Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (9): 2217-2225.doi: 10.12307/2026.620
Previous Articles Next Articles
Biomechanical differences between the new proximal femoral stable intramedullary nail and traditional intramedullary nail#br#
Rao Jingcheng1, Li Yuwan2, Zheng Hongbing1, Xu Zhi3, Zhu Aixiang1, Shi Ce1, Wang Bing1, Yang Chun1, Kong Xiangru1, Zhu Dawei1
- 1Nanjing Drum Tower Hospital Group Suqian Hospital (Suqian Hospital Affiliated to Xuzhou Medical University), Suqian 223800, Jiangsu Province, China; 2First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310009, Zhejiang Province, China; 3Department of Orthopedics, Zhangjiagang Fifth People’s Hospital, Zhangjiagang 215600, Jiangsu Province, China
-
Received:2025-02-08Accepted:2025-04-12Online:2026-03-28Published:2025-09-05 -
Contact:Zhu Dawei, MS, Chief physician, Nanjing Drum Tower Hospital Group Suqian Hospital (Suqian Hospital Affiliated to Xuzhou Medical University), Suqian 223800, Jiangsu Province, China -
About author:Rao Jingcheng, MS, Attending physician, Nanjing Drum Tower Hospital Group Suqian Hospital (Suqian Hospital Affiliated to Xuzhou Medical University), Suqian 223800, Jiangsu Province, China -
Supported by:Youth Science Foundation of National Natural Science Foundation, No. 82302853 (to LYW); Jiangsu Provincial Social Development Key Research and Development Project, No. BE2019703 (to WB)
CLC Number:
Cite this article
Rao Jingcheng, Li Yuwan, Zheng Hongbing, Xu Zhi, Zhu Aixiang, Shi Ce, Wang Bing, Yang Chun, Kong Xiangru, Zhu Dawei. Biomechanical differences between the new proximal femoral stable intramedullary nail and traditional intramedullary nail#br#[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2217-2225.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
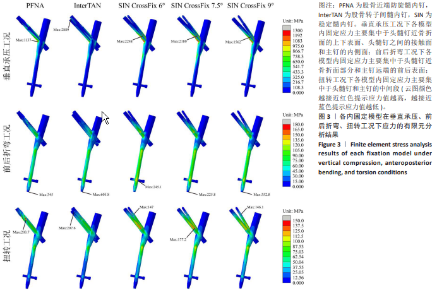
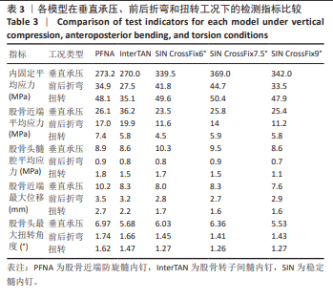
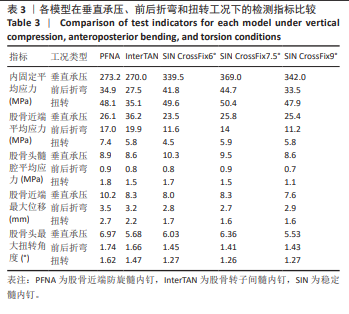
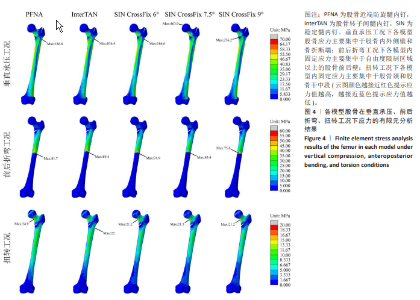
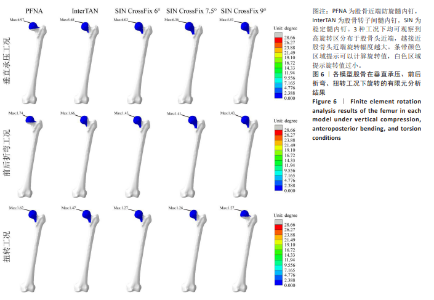
2.1 内固定应力比较 如图3及表3所示,在垂直承压工况下,PFNA、InterTAN、SIN CrossFix6°、SIN CrossFix7.5°、SIN CrossFix9°应力均值分别为273.2,270,339.5,369,342 MPa,应力大小排序为:SIN CrossFix7.5° > SIN CrossFix9° > SIN CrossFix6° > PFNA > InterTAN,应力云图显示PFNA峰应力发生于螺旋刀片和主钉内侧壁交界处,InterTAN峰应力则发生于2枚头髓钉近端接触面上,3种SIN峰应力均发生于压力钉和拉力螺钉近主钉处的接触面上。在前后折弯工况下,5种内固定应力均值分别为34.9,27.5,41.8,44.7,33.5 MPa,应力大小排序为:SIN CrossFix7.5° > SIN CrossFix6° > PFNA > SIN CrossFix9° > InterTAN,应力云图显示SIN CrossFix6°峰应力发生于主钉远端螺钉道口、其余4个模型峰应力均发生于主钉远端。在扭转工况下,5种内固定应力均值分别为48.1,35.1,49.6,50.4,47.9 MPa,应力大小排序为:SIN CrossFix7.5° > SIN CrossFix6° > PFNA > SIN CrossFix9° > InterTAN,应力云图显示PFNA峰应力发生于螺旋刀片刀头近骨折线处,InterTAN峰应力与垂直工况下类似出现在2枚头髓钉近端接触面上,SIN CrossFix6°和SIN CrossFix9°峰应力均发生于拉力钉螺纹近骨折面处,SIN CrossFix7.5°峰应力发生于压力钉基底部近骨折面处。"
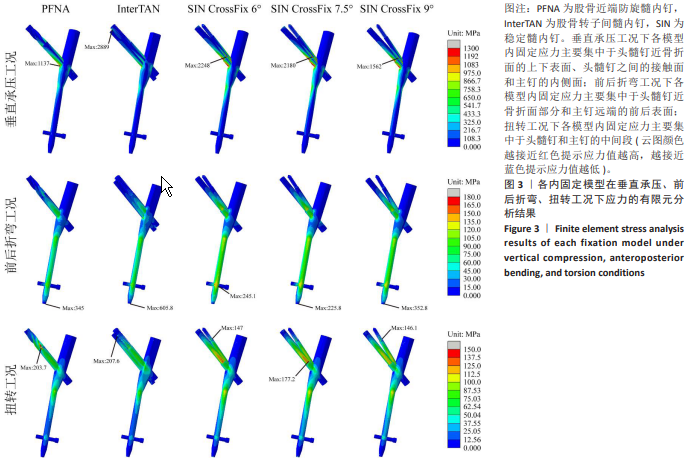
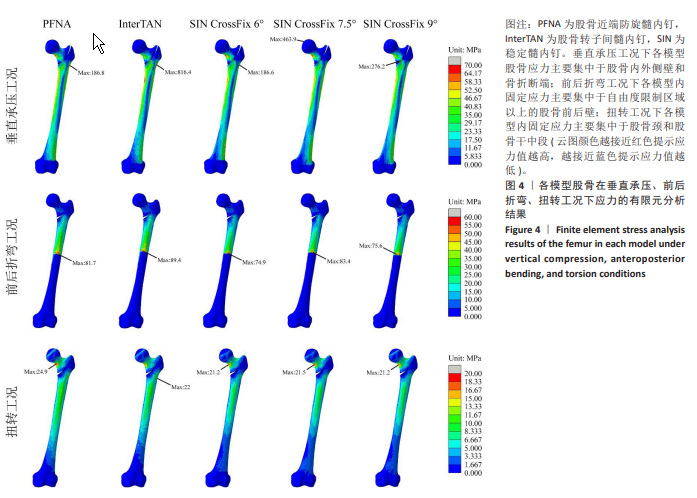
2.2 股骨近端/髓腔应力比较 如图4及表3所示,在垂直承压工况下,PFNA、InterTAN、SIN CrossFix6°、SIN CrossFix7.5°、SIN CrossFix9°股骨近端应力均值分别为26.1,36.2,23.5,25.8,25.4 MPa,应力大小排序为:InterTAN > PFNA > SIN CrossFix7.5° > SIN CrossFix9° > SIN CrossFix6°,在此工况下5个模型髓腔应力均值则为8.9,8.6,10.3,9.5,8.6 MPa,应力大小排序为:SIN CrossFix6° > SIN CrossFix7.5° > PFNA > InterTAN =SIN CrossFix9°,应力云图显示PFNA、InterTAN和SIN CrossFix6°峰应力均发生于外侧壁骨隧道口,SIN CrossFix7.5°峰应力发生于股骨头,SIN CrossFix9°峰应力发生于近端骨折断端接触面上。在前后折弯工况下,5个模型股骨近端应力均值分别为17,19.9,11.6,14,11.2 MPa,应力大小排序为:InterTAN > PFNA > SIN CrossFix7.5° > SIN CrossFix6° > SIN CrossFix9°,在此工况下5个模型髓腔应力均值则为0.9,0.8,0.8,0.9,0.7 MPa,应力大小排序为:PFNA= SIN CrossFix7.5° > InterTAN= SIN CrossFix6° > SIN CrossFix9°,应力云图显示5个模型股骨峰应力均出现在股骨前壁中段自由度限制区上缘。在扭转工况下,5个模型股骨近端应力均值分别为7.4,5.8,4.5,5.9,5.8 MPa,应力大小排序为:PFNA > SIN CrossFix7.5° > InterTAN= SIN CrossFix9° > SIN CrossFix6°,在此工况下5个模型髓腔应力均值则为1.8,1.5,1.7,1.5,1.1 MPa,应力大小排序为:PFNA > SIN CrossFix6° > InterTAN= SIN CrossFix7.5° > SIN CrossFix9°,应力云图显示除InterTAN股骨峰应力发生于外侧壁钉道口之外,其余4个模型峰应力均发生于股骨颈下表面。"
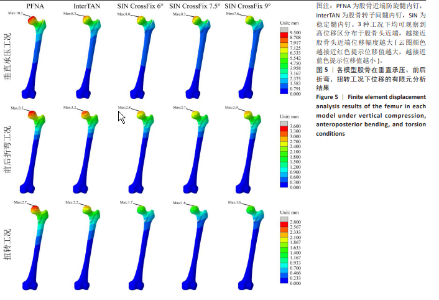
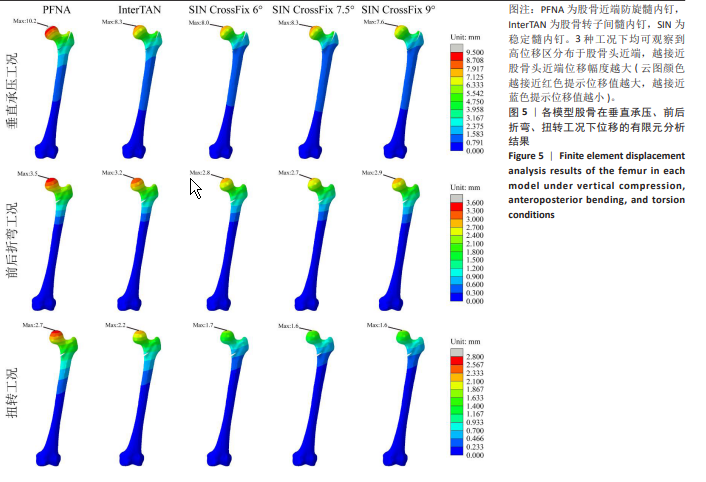
2.3 股骨位移比较 如表3所示,在垂直承压工况下,PFNA、InterTAN、SIN CrossFix6°、SIN CrossFix7.5°、SIN CrossFix9°最大位移分别为10.2,8.3,8,8.3,7.6 mm,位移大小排序为:PFNA > InterTAN= SIN CrossFix7.5° > SIN CrossFix6° > SIN CrossFix9°。在前后折弯工况下,5个模型最大位移分别为3.5,3.2,2.8,2.7,2.9 mm,位移大小排序为:PFNA > InterTAN > SIN CrossFix9° > SIN CrossFix6° > SIN CrossFix7.5°。在扭转工况下,5个模型最大位移分别为2.7,2.2,1.7,1.6,1.6 mm,位移大小排序为:PFNA > InterTAN > SIN CrossFix6° > SIN CrossFix7.5°= SIN CrossFix9°,3种工况下的位移云图显示5个模型最大位移均出现在股骨头近端(图5)。"
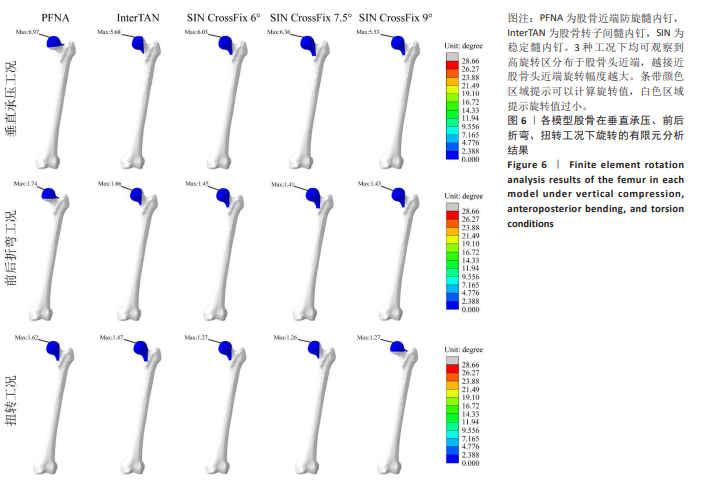
2.4 股骨头旋转比较 如表3所示,在垂直承压工况下,PFNA、InterTAN、SIN CrossFix6°、SIN CrossFix7.5°、SIN CrossFix9°最大旋转角度分别为6.97°,5.68°,6.03°,6.36°,5.53°,旋转大小排序为:PFNA > SIN CrossFix7.5° > SIN CrossFix6° > InterTAN > SIN CrossFix9°。在前后折弯工况下,5个模型最大旋转角度分别为1.74°,1.66°,1.45°,1.41°,1.43°,旋转大小排序为:PFNA > InterTAN > SIN CrossFix6° > SIN CrossFix9° > SIN CrossFix7.5°。在扭转工况下,5个模型最大旋转角度分别为1.62°,1.47°,1.27°,1.26°,1.27°,旋转大小排序为:PFNA > InterTAN > SIN CrossFix6°= SIN CrossFix9° > SIN CrossFix7.5°。3种工况下的旋转云图显示5个模型最大位移均出现在股骨头近端(图6)。"
| [1] HUANG Q, XU Y, XUE H, et al. Percutaneous reduction with double screwdrivers versus limited open reduction in the treatment of irreducible extracapsular hip fractures. BMC Musculoskelet Disord. 2022;23(1):429. [2] BI C, ZHAO Y, MA Z, et al. Comparison of Proximal Anti-Rotation Intramedullary Nail and Femoral Head Replacement for the Treatment of Femoral Intertrochanteric Fractures in Elderly Patients. Altern Ther Health Med. 2023;29(5):268-273. [3] 孙鸿朔, 张治博, 李孟奇, 等. 新型牵引床闭合复位髓内钉固定股骨粗隆间骨折[J]. 中国矫形外科杂志,2024,32(6):506-511. [4] AN Y, JIANG D. Biomechanical effects of three internal fixation modes on femoral subtrochanteric spiral fractures in osteoporotic patients by finite element analysis. Zhongguo xiu fu chong jian wai ke za zhi. 2023;37(6):688-693. [5] 徐志, 仲鹤鹤, 向浩, 等. 股骨干骨折3种不同固定方式的有限元分析[J]. 中国组织工程研究,2022,26(33):5271-5277. [6] 李浩涛, 李力文, 张世民. 股骨转子间骨折后壁冠状面“香蕉样骨块”特点及其在头髓钉治疗中的研究进展[J]. 中国修复重建外科杂志, 2024,38(12):1517-1523. [7] 王伟, 张金明, 杨占辉, 等. 有限切开复位钛缆环扎联合加长型髓内钉治疗股骨转子下骨折的效果[J]. 滨州医学院学报, 2023,46(4):312-314. [8] 张巍, 唐佩福.老年髋部骨折治疗方法的选择与进展[J]. 中国骨伤, 2023,36(12):1111-1113. [9] CHLEBECK JD, BIRCH CE, BLANKSTEIN M, et al. Nonoperative Geriatric Hip Fracture Treatment Is Associated With Increased Mortality: A Matched Cohort Study. J Orthop Trauma. 2019;33(7):346-350. [10] USAMI T, TAKADA N, KOSUWON W, et al. A Lateral Fracture Line Affects Femoral Trochanteric Fracture Instability and Swing Motion of the Intramedullary Nail: A Biomechanical Study. JB JS Open Access. 2024; 9(1):2300118. [11] CHEN X, HU Y, GENG Z, et al. The “Three in One” Bone Repair Strategy for Osteoporotic Fractures. Front Endocrinol (Lausanne). 2022;13:910602. [12] SONG H, CHANG SM, HU SJ, et al. Low filling ratio of the distal nail segment to the medullary canal is a risk factor for loss of anteromedial cortical support: a case control study. J Orthop Surg Res. 2022;17(1):27. [13] TANG Z, LV Y, ZHU Z, et al. Biomechanical characteristic differences of two new types of intramedullary nail devices in the treatment of comminuted intertrochanteric fractures of femur: a comparative study based on finite element analysis. J Orthop Surg Res. 2024;19(1):583. [14] 杨青, 牛宇飞, 苏静亮, 等. InterTan结合重建钢板治疗老年股骨转子间骨折PFNA内固定术后髓钉断裂的疗效分析[J]. 生物骨科材料与临床研究,2024,21(3):58-63. [15] 缪建云, 徐维臻, 翟文亮, 等. 髓内钉联合髓外固定治疗伴有冠状面骨折的股骨粗隆间骨折的疗效观察[J]. 中国中医骨伤科杂志,2025,33(1):74-77. [16] LI J, ZHANG L, ZHANG H, et al. Effect of reduction quality on post-operative outcomes in 31-A2 intertrochanteric fractures following intramedullary fixation: a retrospective study based on computerised tomography findings. Int Orthop. 2019;43(8):1951-1959. [17] 史文骥, 毛宾尧, 赵艳. 股骨近端防旋髓内钉治疗老年股骨转子间骨折疗效及并发症探讨[J]. 中国骨伤,2021,34(10):906-910. [18] WANG Y, CHEN W, ZHANG L, et al. Finite Element Analysis of Proximal Femur Bionic Nail (PFBN) Compared with Proximal Femoral Nail Antirotation and InterTan in Treatment of Intertrochanteric Fractures. Orthop Surg. 2022;14(9):2245-2255. [19] 徐志, 刘子铭, 李豫皖, 等. 多孔结构设计人工踝关节衬垫生物力学的优化方案[J].中国组织工程研究,2024,28(30):4817-4824. [20] 徐志, 李豫皖, 刘子铭, 等. 五种内固定方式治疗SeinsheimerⅤ型股骨转子下骨折的生物力学特性比较[J].中华骨科杂志,2024,44(9):616-625. [21] LI J, YIN P, ZHANG L, et al. Medial anatomical buttress plate in treating displaced femoral neck fracture a finite element analysis. Injury. 2019; 50(11):1895-1900. [22] WANG Q, SUN L, LIU L, et al. Biomechanical evaluation of the modified proximal femoral nail for the treatment of reverse obliquity intertrochanteric fractures. Sci Rep. 2025;15(1):3261. [23] HOHENDORFF B, MEYER P, MENEZES D, et al. Treatment results and complications after PFN osteosynthesis. Unfallchirurg. 2005;108(11):938, 940-946. [24] BONNAIRE F, LEIN T, FÜLLING T, et al. Reduced complication rates for unstable trochanteric fractures managed with third-generation nails: Gamma 3 nail versus PFNA. Eur J Trauma Emerg Surg. 2020;46(5):955-962. [25] 孟永标, 杨跃芬, 吴生华, 等. 股骨近端防旋髓内钉治疗老年股骨粗隆间骨折合并膝骨关节炎的效果[J]. 浙江创伤外科,2025,30(2):238-241. [26] MURUGAN PB, MOHIDEEN S, PRADEEP E, et al. Comparison of functional and radiological outcome of unstable intertrochanteric femur fractures treated using PFN and PFNA in patients with osteoporosis. J Orthop Case Rep. 2024; 14(10):219-224. [27] 田可为, 陈勤, 陈柯, 等. 股骨近端防旋髓内钉内固定术后尾帽退出并发症临床报道[J].中国修复重建外科杂志,2023,37(2):252-254. [28] 冯皓, 张斌, 聂涛. 三种术式治疗老年不稳定股骨粗隆间骨折术后并发症及远期疗效[J].中国老年学杂志,2021,41(9):1850-1853. [29] LU X, GOU W, WU S, et al. Complication Rates and Survival of Nonagenarians after Hip Hemiarthroplasty versus Proximal Femoral Nail Antirotation for Intertrochanteric Fractures: A 15-Year Retrospective Cohort Study of 113 Cases. Orthop Surg. 2023;15(12):3231-3242. [30] ZHU Z, ZHAO Z, WANG X, et al. A comparison of functional and radiological outcome of combine compression antegrade intertrochanteric nail (InterTan) and proximal femoral nail anti-rotation II (PFNA-II) in elderly patients with intertrochanteric fractures. Pak J Med Sci. 2023;39(1):96-100. [31] 金立昆, 李晔, 张杰, 等. 不同髓内固定方式治疗股骨转子间骨折的临床观察[J]. 中国骨伤,2024,37(3):293-299. [32] 傅宏沛, 周云烽, 贾俊杰, 等. PFBN、InterTan、PFNA髓内钉内固定治疗老年股骨粗隆间骨折早期疗效比较[J].中国骨与关节损伤杂志, 2023,38(10):1058-1061. [33] 杨冬松, 王琼, 陈许冬, 等. 股骨近端仿生髓内钉治疗外侧壁破裂型老年股骨转子间骨折的近期疗效观察[J]. 创伤外科杂志,2025,27(1):34-37. [34] BAI H, LIU L, DUAN N, et al. Biomechanical evaluation of three implants for treating unstable femoral intertrochanteric fractures: finite element analysis in axial, bending and torsion loads. Front Bioeng Biotechnol. 2023; 11:1279067. [35] TANG Z, LV Y, ZHU Z, et al. Biomechanical characteristic differences of two new types of intramedullary nail devices in the treatment of comminuted intertrochanteric fractures of femur: a comparative study based on finite element analysis. J Orthop Surg Res. 2024;19(1):583. |
| [1] | Chen Huiting, Zeng Weiquan, Zhou Jianhong, Wang Jie, Zhuang Congying, Chen Peiyou, Liang Zeqian, Deng Weiming. Tail anchoring technique of vertebroplasty in treatment of osteoporotic vertebral compression fractures with intravertebral cleft: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2145-2152. |
| [2] | Zeng Xuan, Weng Rui, Ye Shicheng, Tang Jiadong, Mo Ling, Li Wenchao. Two lumbar rotary manipulation techniques in treating lumbar disc herniation: a finite element analysis of biomechanical differences [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2153-2161. |
| [3] | Cheng Qisheng, Julaiti·Maitirouzi, Xiao Yang, Zhang Chenwei, Paerhati·Rexiti. Finite element analysis of novel variable-diameter screws in modified cortical bone trajectory of lumbar vertebrae [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2162-2171. |
| [4] | Wu Hongxu, Liu Xuanyu, Wang Taoyu, Wang Shiyao, Cheng Jingyi, Zhang Mingwen, Zhang Yinxia, Liu Zhihua, Wang Xiaojie. Finite element simulation of scoliosis with muscle unit introduction: verification of correction effect under bidirectional load [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2172-2181. |
| [5] | Liu Jiafu, Ren Ruxia, Liao Zhouwei, Zhou Xiali, Wu Yihong, Zhang Shaoqun. Three-dimensional finite element analysis of cervical spine biomechanical characteristics in a rat model of cervical vertigo [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2182-2190. |
| [6] | Liu Wenlong, Dong Lei, Xiao Zhengzheng, Nie Yu. Finite element analysis of tibial prosthesis loosening after fixed-bearing unicompartmental knee arthroplasty for osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2191-2198. |
| [7] | Zheng Wangyang, Fei Ji, Yang Di, Zhao Lang, Wang Lingli, Liu Peng, Li Haiyang. Finite element analysis of the force changes of the supraspinatus tendon and glenohumeral joint during the abduction and flexion of the humerus [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2199-2207. |
| [8] | Cai Qirui, Dai Xiaowei, Zheng Xiaobin, Jian Sili, Lu Shaoping, Liu Texi, Liu Guoke, Lin Yuanfang. Mechanical effects of Long’s traction orthopedic method on cervical functional units: quantitative analysis of biomechanical model of head and neck [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2208-2216. |
| [9] | Chen Long, Wang Xiaozhen, Xi Jintao, Lu Qilin. Biomechanical performance of short-segment screw fixation combined with expandable polyetheretherketone vertebral body replacement in osteoporotic vertebrae [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2226-2235. |
| [10] | Yan Xiangning, Chen Lei, Chen Yonghuan, Wang Chao, Li Xiaosheng. Influence of different depths and loads on knee joint mechanics and peripheral muscle force characteristics during squatting [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2236-2247. |
| [11] | Zhou Daobin, Wang Kehao, Xie Yang, Ning Rende. Biomechanical characteristics of volar locking plate only versus combined dorsal mini-plate fixation of distal radius fractures with dorsal ulnar fragment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2255-2261. |
| [12] | Zheng Xuying, Hu Hongcheng, Xu Libing, Han Jianmin, Di Ping. Stress magnitude and distribution in two-piece cement-retained zirconia implants under different loading conditions and with varying internal connection shapes [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1979-1987. |
| [13] | Zhong Caihong, Xiao Xiaoge, Li Ming, Lin Jianhong, Hong Jing. Biomechanical mechanism of sports-related patellar tendinitis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1417-1423. |
| [14] | Xu Hao, Ding Lu, Li Xiao. Mechanical effect of mechanical wear of abutment screws on the Morse taper connection implant system: a three-dimensional finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1375-1383. |
| [15] | Shang Depeng, Wei Haiyu, Yang Fan. Finite element analysis for three different types of internal screw fixation in treatment of severe lumbar 1 vertebral body fractures [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 537-545. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||