] | Cheng Qisheng, Julaiti·Maitirouzi, Xiao Yang, Zhang Chenwei, Paerhati·Rexiti. Finite element analysis of novel variable-diameter screws in modified cortical bone trajectory of lumbar vertebrae [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2162-2171. |
| [4] | Wu Hongxu, Liu Xuanyu, Wang Taoyu, Wang Shiyao, Cheng Jingyi, Zhang Mingwen, Zhang Yinxia, Liu Zhihua, Wang Xiaojie. Finite element simulation of scoliosis with muscle unit introduction: verification of correction effect under bidirectional load [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2172-2181. |
| [5] | Liu Jiafu, Ren Ruxia, Liao Zhouwei, Zhou Xiali, Wu Yihong, Zhang Shaoqun. Three-dimensional finite element analysis of cervical spine biomechanical characteristics in a rat model of cervical vertigo [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2182-2190. |
| [6] | Zhang Nan, Meng Qinghua, Bao Chunyu. Characteristics and clinical application of ankle joint finite element models [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2343-2349. |
| [7] | Zhou Daobin, Wang Kehao, Xie Yang, Ning Rende. Biomechanical characteristics of volar locking plate only versus combined dorsal mini-plate fixation of distal radius fractures with dorsal ulnar fragment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2255-2261. |
| [8] | Liu Wenlong, Dong Lei, Xiao Zhengzheng, Nie Yu. Finite element analysis of tibial prosthesis loosening after fixed-bearing unicompartmental knee arthroplasty for osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2191-2198. |
| [9] | Zheng Wangyang, Fei Ji, Yang Di, Zhao Lang, Wang Lingli, Liu Peng, Li Haiyang. Finite element analysis of the force changes of the supraspinatus tendon and glenohumeral joint during the abduction and flexion of the humerus [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2199-2207. |
| [10] | Cai Qirui, Dai Xiaowei, Zheng Xiaobin, Jian Sili, Lu Shaoping, Liu Texi, Liu Guoke, Lin Yuanfang. Mechanical effects of Long’s traction orthopedic method on cervical functional units: quantitative analysis of biomechanical model of head and neck [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2208-2216. |
| [11] | Rao Jingcheng, Li Yuwan, Zheng Hongbing, Xu Zhi, Zhu Aixiang, Shi Ce, Wang Bing, Yang Chun, Kong Xiangru, Zhu Dawei. Biomechanical differences between the new proximal femoral stable intramedullary nail and traditional intramedullary nail#br# [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2217-2225. |
| [12] | Yan Xiangning, Chen Lei, Chen Yonghuan, Wang Chao, Li Xiaosheng. Influence of different depths and loads on knee joint mechanics and peripheral muscle force characteristics during squatting [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2236-2247. |
| [13] | Zhang Xianxu, Ma Zhong, Liu Xin, Huang Lei, Shen Wenxiang, Luo Zhiqiang . Lumbar fusion combined with unilateral fixation for lumbar degenerative diseases: biomechanics, technical evolution, and clinical applications [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2334-2342. |
| [14] | Hu Xiongke, Liu Shaohua, Tan Qian, Liu Kun, Zhu Guanghui. Shikonin intervention with bone marrow mesenchymal stem cells improves microstructure of femur in aged mice [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1609-1615. |
| [15] | Wu Zhilin, , He Qin, Wang Pingxi, Shi Xian, Yuan Song, Zhang Jun, Wang Hao . DYRK2: a novel therapeutic target for rheumatoid arthritis combined with osteoporosis based on East Asian and European populations [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1569-1579. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||