Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (15): 3936-3945.doi: 10.12307/2026.683
Previous Articles Next Articles
Differences in clinical function and imaging between robot-assisted and conventional total knee arthroplasty
Liu Haoyang1, Li Hongxu1, Zhou Yu1, Yue Debo2, Wang Bailiang2, Ma Jinhui2
- 1China-Japan Friendship School of Clinical Medicine, Peking University, Beijing 100029, China; 2Department of Orthopedic Surgery, China-Japan Friendship Hospital, Beijing 100029, China
-
Accepted:2025-04-22Online:2026-05-28Published:2025-11-07 -
Contact:Wang Bailiang, MD, Chief physician, Master’s supervisor, Department of Orthopedic Surgery, China-Japan Friendship Hospital, Beijing 100029, China Ma Jinhui, MD, Department of Orthopedic Surgery, China-Japan Friendship Hospital, Beijing 100029, China -
About author:Liu Haoyang, Master candidate, China-Japan Friendship School of Clinical Medicine, Peking University, Beijing 100029, China -
Supported by:Education and Teaching Reform Research Project of Capital Medical University, No. 2023JYY388 (to MJH); Clinical Research Business Funds of Central High-level Hospitals, Talent Cultivation Project of China-Japan Friendship Hospital “Elite Program”, No. ZRJY2021-TD01 (to WBL)
CLC Number:
Cite this article
Liu Haoyang, Li Hongxu, Zhou Yu, Yue Debo, Wang Bailiang, Ma Jinhui. Differences in clinical function and imaging between robot-assisted and conventional total knee arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(15): 3936-3945.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

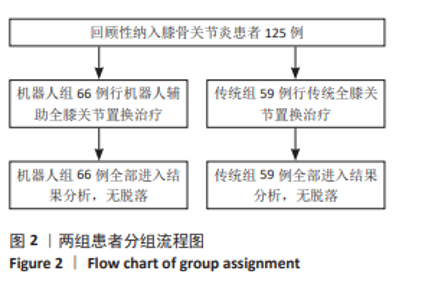
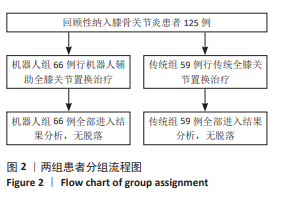
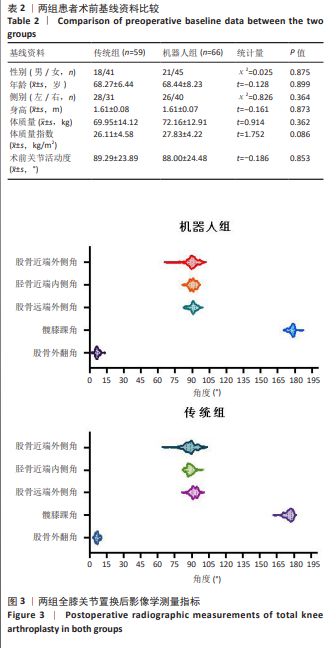
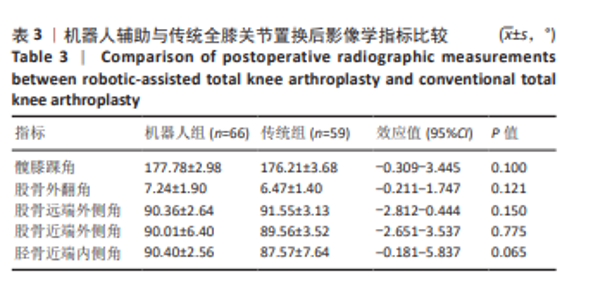
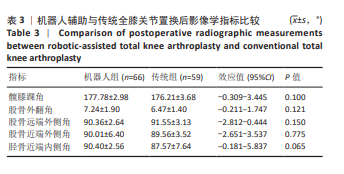
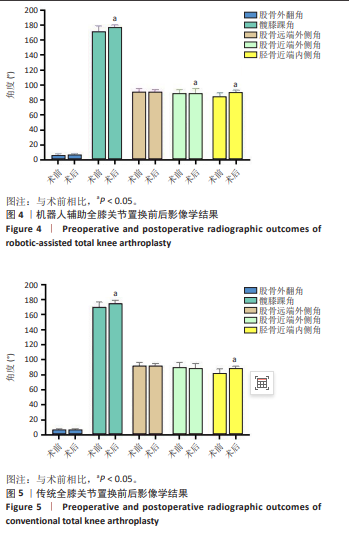
2.4 影像学指标比较 关于机器人组与传统组术后不同测量角度的比较,采用小提琴图展示于图3。X射线片复查结果显示,所有患者的下肢力线均有所改善,且膝关节假体位置良好。术后X射线片影像学测量结果表明,机器人组中,除股骨外翻角和股骨远端外侧角术前术后无显著性差异外(P > 0.05),髋膝踝角、胫骨近端内侧角和股骨近端外侧角均较术前显著改善(P < 0.05),详见图4;而在传统组中,股骨外翻角、股骨近端外侧角和股骨远端外侧角无显著差异(P > 0.05),髋膝踝角和胫骨近端内侧角较术前显著改善(P < 0.05),详见图5。在机器人组和传统组术后影像学角度的比较中,各项指标均无显著性差异(P > 0.05),详见表3。此外,在两组术前与术后差值的比较中,除股骨外翻角和股骨近端外侧角外,其余指标均无显著性差异(P > 0.05),详见表4。"
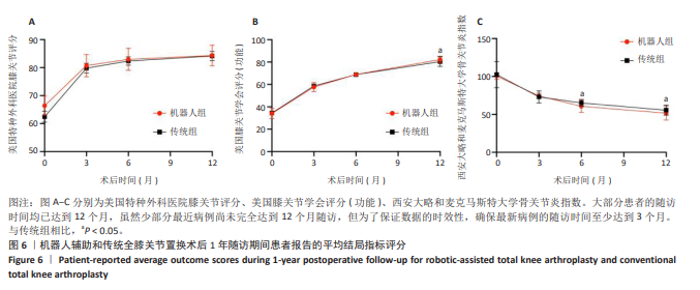
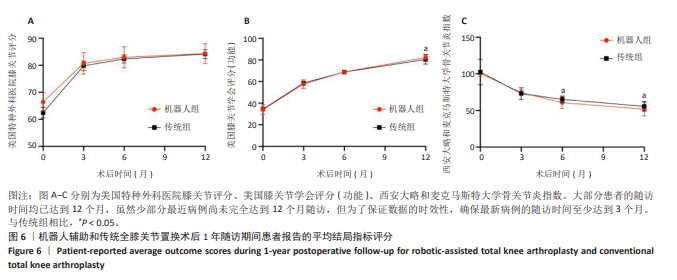
2.5 临床指标比较 机器人组较传统组平均手术时间长27.74 min(117.69 min vs. 89.95 min)(P < 0.05),平均止血带使用时间传统组较机器人组时间长39.10 min (55.69 min vs. 15.59 min)(P < 0.05),两组的平均失血量无显著性差异(P=0.359)。两组患者术后1周活动度均较术前改善,机器人组活动度平均改善9.63°,传统组为22.59°(P=0.066),详见表5。在美国特种外科医院评分方面,术前、术后3,6,12个月两组间相比均无显著性差异(P=0.865,0.482,0.347,0.688)。在美国膝关节学会评分(功能)方面,术前、术后3,6个月两组间相比均无显著性差异(P=0.821,0.147,0.699);1年时机器人组提高到(82.15±3.16)分,而传统组为(80.33±4.24)分,两组间差异有显著性意义(P=0.009 < 0.05),说明从长远随访来看,机器人组在美国膝关节学会评分(功能)改善方面优于传统组。在西安大略和麦克马斯特大学骨关节炎指数方面,术前、术后3个月两组间相比均无显著性差异(P=0.409,0.174),术后3个月时机器人组、传统组分别较术前降低了28.38分和28.05分;术后6个月时传统组、机器人组分别为(64.50±3.72)分和(60.90±8.01)分,机器人组优于传统组(P < 0.05);术后1年时两组分别为(54.69±5.98)分和(51.68±9.13)分,机器人组优于传统组(P < 0.05),见图6。"
| [1] KAHLENBERG CA, NWACHUKWU BU, MCLAWHORN AS, et al. Patient Satisfaction After Total Knee Replacement: A Systematic Review. HSS J. 2018;14(2):192-201. [2] BAUTISTA M, MANRIQUE J, HOZACK WJ. Robotics in Total Knee Arthroplasty. J Knee Surg. 2019;32(7):600-606. [3] KHATRI C, METCALFE A, WALL P, et al. Robotic trials in arthroplasty surgery. Bone Joint J. 2024;106-b(2):114-120. [4] BANERJEE S, CHERIAN JJ, ELMALLAH RK, et al. Robotic-Assisted Knee Arthroplasty. Expert Rev Med Devices. 2015;12(6):727-735. [5] SONG EK, SEON JK, YIM JH, et al. Robotic-Assisted TKA Reduces Postoperative Alignment Outliers and Improves Gap Balance Compared to Conventional TKA. Clin Orthop Relat Res. 2013;471(1):118-126. [6] JAKOPEC M, HARRIS SJ, RODRIGUEZ Y, et al. The First Clinical Application of a “Hands-On” Robotic Knee Surgery System. Comput Aided Surg. 2001;6(6):329-339. [7] PARRATTE S, PAGNANO MW, TROUSDALE RT, et al. Effect of Postoperative Mechanical Axis Alignment on the Fifteen-Year Survival of Modern, Cemented Total Knee Replacements. J Bone Joint Surg Am. 2010;92(12):2143-2149. [8] REED SC, GOLLISH J. The Accuracy of Femoral Intramedullary Guides in Total Knee Arthroplasty. J Arthroplasty. 1997;12(6):677-682. [9] RITTER MA, DAVIS KE, MEDING JB, et al. The Effect of Alignment and BMI on Failure of Total Knee Replacement. J Bone Joint Surg Am. 2011; 93(17):1588-1596. [10] GOH GS, LIOW MHL, ABD RAZAK HR, et al. Patient-Reported Outcomes, Quality of Life, and Satisfaction Rates in Young Patients Aged 50 Years or Younger After Total Knee Arthroplasty. J Arthroplasty. 2017;32(2): 419-425. [11] HELD MB, GROSSO MJ, GAZGALIS A, et al. Improved Compartment Balancing Using a Robot-Assisted Total Knee Arthroplasty. Arthroplast Today. 2021;7:130-134. [12] RAJGOR HD, MAYNE A, MUNASINGHE C, et al. Mako Versus ROSA: Comparing Surgical Accuracy in Robotic Total Knee Arthroplasty. J Robot Surg. 2024;18(1):33. [13] WU XD, ZHOU Y, SHAO H, et al. Robotic-Assisted Revision Total Joint Arthroplasty: A State-of-the-Art Scoping Review. EFORT Open Rev. 2023;8(1):18-25. [14] SEO SS, KIM CW, SEO JH, et al. Effects of Resection of Posterior Condyles of Femur on Extension Gap of Knee Joint in Total Knee Arthroplasty. J Arthroplasty. 2017;32(6):1819-1823. [15] MA N, SUN P, XIN P, et al. Comparison of the Efficacy and Safety of MAKO Robot-Assisted Total Knee Arthroplasty Versus Conventional Manual Total Knee Arthroplasty in Uncomplicated Unilateral Total Knee Arthroplasty a Single-Centre Retrospective Analysis. Int Orthop. 2024;48(9):2351-2358. [16] XU JZ, LI LL, FU J, et al. Comparison of Serum Inflammatory Indicators and Radiographic Results in MAKO Robotic-Assisted Versus Conventional Total Knee Arthroplasty for Knee Osteoarthritis: A Retrospective Study of Chinese Patients. BMC Musculoskelet Disord. 2022;23(1):418. [17] SIRES JD, WILSON CJ. Accuracy of Bone Resection in MAKO Total Knee Robotic-Assisted Surgery. J Knee Surg. 2021;34(7):745-748. [18] SHEN TS, UPPSTROM TJ, WALKER PJ, et al. High Degree of Alignment Precision Associated With Total Knee Arthroplasty Performed Using a Surgical Robot or Handheld Navigation. Knee Surg Sports Traumatol Arthrosc. 2023;31(11):4735-4740. [19] BATAILLER C, FERNANDEZ A, SWAN J, et al. MAKO CT-Based Robotic Arm-Assisted System Is a Reliable Procedure for Total Knee Arthroplasty: A Systematic Review. Knee Surg Sports Traumatol Arthrosc. 2021;29(11):3585-3598. [20] MARCHAND RC, SODHI N, KHLOPAS A, et al. Patient Satisfaction Outcomes After Robotic Arm-Assisted Total Knee Arthroplasty: A Short-Term Evaluation. J Knee Surg. 2017;30(9):849-853. [21] MARCHAND RC, SODHI N, ANIS HK, et al. One-Year Patient Outcomes for Robotic-Arm-Assisted Versus Manual Total Knee Arthroplasty. J Knee Surg. 2019;32(11):1063-1068. [22] WONG WK, ABU BAKAR SAJAK A, CHUA HS. Real-World Accuracy of Robotic-Assisted Total Knee Arthroplasty and Its Impact on Expedited Recovery. J Robot Surg. 2024;18(1):309. [23] COTTER EJ, WANG J, ILLGEN RL. Comparative Cost Analysis of Robotic-Assisted and Jig-Based Manual Primary Total Knee Arthroplasty. J Knee Surg. 2022;35(2):176-184. [24] KAYANI B, KONAN S, TAHMASSEBI J, et al. Robotic-Arm Assisted Total Knee Arthroplasty Is Associated With Improved Early Functional Recovery and Reduced Time to Hospital Discharge Compared With Conventional Jig-Based Total Knee Arthroplasty: A Prospective Cohort Study. Bone Joint J. 2018;100-B(7):930-937. [25] KARUMURI K, DESAI KB, HIPPALGAONKAR K, et al. Is It Worth the Risk? Frailty Transition and Complications Following Robotic Total Knee Arthroplasty: A Retrospective Observational Study. Knee. 2023;44: 72-78. [26] KAYANI B, KONAN S, HUQ SS, et al. Robotic-Arm Assisted Total Knee Arthroplasty Has a Learning Curve of Seven Cases for Integration Into the Surgical Workflow But No Learning Curve Effect for Accuracy of Implant Positioning. Knee Surg Sports Traumatol Arthrosc. 2019; 27(4):1132-1141. [27] SULTAN AA, SAMUEL LT, KHLOPAS A, et al. Robotic-Arm Assisted Total Knee Arthroplasty More Accurately Restored the Posterior Condylar Offset Ratio and the Insall-Salvati Index Compared to the Manual Technique; A Cohort-Matched Study. Surg Technol Int. 2019;34: 409-413. [28] LEE JH, KWON SC, HWANG JH, et al. Functional Alignment Maximises Advantages of Robotic Arm-Assisted Total Knee Arthroplasty With Better Patient-Reported Outcomes Compared to Mechanical Alignment. Knee Surg Sports Traumatol Arthrosc. 2024;32(4):896-906. [29] MANARA JR, GOONATILLAKE M, MARLEY M, et al. Virtual Assessment of Coronal Balance Prior to Bone Resection With the MAKO Robotic-Assisted System Accurately Predicts Final Balance in TKA. J Robot Surg. 2023;17(6):2849-2854. [30] MUKARTIHAL R, BHAT VK, DAS R, et al. Relationship Between Femoral Component Placement and Patient-Specific Anatomical Rotational Landmarks in Robotic Arm Assisted Total Knee Arthroplasty- A Multicentric Study. J Orthop. 2023;45:87-90. [31] GU Y, HOWELL SM, HULL ML. Simulation of Total Knee Arthroplasty in 5° or 7° Valgus: A Study of Gap Imbalances and Changes in Limb and Knee Alignments From Native. J Orthop Res. 2017;35(9):2031-2039. [32] MASILAMANI ABS, JAYAKUMAR T, MULPUR P, et al. Functional Alignment Is Associated With Increased Incidence of Pre-Balance, Reduced Soft-Tissue Release, and Post-Operative Pain Compared to Mechanical Alignment in Patients Undergoing Simultaneous Bilateral Robotic-Assisted TKA. J Robot Surg. 2023;17(6):2919-2927. [33] SELVANATHAN N, AYENI FE, SORIAL R. Incidence of Soft Tissue Releases in Robotic Assisted Cementless TKA With Mechanical Alignment and Flexion Gap Balancing. Arthroplasty. 2023;5(1):28. [34] VIGDORCHIK JM, WAKELIN EA, KOENIG JA, et al. Impact of Component Alignment and Soft Tissue Release on 2-Year Outcomes in Total Knee Arthroplasty. J Arthroplasty. 2022;37(10):2035-2040. [35] CHUNG BJ, KANG YG, CHANG CB, et al. Differences Between Sagittal Femoral Mechanical and Distal Reference Axes Should Be Considered in Navigated TKA. Clin Orthop Relat Res. 2009;467(9):2403-2413. [36] SHAWEN SB, BELMONT PJ, KLEMME WR, et al. Osteoporosis and Anterior Femoral Notching in Periprosthetic Supracondylar Femoral Fractures: A Biomechanical Analysis. J Bone Joint Surg Am. 2003;85(1):115-121. [37] MOON YW, HA CW, DO KH, et al. Comparison of Robot-Assisted and Conventional Total Knee Arthroplasty: A Controlled Cadaver Study Using Multiparameter Quantitative Three-Dimensional CT Assessment of Alignment. Comput Aided Surg. 2012;17(2):86-95. [38] SONG EK, SEON JK, YIM JH, et al. Robotic-Assisted TKA Reduces Postoperative Alignment Outliers and Improves Gap Balance Compared to Conventional TKA. Clin Orthop Relat Res. 2013;471(1):118-126. [39] SIRES JD, WILSON CJ. CT Validation of Intraoperative Implant Position and Knee Alignment as Determined by the MAKO Total Knee Arthroplasty System. J Knee Surg. 2021;34(10):1133-1137. [40] SCHOLL LY, HAMPP EL, DE SOUZA KM, et al. How Does Robotic-Arm Assisted Technology Influence Total Knee Arthroplasty Implant Placement for Surgeons in Fellowship Training? J Knee Surg. 2022; 35(2):198-203. [41] DECKEY DG, VERHEY JT, ROSENOW CS, et al. Robotic-Assisted Total Knee Arthroplasty Allows for Trainee Involvement and Teaching Without Lengthening Operative Time. J Arthroplasty. 2022;37(6S):S201-S206. [42] JUNG HJ, KANG MW, LEE JH, et al. Learning Curve of Robot-Assisted Total Knee Arthroplasty and Its Effects on Implant Position in Asian Patients: A Prospective Study. BMC Musculoskelet Disord. 2023;24(1):332. [43] MURPHY GT, SHATROV J, DUONG J, et al. How Does the Use of Quantified Gap-Balancing Affect Component Positioning and Limb Alignment in Robotic Total Knee Arthroplasty Using Functional Alignment Philosophy? A Comparison of Two Robotic Platforms. Int Orthop. 2023;47(5):1221-1232. [44] PATIL S, D’LIMA DD, FAIT JM, et al. Improving Tibial Component Coronal Alignment During Total Knee Arthroplasty With Use of a Tibial Planing Device. J Bone Joint Surg Am. 2007;89(2):381-387. [45] JENNY JY, CLEMENS U, KOHLER S, et al. Consistency of Implantation of a Total Knee Arthroplasty With a Non-Image-Based Navigation System: A Case-Control Study of 235 Cases Compared With 235 Conventionally Implanted Prostheses. J Arthroplasty. 2005;20(7):832-839. [46] AGARWAL N, TO K, MCDONNELL S, et al. Clinical and Radiological Outcomes in Robotic-Assisted Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. J Arthroplasty. 2020;35(11):3393-3409. [47] BECKER R, BONNIN M, HOFMANN S. The Painful Knee After Total Knee Arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19(9): 1409-1410. [48] CHIN BZ, TAN SSH, CHUA KCX, et al. Robot-Assisted Versus Conventional Total and Unicompartmental Knee Arthroplasty: A Meta-Analysis of Radiological and Functional Outcomes. J Knee Surg. 2021;34(10): 1064-1075. [49] ONGGO JR, ONGGO JD, DE STEIGER R, et al. Robotic-Assisted Total Knee Arthroplasty Is Comparable to Conventional Total Knee Arthroplasty: A Meta-Analysis and Systematic Review. Arch Orthop Trauma Surg. 2020;140(10):1533-1549. [50] ZHANG J, NDOU WS, NG N, et al. Robotic-Arm Assisted Total Knee Arthroplasty Is Associated With Improved Accuracy and Patient Reported Outcomes: A Systematic Review and Meta-Analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30(8):2677-2695. [51] CHANG JS, KAYANI B, WALLACE C, et al. Functional Alignment Achieves Soft-Tissue Balance in Total Knee Arthroplasty as Measured With Quantitative Sensor-Guided Technology. Bone Joint J. 2021;103-B(3): 507-514. [52] YOUNG SW, ZENG N, TAY ML, et al. A Prospective Randomised Controlled Trial of Mechanical Axis With Soft Tissue Release Balancing vs Functional Alignment With Bony Resection Balancing in Total Knee Replacement-A Study Using Stryker Mako Robotic Arm-Assisted Technology. Trials. 2022;23(1):580. [53] DIQUATTRO E, PRILL R, SALZMANN M, et al. High Three-Dimensional Accuracy of Component Placement and Lower Limb Alignment Using a Robotic Arm-Assisted System and Gap-Balancing Instrument in Total Knee Arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2024;32(3):685-692. [54] GLOWALLA C, LANGER S, LENZE U, et al. Postoperative Full Leg Radiographs Exhibit Less Residual Coronal Varus Deformity Compared to Intraoperative Measurements in Robotic Arm-Assisted Total Knee Arthroplasty With the MAKO™ System. Knee Surg Sports Traumatol Arthrosc. 2023;31(9):3912-3918. [55] SONG EK, SEON JK, PARK SJ, et al. Simultaneous Bilateral Total Knee Arthroplasty With Robotic and Conventional Techniques: A Prospective, Randomized Study. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1069-1076. [56] STIMSON LN, STEELMAN KR, HAMILTON DA, et al. Evaluation of Blood Loss in Conventional vs MAKOplasty Total Knee Arthroplasty. Arthroplast Today. 2022;16:224-228. [57] KAYANI B, KONAN S, PIETRZAK JRT, et al. Iatrogenic Bone and Soft Tissue Trauma in Robotic-Arm Assisted Total Knee Arthroplasty Compared With Conventional Jig-Based Total Knee Arthroplasty: A Prospective Cohort Study and Validation of a New Classification System. J Arthroplasty. 2018;33(8):2496-2501. [58] PARRATTE S, VAN OVERSCHELDE P, BANDI M, et al. An Anatomo-Functional Implant Positioning Technique With Robotic Assistance for Primary TKA Allows the Restoration of the Native Knee Alignment and a Natural Functional Ligament Pattern, With a Faster Recovery at 6 Months Compared to an Adjusted Mechanical Technique. Knee Surg Sports Traumatol Arthrosc. 2023;31(4):1334-1346. [59] MCEWEN P, BALENDRA G, DOMA K. Medial and Lateral Gap Laxity Differential in Computer-Assisted Kinematic Total Knee Arthroplasty. Bone Joint J. 2019;101-B(3):331-339. [60] NAKAMURA S, TIAN Y, TANAKA Y, et al. The Effects of Kinematically Aligned Total Knee Arthroplasty on Stress at the Medial Tibia: A Case Study for Varus Knee. Bone Joint Res. 2017;6(1):43-51. [61] TIAN R, DUAN X, KONG N, et al. Robotic-Assisted Total Knee Arthroplasty Is More Advantageous for Knees With Severe Deformity: A Randomized Controlled Trial Study Design. Int J Surg. 2023;109(3): 287-296. |
| [1] | Li Sa, Sun Ning, Sun Zhaozhong, Feng Zhimeng, Li Xuedong. Evaluation parameters and specific region of C6 nerve oppression by uncinate process degeneration [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2294-2302. |
| [2] | He Yixiang, Qiao Wanjia, Wang Wenji. Effectiveness and safety of tranexamic acid versus epsilon-aminocaproic acid in total hip and knee arthroplasties: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2361-2369. |
| [3] | Zhou Jian, Zhang Tao, Zhou Weili, Zhao Xingcheng, Wang Jun, Shen Jie, Qian Li, Lu Ming. Effects of resistance training on quadriceps mass and knee joint function in patients with osteoporosis and sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1081-1088. |
| [4] | Zhang Anqi, Hua Haotian, Cai Tianyuan, Wang Zicheng, Meng Zhuo, Zhan Xiaoqian, Chen Guoqian . Pain after total knee arthroplasty: current status and trend analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 795-804. |
| [5] | Zhou Feng, Fu Pengfei, Qian Yufan, Xu Pingcheng, Guo Jiongjiong, Zhang Lei. Correlation between spinal sagittal imbalance and knee joint parameters detected by whole-body EOS imaging [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 596-603. |
| [6] | Zhang Qian, Wang Fuxia, Wang Wen, Zhang Kun. Characteristic analysis of nanogel composite system and its application strategies in visualization of diagnostic imaging and therapy [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 480-488. |
| [7] | Li Chunchao, Julaiti·Maitirouzi, Xie Xuechen, Zhang Le, Wang Yixi, Paerhati·Rexiti. Finite element analysis of effect of passive support of deep intrinsic lumbar muscle groups on the lumbar spine [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(15): 3820-3831. |
| [8] | Liu Fei, Deng Xinheng, Cheng Yongzhong, Yin Xiaodong, Li Xiaomin, Zhu Shuchao, Wang Chaolu. Accuracy and stability of digital algorithm-based CT imaging recognition software in identifying AO-C2 type distal radius fractures [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(15): 3929-3935. |
| [9] | Li Zhongxian, Jiao Zitong, Ren Hanyue, Zhang Pan, Peng Min, Huang Yingxin, Li Mengyao, Hu Yuechen, Liang Junquan, Yan Luda, Fu Wenbin, Zhou Peng. Mechanism of depression with insomnia mediated by the locus coeruleus-norepinephrine system: an assessment based on resting-state functional magnetic resonance imaging [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 3083-3090. |
| [10] | Zhou Jinhai, Li Jiangwei, Wang Xuquan, Zhuang Ying, Zhao Ying, Yang Yuyong, Wang Jiajia, Yang Yang, Zhou Shilian. Three-dimensional finite element analysis of anterior femoral notching during total knee arthroplasty at different bone strengths [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1775-1782. |
| [11] | Miao Jiahang, Ma Sheng, Li Qupeng, Yu Huilin, Hu Tianyu, Gao Xiao, Feng Hu. Cervical lordosis ratio can be used as a decision-making indicator for selection of posterior surgical approach for multi-level cervical spondylotic myelopathy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1796-1802. |
| [12] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| [13] | Wen Zixing, Xu Xin, Zhu Shengqun. Correlations between gastrocnemius morphology parameters and physical activity capacity in elderly females under high-frequency ultrasound [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1058-1063. |
| [14] | Jiang Tao, Zhang Chuankai, Hao Liang, Liu Yong. MAKO robot- and navigation-assisted knee replacement: comparison of lower limb force alignment and prosthesis position accuracy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7150-7157. |
| [15] | Liu Ning, Sun Yingjin, Huang Long, Feng Shuo, Chen Xiangyang. Optimal rotational alignment of the tibial component during Oxford unicompartmental knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7158-7164. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||