Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (15): 3920-3928.doi: 10.12307/2026.727
Previous Articles Next Articles
Analysis of risk factors for secondary fractures after hip fracture surgery in the elderly
La Rui, Wu Qian, Zhang Zhongtai, Xu Wu, Ding Qingfeng, Zhang Zhigang, Jiang Dinghua, Huang Lixin, Wang Shenghao
- Department of Orthopedics, The First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China
-
Accepted:2025-06-27Online:2026-05-28Published:2025-11-07 -
Contact:Wang Shenghao, PhD, Attending physician, Department of Orthopedics, The First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China Huang Lixin, Associate professor, Doctoral supervisor, Chief physician, Department of Orthopedics, The First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China -
About author:La Rui, MS, Physician, Department of Orthopedics, The First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China Wu Qian, MD, Physician, Department of Orthopedics, The First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China La Rui and Wu Qian contributed equally to this article. -
Supported by:National Natural Science Foundation of China, No. 82102619 (to WSH); Jiangsu Provincial Traditional Chinese Medicine Science and Technology Development Project, No. ZD202232 (to HLX)
CLC Number:
Cite this article
La Rui, Wu Qian, Zhang Zhongtai, Xu Wu, Ding Qingfeng, Zhang Zhigang, Jiang Dinghua, Huang Lixin, Wang Shenghao. Analysis of risk factors for secondary fractures after hip fracture surgery in the elderly[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(15): 3920-3928.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
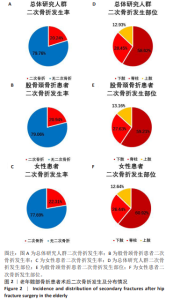
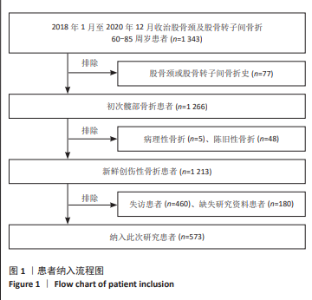
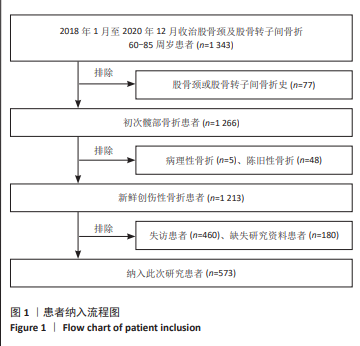
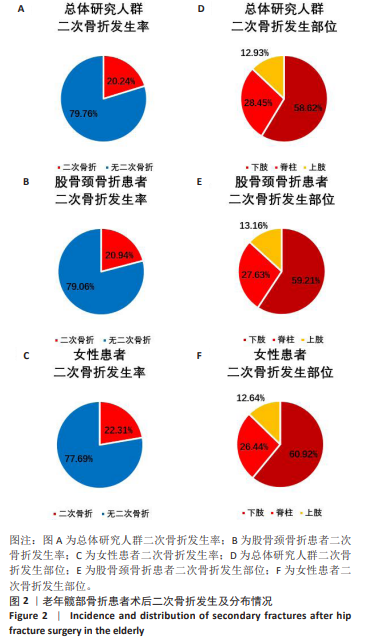
2.3 二次骨折的发生和分布概况 此次研究平均随访时间为(62.35±10.65)个月。 老年髋部骨折患者术后二次骨折的发生情况如图2所示,在纳入的573例患者中,116例患者发生二次骨折,二次骨折的总体发生率为20.2% (116/573)。二次骨折的发生部位及比例为:发生下肢骨折68例,占比58.6%(68/116);发生脊柱骨折33例,占比28.5%(33/116);发生上肢骨折15例,占比12.9%(15/116)。 初次髋部骨折为股骨颈骨折的患者共363例,其中76例患者发生二次骨折,发生率为20.9% (76/363)。二次骨折的发生部位及比例为:发生下肢骨折45例,占比59.2%(45/76);发生脊柱骨折21例,占比27.6%(21/76);发生上肢骨折10例,占比13.2%(10/76)。 女性患者共390例,其中87例患者发生二次骨折,发生率为22.3%(87/390)。二次骨折的发生部位及比例为:发生下肢骨折53例,占比60.9%(53/87);发生脊柱骨折23例,占比26.4%(23/87);发生上肢骨折11例,占比12.6%(11/87)。"

2.4 二次骨折组和无二次骨折组患者的基线资料比较 表2列举了二次骨折组和无二次骨折组患者的一般临床特征。二次骨折组和无二次骨折组患者在性别分布上无统计学差异(P > 0.05),但二次骨折组女性患者比例较高。年龄方面,二次骨折组患者年龄显著高于无二次骨折组患者(P < 0.01)。临床合并症方面,二次骨折组患者中合并脑血管疾病史以及帕金森病病史的患者比例显著高于无二次骨折组患者(P < 0.05)。二次骨折组患者中合并高血压病史、慢性呼吸系统疾病的患者比例高于无二次骨折组,但无统计学差异(P > 0.05)。此外,二次骨折组患者中合并糖尿病病史、心脏疾病史的患者比例低于无二次骨折组患者,但无统计学差异(P > 0.05)。"

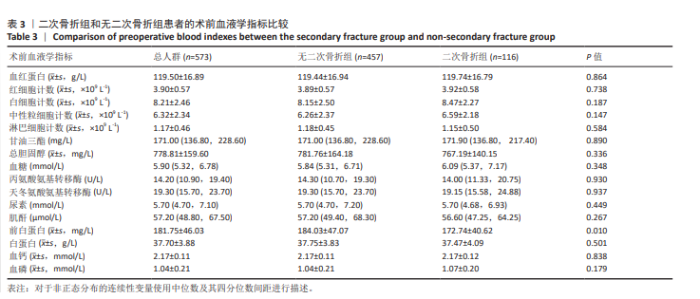
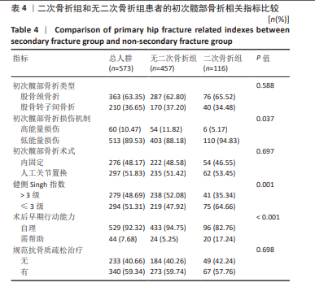
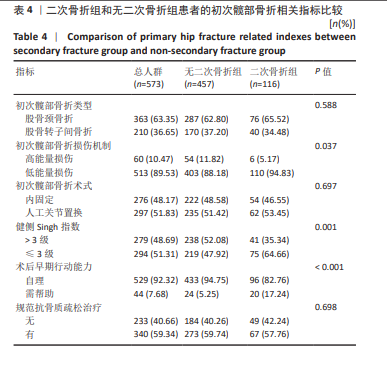
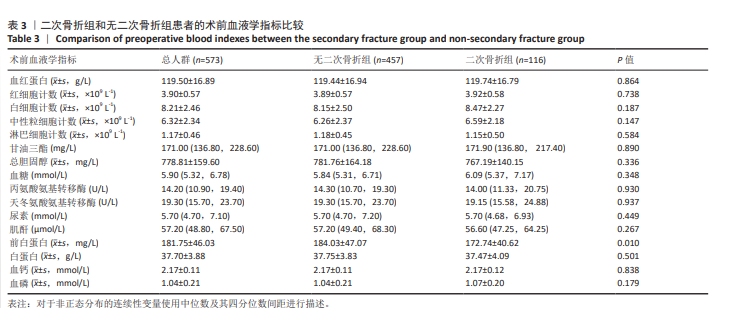
表3列举了二次骨折组和无二次骨折组患者的术前血液学指标。二次骨折组患者术前的前白蛋白水平显著低于无二次骨折组患者(P < 0.05)。还观察到二次骨折组患者术前的血红蛋白、红细胞计数、白细胞计数、中性粒细胞计数、甘油三酯、血糖、血磷水平高于无二次骨折组患者,但无统计学差异(P > 0.05)。此外,两组患者在淋巴细胞计数、总胆固醇、丙氨酸氨基转移酶、天冬氨酸氨基转移酶、尿素、肌酐、白蛋白和血钙水平之间的差异也均无显著性意义(P > 0.05)。 表4列举二次骨折组和无二次骨折组患者的初次髋部骨折相关指标。二次骨折组患者初次髋部骨折损伤机制为低能量损伤的患者比例显著高于无二次骨折组患者(P < 0.05);健侧Singh指数≤3级的患者比例显著高于无二次骨折组(P < 0.01);术后早期行动需帮助的患者比例显著高于无二次骨折组(P < 0.001)。二次骨折组患者初次髋部骨折术后进行规范抗骨质疏松的患者比例低于无二次骨折组患者,但差异无显著性意义(P > 0.05)。此外,没有观察到二次骨折组和无二次骨折组患者在初次髋部骨折类型和手术方式上的统计学差异(P > 0.05)。"
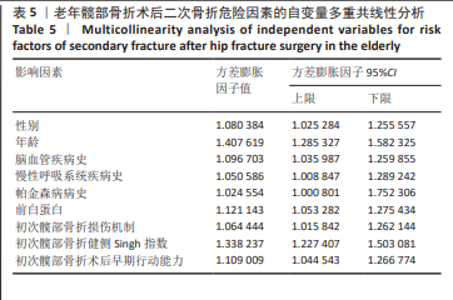
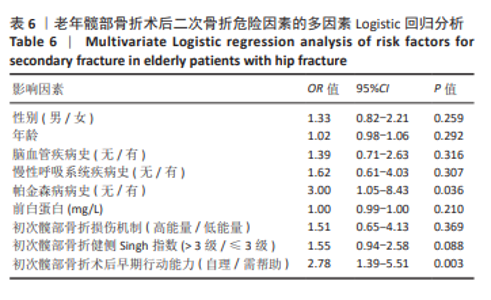
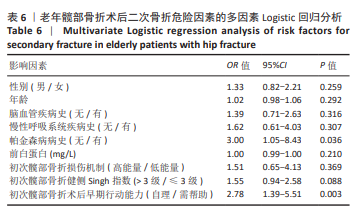
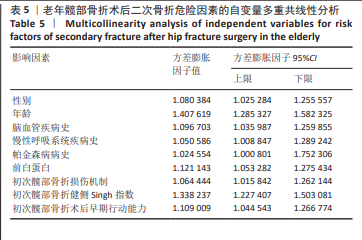
2.5 老年髋部骨折术后二次骨折危险因素的多因素Logistic回归分析 将下列指标作为自变量:性别、年龄、脑血管疾病史、慢性呼吸系统疾病史、帕金森病病史、术前的前白蛋白水平、初次髋部骨折损伤机制、初次髋部骨折健侧Singh指数、初次髋部骨折术后早期行动能力。多重共线性分析显示各指标间无显著的多重共线性(表5)。故以老年髋部骨折患者术后是否发生二次骨折为结局变量,以上述指标为自变量进行多因素Logistic回归分析,结果如表6所示。帕金森病病史(OR=3.00,95%CI:1.05-8.43,P=0.036)和初次髋部骨折术后早期行动需帮助(OR=2.78,95%CI:1.39-5.51,P=0.003)是术后二次骨折的独立危险因素。"
| [1] COLLABORATORS GBDF. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2021;2(9):e580-e592. [2] FENG JN, ZHANG CG, LI BH, et al. Global burden of hip fracture: The Global Burden of Disease Study. Osteoporos Int. 2024;35(1):41-52. [3] TAI TW, LIN YH, CHANG CJ, et al. The economic burden of hip fractures in Asia. Osteoporos Sarcopenia. 2021;7(2):45-46. [4] BAJI P, PATEL R, JUDGE A, et al. Organisational factors associated with hospital costs and patient mortality in the 365 days following hip fracture in England and Wales (REDUCE): a record-linkage cohort study. Lancet Healthy Longev. 2023;4(8):e386-e398. [5] ADEYEMI A, DELHOUGNE G. Incidence and Economic Burden of Intertrochanteric Fracture: A Medicare Claims Database Analysis. JB JS Open Access. 2019;4(1):e0045. [6] 张强, 李大伟, 刘凝昊, 等. 股骨转子间骨折行髓内钉治疗后营养风险预测模型的建立[J]. 中国组织工程研究,2024,28(21):3380-3384. [7] 夏冰, 张永华, 刘振鹏, 等. 老年股骨粗隆间骨折的组合微创半髋置换术[J]. 中国矫形外科杂志,2022,30(14):1303-1306. [8] GUZON-ILLESCAS O, PEREZ FERNANDEZ E, CRESPI VILLARIAS N, et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res. 2019;14(1):203. [9] HARVEY LA, PAYNE NL, TAN A, et al. Variation in mortality following hip fracture across the Asia Pacific region: Systematic review and proportional meta-analysis. Arch Gerontol Geriatr. 2024;126:105519. [10] SING CW, LIN TC, BARTHOLOMEW S, et al. Global Epidemiology of Hip Fractures: Secular Trends in Incidence Rate, Post-Fracture Treatment, and All-Cause Mortality. J Bone Miner Res. 2023;38(8):1064-1075. [11] MOHSENI V, FAHIMFAR N, ANSARIFAR A, et al. Mortality and re-fracture rates in low trauma hip fracture. BMC Geriatr. 2024;24(1):381. [12] HELYNEN N, RANTANEN L, LEHENKARI P, et al. Predisposing factors for a second fragile hip fracture in a population of 1130 patients with hip fractures, treated at Oulu University Hospital in 2013-2016: a retrospective study. Arch Orthop Trauma Surg. 2023;143(5):2261-2271. [13] VOCHTELOO AJ, BORGER VAN DER BURG BL, ROLING MA, et al. Contralateral hip fractures and other osteoporosis-related fractures in hip fracture patients: incidence and risk factors. An observational cohort study of 1,229 patients. Arch Orthop Trauma Surg. 2012;132(8): 1191-1197. [14] VAN DER STEENHOVEN TJ, STAFFHORST B, VAN DE VELDE SK, et al. Complications and institutionalization are almost doubled after second hip fracture surgery in the elderly patient. J Orthop Trauma. 2015;29(3):e103-108. [15] TREVISAN C, BEDOGNI M, PAVAN S, et al. The impact of second hip fracture on rehospitalization and mortality in older adults. Arch Gerontol Geriatr. 2020;90:104175. [16] LLOPIS-CARDONA F, ARMERO C, HURTADO I, et al. Incidence of Subsequent Hip Fracture and Mortality in Elderly Patients: A Multistate Population-Based Cohort Study in Eastern Spain. J Bone Miner Res. 2022;37(6):1200-1208. [17] CHEN M, LI Y, YANG Y, et al. Analysis of the risk factors for contralateral refracture after hip fracture surgery in elderly individuals: a retrospective study. J Orthop Surg Res. 2024;19(1):681. [18] ZHAO L, TIAN S, SHA W, et al. Analysis of the clinical characteristics and risk factors associated with contralateral hip fracture after initial hip fracture in elderly patients: a retrospective cohort study. Sci Rep. 2024;14(1):14292. [19] LIANG J, ZHANG J, LOU Z, et al. Development and validation of a predictive nomogram for subsequent contralateral hip fracture in elderly patients within 2 years after hip fracture surgery. Front Med (Lausanne). 2023;10:1263930. [20] RATNASAMY PP, RUDISILL KE, OGHENESUME OP, et al. Risk of Contralateral Hip Fracture Following Initial Hip Fracture Among Geriatric Fragility Fracture Patients. J Am Acad Orthop Surg Glob Res Rev. 2023;7(7):e23.00001. [21] 刘勇, 丁生权, 陈国川, 等. 老年髋部骨折术后对侧再骨折的独立风险因素分析 [J]. 中国骨与关节杂志,2021,10(9):649-654. [22] SONG M, WANG Y, JIANG Y, et al. Risk factors for subsequent fractures in hip fracture patients: a nested case-control study. J Orthop Surg Res. 2024;19(1):348. [23] JIANG Y, ZHU Y, ZHANG B, et al. Characteristics of subsequent contralateral proximal femoral fracture: more convenient access is needed to treat osteoporosis. J Orthop Surg Res. 2023;18(1):126. [24] 严广斌. Singh指数[J]. 中华关节外科杂志(电子版),2016,10(2): 236. [25] CHAU NVV, NGOC NM, NGUYET LA, et al. An observational study of breakthrough SARS-CoV-2 Delta variant infections among vaccinated healthcare workers in Vietnam. E Clin Med. 2021;41:101143. [26] ZHU Y, CHEN W, SUN T, et al. Epidemiological characteristics and outcome in elderly patients sustaining non-simultaneous bilateral hip fracture: a systematic review and meta-analysis. Geriatr Gerontol Int. 2015;15(1):11-18. [27] YAMANASHI A, YAMAZAKI K, KANAMORI M, et al. Assessment of risk factors for second hip fractures in Japanese elderly. Osteoporos Int. 2005;16(10):1239-1246. [28] FUKUSHIMA T, SUDO A, UCHIDA A. Bilateral hip fractures. J Orthop Sci. 2006;11(5):435-438. [29] OMSLAND TK, EMAUS N, TELL GS, et al. Ten-year risk of second hip fracture. A NOREPOS study. Bone. 2013;52(1):493-497. [30] GIBSON-SMITH D, KLOP C, ELDERS PJ, et al. The risk of major and any (non-hip) fragility fracture after hip fracture in the United Kingdom: 2000-2010. Osteoporos Int. 2014;25(11):2555-2563. [31] CHEN M, DU Y, TANG W, et al. Risk factors of mortality and second fracture after elderly hip fracture surgery in Shanghai, China. J Bone Miner Metab. 2022;40(6):951-959. [32] CHUANG PY, SHEN SH, YANG TY, et al. Non-steroidal anti-inflammatory drugs and the risk of a second hip fracture: a propensity-score matching study. BMC Musculoskelet Disord. 2016;17:201. [33] ZIDROU C, VASILIADIS AV, RIZOU S, et al. Second hip fracture in older adults: incidence and risk factors. Eur J Orthop Surg Traumatol. 2023; 33(5):1599-1606. [34] HARVEY L, TOSON B, MITCHELL R, et al. Incidence, timing and impact of comorbidity on second hip fracture: a population-based study. ANZ J Surg. 2018;88(6):577-581. [35] FIGUEROA CA, ROSEN CJ. Parkinson’s disease and osteoporosis: basic and clinical implications. Expert Rev Endocrinol Metab. 2020;15(3): 185-193. [36] TAN L, WANG Y, ZHOU L, et al. Parkinson’s disease and risk of fracture: a meta-analysis of prospective cohort studies. PLoS One. 2014;9(4): e94379. [37] GIBSON LL, WEINTRAUB D, LEMMEN R, et al. Risk of Dementia in Parkinson’s Disease: A Systematic Review and Meta-Analysis. Mov Disord. 2024;39(10):1697-1709. [38] LARRAINZAR-GARIJO R, DIEZ-PEREZ A, FERNANDEZ-TORMOS E, et al. Risk factors for a second nonsimultaneous hip fracture in a prospective cohort study. Arch Orthop Trauma Surg. 2022;142(10):2611-2617. [39] HJELHOLT TJ, JOHNSEN SP, BRYNNINGSEN PK, et al. Impact of Stroke History on the Risk of Recurrent Hip Fracture or Major Osteoporotic Fractures among Patients with Incident Hip Fracture: A Nationwide Cohort Study. J Bone Miner Res. 2023;38(2):278-287. [40] WANG L, YIN L, YANG M, et al. Muscle density is an independent risk factor of second hip fracture: a prospective cohort study. J Cachexia Sarcopenia Muscle. 2022;13(3):1927-1937. [41] WANG L, YANG M, GE Y, et al. Muscle size and density are independently associated with death after hip fracture: A prospective cohort study. J Cachexia Sarcopenia Muscle. 2023;14(4):1824-1835. [42] 中国加速康复外科专家组. 中国加速康复外科围术期管理专家共识(2016版)[J]. 中华消化外科杂志,2016,15(6):527-533. |
| [1] | Shi Yaozhou, Jia Fanglin, Zhang Heling, Song Hanlin, Gao Haoran, Gao Xiao, Sun Wei, Feng Hu. Establishment and validation of a prediction model for axial symptoms after laminectomy with lateral mass screw fixation [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2269-2277. |
| [2] | Zhang Zizheng, Luo Wang, Liu Changlu. Application value of finite element analysis on unicompartmental knee arthroplasty for medial knee compartmental osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2313-2322. |
| [3] | Zhao Feifan, Cao Yujing. Risk factors and coping strategies of internal fixation failure in treatment of intertrochanteric fracture with proximal femoral nail antirotation [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2323-2333. |
| [4] | Li Qingbin, Lin Jianhui, Huang Wenjie, Wang Mingshuang, Du Jiankai, Lao Yongqiang. Bone cement filling after enlarged curettage of giant cell tumor around the knee joint: a comparison of subchondral bone grafting and non-grafting [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1896-1902. |
| [5] | Sun Jiahe, Shi Jipeng, Zhu Tianrui, Quan Helong, Xu Hongqi. Effect of exercise intervention in elderly individuals with sarcopenia and its comorbidities: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 997-1007. |
| [6] | Ding Yu, Chen Jingwen, Chen Xiuyan, Shi Huimin, Yang Yudie, Zhou Meiqi, Cui Shuai, . Circulating inflammatory proteins and myocardial hypertrophy: large sample analysis of European populations from GWAS Catalog and FinnGen databases [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1047-1057. |
| [7] | Abuduwupuer·Haibier, Shang Qisong Song Xinghua. Analysis of factors for recurrent fractures of vertebral and adjacent vertebrae after osteoporotic compression fracture in the elderly patients with underlying diseases [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 642-651. |
| [8] | Yang Peng, Xu Chenghan, Zhou Yingjie, Chai Xubin, Zhuo Hanjie, Li Lin, Shi Jinyu. A meta-analysis of risk factors for residual back pain after vertebral augmentation for osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 731-739. |
| [9] | Wang Jiangjing, Zhao Na, Hu Xiaona, Zhao Na . Safety of 3D printed titanium alloy bone trabecular cup prosthesis combined with modified Kidney Tonifying and Blood Activating Decoction for elderly hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 612-619. |
| [10] | Zhang Junwei, Chen Lingling, Ma Zhenyuan, Nie Weizhi, Li Chaohui, Wang Haitao, Duan Laibao, Hou Jinyong, Bi Hongzheng. Three-dimensional displacement and risk factors of midshaft clavicle fractures treated with titanium elastic intramedullary nailing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 269-277. |
| [11] | Ma Le, Song Yuke, Zhong Xianxing, Zhang Wensheng. Risk factors for axial symptoms following posterior cervical laminoplasty: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(15): 3983-3992. |
| [12] | Wang Shijie, Hu Xiaoyu, Duan Zhuoran, Tang Yingfeng, Wang Wei . Association between grip strength to weight ratio and new-onset cardiovascular and cerebrovascular diseases: a big data analysis of the China Health and Retirement Longitudinal Study [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 3190-3197. |
| [13] | Wang Degang, , Chen Guohua, , Mei Junhua, Wang Junli, Zheng Li. Effects of nocturnal sleep duration on new-onset cardiovascular and cerebrovascular diseases in middle-aged and elderly patients with chronic comorbidities [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(11): 2814-2822. |
| [14] | Yan Wenjian, Li Yinghui, Zhang Yong. Daily diet and structural damage of the knee joint: a large-scale genetic analysis based on UK and FinnGen databases [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(11): 2877-2885. |
| [15] | Huang Fengqin, Hu Yalin, Yang Boyin, Luo Xingmei. Constructing a risk prediction nomogram model for cognitive impairment in hypertensive intracerebral hemorrhage [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(10): 2466-2474. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||