Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (13): 3435-3445.doi: 10.12307/2026.143
Previous Articles Next Articles
Mesenchymal stem cells and their exosomes in treatment of bronchopulmonary dysplasia
Huang Jia1, 2, Yan Qingyan1, 2, Yang Xing1, 2, Zhu Xiaoping1, 3, Luo Hongfang1, 2
- 1Department of Pediatrics, School of Clinical Medicine, Guizhou Medical University, Guiyang 550004, Guizhou Province, China; 2Department of Pediatrics, Second Affiliated Hospital, Guizhou Medical University, Kaili 556000, Guizhou Province, China; 3Department of Pediatrics, Affiliated Hospital, Guizhou Medical University, Guiyang 550004, Guizhou Province, China
-
Accepted:2025-08-05Online:2026-05-08Published:2025-12-26 -
Contact:Luo Hongfang, Chief physician, Master’s supervisor, Department of Pediatrics, School of Clinical Medicine, Guizhou Medical University, Guiyang 550004, Guizhou Province, China; Department of Pediatrics, Second Affiliated Hospital, Guizhou Medical University, Kaili 556000, Guizhou Province, China Co-corresponding author: Zhu Xiaoping, Chief physician, Doctoral supervisor, Department of Pediatrics, School of Clinical Medicine, Guizhou Medical University, Guiyang 550004, Guizhou Province, China; Department of Pediatrics, Affiliated Hospital, Guizhou Medical University, Guiyang 550004, Guizhou Province, China -
About author:Huang Jia, MS, Department of Pediatrics, School of Clinical Medicine, Guizhou Medical University, Guiyang 550004, Guizhou Province, China; Department of Pediatrics, Second Affiliated Hospital, Guizhou Medical University, Kaili 556000, Guizhou Province, China -
Supported by:Social Development Key Project of Guizhou Provincial Department of Science and Technology, No. [2020]4Y124 (to ZXP)
CLC Number:
Cite this article
Huang Jia, Yan Qingyan, Yang Xing, Zhu Xiaoping, Luo Hongfang. Mesenchymal stem cells and their exosomes in treatment of bronchopulmonary dysplasia[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(13): 3435-3445.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
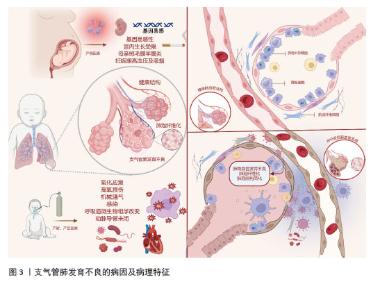
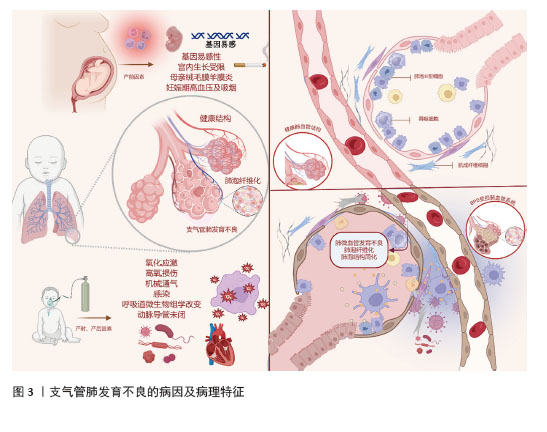
2.1 支气管肺发育不良概述 支气管肺发育不良最早由NORTHWAY等[3]于1967年提出,是一种复杂的多因素引起的肺损伤综合征。支气管肺发育不良的发生与产前、产时和产后3个阶段的多种因素密切相关,见图3。产前阶段的主要影响因素包括遗传易感性、宫内发育受限、母体绒毛膜羊膜炎、妊娠期高血压以及孕妇吸烟等[4];产时因素主要是胎龄和出生体质量,研究显示,早产儿胎龄越小、体质量越轻,发生支气管肺发育不良的概率越高,因此这两项指标被广泛认为是最具预测价值的危险因素[5];产后阶段则受氧化应激、高浓氧暴露、机械通气、感染、呼吸道菌群失调和动脉导管未闭等因素影响,这些因素容易引起肺部炎症、氧化应激损伤及实质纤维化,从而促使支气管肺发育不良的发生。支气管肺发育不良的主要特征为肺生长停滞、肺泡结构简化、血管发育受损和肺功能异常,对于肺仍处于肺管期向囊泡期过渡阶段的早产儿而言,这些病理改变会导致气体交换障碍,并引发严重的呼吸系统疾病。一项随访研究发现,支气管肺发育不良患儿不仅在婴儿期肺功能受损,哮喘患病率增加,同时还会对儿童期乃至成年期的肺功能产生深远影响[6]。据统计,在胎龄为22-24周的新生儿中,近80%被诊断患有支气管肺发育不良[7]。该疾病在早期死亡率较高,晚期则可能导致呼吸系统、循环系统乃至神经系统的长期并发症,严重影响患儿的生存预后和生活质量[8]。目前,针对支气管肺发育不良的治疗手段较为有限,常用药物包括外源性肺泡表面活性物质、抗氧化剂、糖皮质激素、抗氧化剂、维生素A、咖啡因、大环内酯类抗生素、利尿剂等[9]。然而,由于支气管肺发育不良牵涉复杂的病理生理机制,目前的治疗方案尚不能够完全预防或阻止肺损伤的进展,间充质干细胞作为未分化的基础细胞,能够在特定条件下诱导为修复受损或破坏组织所需的特定细胞类型,并具备自我更新能力[10]。在支气管肺发育不良的治疗中,间充质干细胞显示出了巨大的潜力。"
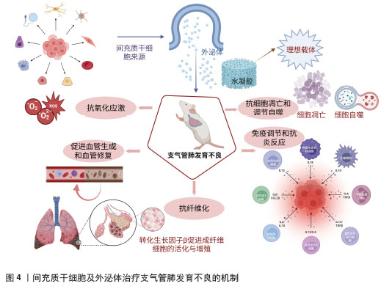
2.2 间充质干细胞及其外泌体在支气管肺发育不良中的潜在治疗作用 2.2.1 抗氧化应激 支气管肺发育不良是一种由出生时过早暴露于高氧环境所诱发的疾病。尽管胎儿的肺通常在子宫内低氧环境中发育,但对于极低出生体质量的婴儿而言,长期接受机械通气,或仅仅因暴露于相对较高的环境氧浓度,再加之肺部内源性抗氧化系统尚未发育成熟,使其更容易受到氧化应激损伤,从而加重支气管肺发育不良的发生和发展[11]。在肺间质中,脂肪成纤维细胞通过提供中性脂质,支持Ⅱ型肺泡上皮细胞合成磷脂,这一过程对未成熟胎儿肺部表面活性剂的合成至关重要。然而,氧化应激可诱导脂肪成纤维细胞向肌成纤维细胞转分化,导致Ⅱ型肺泡上皮细胞合成和分泌表面活性剂的能力下降[12]。此外,氧化应激还会诱导Ⅱ型肺泡上皮细胞过度凋亡并抑制其增殖,进一步阻碍肺泡上皮损伤的修复,影响肺泡的结构和功能恢复,从而加剧支气管肺发育不良的病理进程[13]。 氧气含量已被证明能够调节多种间充质干细胞的生长和分化。然而,在高氧暴露和机械通气条件下,肺部常驻间充质干细胞的功能会受到抑制。来自支气管肺发育不良新生儿气管抽吸样本的肺间充质干细胞显示,血小板衍生生长因子受体α和血管内皮生长因子等与肺泡发育及修复相关的生长因子表达水平明显下降[14-15]。相比之下,在缺氧环境下培养的骨髓间充质干细胞表现出更高的存活率、集落形成能力和分化潜力[16-18]。这表明氧化应激可能导致婴儿肺组织内常驻干细胞减少或功能障碍,从而影响肺泡的修复和再生。基于此,补充外源性干细胞及其衍生物成为支气管肺发育不良治疗的潜在策略。研究发现,与正常胎肺间充质干细胞相比,在缺氧条件下培养的人脐带间充质干细胞能够分泌相似水平的肺保护蛋白和生长因子,甚至在某些情况下其分泌水平更高。因此,移植人脐带间充质干细胞有望用于对抗高氧暴露对常驻肺细胞的损害[16]。然而,由于人脐带间充质干细胞未曾经历高氧环境,其在移植到接受高氧通气的肺部之后是否会遭受与常驻肺间充质干细胞相同的氧化应激损伤,目前尚缺乏明确的研究结论。 线粒体在细胞能量代谢和氧化应激中发挥核心作用,其结构、动力学、DNA完整性以及氧化代谢功能与支气管肺发育不良的发生密切相关[12]。研究表明,高氧暴露会导致线粒体损伤,从而成为肺结构简化和支气管肺发育不良发生的重要致病因素[19]。高氧环境不仅抑制肺线粒体的生物能量功能,还损害肺损伤动物模型的肺泡发育[20]。线粒体DNA对氧化损伤极为敏感,高氧诱导的线粒体DNA损伤会抑制大鼠肺外植体的分支形态发生,从而影响肺泡成熟。在早产儿中,血管内皮细胞的线粒体生物能量功能障碍、活性氧生成紊乱以及线粒体DNA损伤会破坏正常的肺部发育[21]。因此,线粒体功能不仅可能影响支气管肺发育不良的发生发展,还可作为支气管肺发育不良早产儿长期预后和死亡率的重要预测因子[22]。针对线粒体损伤的修复策略已成为支气管肺发育不良研究的重要方向。间充质干细胞可通过外泌体主动分泌线粒体,并将其转移至受体细胞,从而实现线粒体功能的恢复。这一机制为受损肺细胞提供健康线粒体,促进细胞功能修复,并改善肺组织的生理状态[23-24]。研究表明,在急性呼吸窘迫综合征动物模型中,间充质干细胞衍生外泌体可通过线粒体转移改善损伤肺组织的肺泡-毛细血管屏障功能[25]。此外,骨髓间充质干细胞可依赖间隙连接蛋白43介导的肺泡附着及线粒体转移,恢复肺泡的生物能量学平衡,从而减轻脂多糖诱导的急性肺损伤[26]。同时,间充质干细胞还能通过旁分泌信号分子及外泌体促进受损肺细胞的线粒体复制,进一步增强肺组织的修复能力[23-24]。 2.2.2 促进血管生成和血管修复 在支气管肺发育不良患儿中,血管生成受抑制被认为是导致肺泡简化的主要机制,肺微血管发育不良使毛细血管密度降低,血液循环横截面积减小,最后导致气体交换表面积减小。因此,促进肺血管生成和修复血管损伤是缓解支气管肺发育不良的关键。血管内皮生长因子是一种高度特异性的血管内皮细胞有丝分裂原,是血管生成的中心调节因子。血管内皮生长因子还能促进Ⅱ型肺泡上皮细胞的生长和分化,而这些细胞正是合成和分泌肺表面活性物质的关键细胞类型。因此,血管内皮生长因子在调节血管生成和肺泡发育中发挥重要作用[27]。间充质干细胞及其外泌体可通过调控血管内皮生长因子表达参与血管损伤的修复过程。ZHANG等[28]发现,来自人脐带间充质干细胞的外泌体可激活磷脂酰肌醇3激酶/蛋白激酶B/哺乳动物雷帕霉素靶蛋白途径,通过上调缺氧诱导因子1α(一种已知的血管内皮生长因子合成调节因子)来增强血管内皮生长因子的表达,促进血管生成。值得注意的是,联合应用超氧化物歧化酶拟似剂四甲基哌啶与外泌体的治疗策略,能够进一步增强上述促血管生成和修复的效果[29]。CHOU等[30]通过动物实验发现,在支气管肺发育不良大鼠模型中,连续每日经气管给予肺表面活性剂联合人脐带间充质干细胞可显著上调血管内皮生长因子和血小板衍生生长因子受体蛋白的表达水平,缓解高氧诱导下的肺泡形成障碍及血管生成受损。值得注意的是,较高剂量的人脐带间充质干细胞相较于低剂量更有效地增强了治疗效果,表明间充质干细胞对修复效果具有剂量依赖性,间充质干细胞联合治疗策略在促进支气管肺发育不良的肺部血管及结构发育方面具有显著潜力。非编码RNA家族作为内皮细胞功能的关键调节因子,在血管生成过程中发挥着重要作用[31]。基因分析结果表明,间充质干细胞外泌体富含大量促进血管生成的miRNA[32]。QU等[33]发现,源自人脐带间充质干细胞外泌体的miR-126-3p通过靶向磷酸肌醇3激酶调节亚基2/磷脂酰肌醇3激酶/蛋白激酶B/哺乳动物雷帕霉素靶蛋白信号途径来启动血管生成程序,在体外实验中,miR-126-3p能显著增强血管生成因子信号,进一步促进血管生成。此外,研究还表明,来源于人脐带间充质干细胞的外泌体所携带的miR-126-3p在大鼠体内表现出抗细胞凋亡作用,凸显了其在治疗中的潜力和应用前景。B型利钠肽(B-type natriuretic peptide,BNP)是一种具有刺激内皮细胞再生作用的新生血管因子。MOREIRA等[34]的研究显示,通过鼻内途径给予新生大鼠人脐带组织来源间充质干细胞可显著上调B型利钠肽编码基因NPPB的表达,进而改善支气管肺发育不良动物模型的肺泡发育和肺血管生成。此外,在深Ⅱ度烧伤的大鼠模型中,研究发现人脐带间充质干细胞来源外泌体能够通过递送血管生成素2,显著增强血管生成[35]。 2.2.3 抗纤维化 纤维化是指在炎症反应或组织损伤过程中,纤维结缔组织及细胞外基质成分(如胶原蛋白和纤连蛋白)在病变区域及其周围组织中的异常沉积,最终导致不可逆的瘢痕形成,并持续损害器官功能[36],肺纤维化是支气管肺发育不良患儿的显著病理特征之一。间充质干细胞及其衍生的外泌体能够减少细胞外基质过度沉积以及促进组织再生,在抑制和修复肺纤维化过程中发挥了关键作用,显示出良好的治疗潜力。 转化生长因子β在炎症调节、细胞增殖与分化以及组织修复等过程中发挥着多种稳态调控作用[37]。大量研究表明,转化生长因子β能够促进成纤维细胞的活化与增殖,导致细胞外基质过度沉积,是肺纤维化形成的主要驱动因子之一[38],见图4。转化生长因子β表达水平的升高常与肺纤维化的严重程度密切相关[39]。肿瘤坏死因子α刺激基因6通过抑制转化生长因子β信号通路来调节成纤维细胞的生长,从而发挥抗纤维化作用[40],GONG等[41]发现间充质干细胞与巨噬细胞在炎症环境下共培养,其肿瘤坏死因子α刺激基因6分泌增加,从而减轻转化生长因子β所介导的纤维化。此外,来源于人脐带间充质干细胞的外泌体中富含的miRNA let-7i-5p可通过靶向调控转化生长因子β受体1/Smad3信号通路,有效抑制成纤维细胞活化,缓解二氧化硅诱导的肺纤维化[42]。SUN等[43-44]进一步发现,间充质干细胞来源外泌体所携带的miRNA let-7 不仅可减少胶原纤维的沉积、转化生长因子β及抗纤维化肝细胞生长因子的表达,还可抑制抗凋亡基因 Bcl-2、铁死亡相关蛋白及线粒体DNA损伤标志物的表达,从而在多个水平上发挥抗纤维化作用,其中核因子E2相关因子2信号通路参与了上述过程。内皮-间充质转化是指内皮细胞丧失其特有的细胞标志和功能,转而获得间充质细胞表型和特性的生物学过程,是特发性肺纤维化的致病机制。ZHAO等[45]的研究发现,人脐带间充质干细胞来源外泌体分泌的miR-218能够通过下调表观遗传转录抑制因子甲基化CpG结合蛋白2来抑制转化生长因子β1诱导的内皮-间充质转化,延缓肺纤维化进展。"
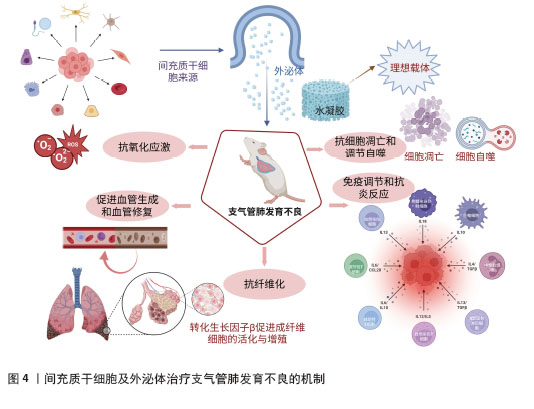

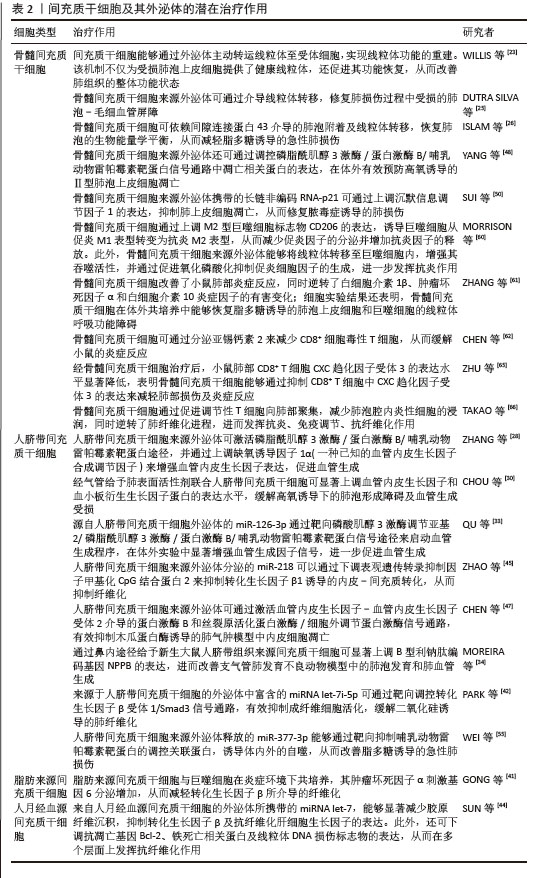
2.2.4 抗细胞凋亡和调节自噬 由于早产儿抗氧化系统功能失调,体内过量的活性氧无法及时消耗,从而攻击生物膜并传播脂质过氧化连锁反应,最后导致细胞凋亡[46]。因此,靶向抑制细胞凋亡是一种具有潜力的支气管肺发育不良治疗策略。CHEN等[47]证实,间充质干细胞来源外泌体可通过激活血管内皮生长因子-血管内皮生长因子受体2介导的蛋白激酶B和丝裂原活化蛋白激酶/细胞外调节蛋白激酶信号通路,有效抑制木瓜蛋白酶诱导的肺血管内皮细胞的凋亡。此外,YANG等[48]的研究表明,间充质干细胞来源外泌体还可通过调控磷脂酰肌醇3激酶/蛋白激酶B/哺乳动物雷帕霉素靶蛋白信号通路中凋亡相关蛋白的表达,在体外有效预防高氧诱导的Ⅱ型肺泡上皮细胞凋亡。RNA通过转录后调节基因表达在各种生物学功能(包括细胞凋亡、增殖和分化)中发挥关键作用[49]。SUI等[50]发现,骨髓间充质干细胞来源外泌体携带的长链非编码RNA-p21可通过上调沉默信息调节因子1的表达,抑制肺上皮细胞凋亡,从而修复脓毒症诱导的肺损伤。尽管间充质干细胞及其外泌体在多种疾病模型中已被证实具有抗凋亡作用,但其在支气管肺发育不良相关肺损伤中的具体机制仍有待深入研究。 自噬是一种细胞自我降解机制,通过将细胞内的有害或受损组分运送至溶酶体进行降解,从而维持细胞内环境的稳态[51]。适度自噬水平可以促进细胞功能和体内平衡,从而延长细胞寿命并改善肺部健康[52]。LI等[53]发现,支气管肺发育不良模型新生大鼠自噬标志物轻链3β水平上调,表明自噬可能在支气管肺发育不良的发展中发挥作用。尽管确切的机制尚不清楚,但已有研究表明自噬在间充质干细胞介导的肺组织再生中发挥关键作用,见图3。SURESHBABU等[54]的一项研究证明,哺乳动物雷帕霉素靶蛋白的调控关联蛋白(regulatory-associated protein of mechanistic target of rapamycin,RPTOR)作为高氧诱导的急性肺损伤和新生儿支气管肺发育不良的潜在治疗靶点,靶向抑制哺乳动物雷帕霉素靶蛋白的调控关联蛋白可增强新生小鼠的自噬活性并减少细胞凋亡,从而有效预防高氧诱导的肺损伤。WEI等[55]发现,人脐带间充质干细胞来源外泌体携带的miR-377-3p能够通过靶向抑制哺乳动物雷帕霉素靶蛋白的调控关联蛋白,诱导体内外自噬,从而改善脂多糖诱导的急性肺损伤。此外,过表达miR-377-3p的骨髓间充质干细胞外泌体相较于人胎肺成纤维细胞来源外泌体,在抑制支气管肺泡灌洗液中炎症因子方面表现出更强的效果,并显著增强自噬水平。 2.2.5 免疫调节和抗炎反应 免疫失衡和炎症反应是影响支气管肺发育不良疾病发展的重要病理生理过程,对支气管肺发育不良动物模型肺免疫细胞的转录组学分析显示,与趋化因子介导的信号传导和免疫细胞趋化相关的基因显著上调,同时与多种T淋巴细胞功能相关的基因则呈下调趋势[56]。间充质干细胞通过调节免疫反应和拮抗炎症可延缓支气管肺发育不良[23]。具体而言,间充质干细胞可以通过细胞接触和旁分泌机制来调节免疫细胞的功能。一方面,间充质干细胞通过细胞表面表达程序性死亡配体1和Fas配体等免疫抑制特性分子,与免疫细胞表面的受体结合,从而抑制免疫细胞的活性,导致其功能丧失[57];另一方面,间充质干细胞还可以直接作用于免疫细胞,抑制其活性和增殖。间充质干细胞能够调节多种免疫细胞的功能,包括中性粒细胞、调节性T细胞、效应T细胞、巨噬细胞和树突状细胞[58],这些细胞在多种炎症性肺病的发生机制中起重要作用。因此,间充质干细胞通过调控先天性及适应性免疫系统中的淋巴细胞,发挥免疫调节和抗炎作用。 树突状细胞和间充质干细胞之间的相互作用可使树突状细胞形成耐受性表型,并诱导炎性M1巨噬细胞极化为免疫抑制性M2巨噬细胞,从而促进某些抗炎因子如白细胞介素10和转化生长因子β的产生,并下调巨噬细胞和树突状细胞中炎症因子和细胞因子的分泌,包括白细胞介素1β、肿瘤坏死因子α、白细胞介素12,这些调节作用对于炎症消退及组织再生修复至关重要[59]。MORRISON等[60]研究发现,骨髓间充质干细胞通过上调M2表型标志物CD206的表达,诱导巨噬细胞由促炎性的M1表型向抗炎性的M2表型转化,从而减少促炎因子的释放并增加抗炎因子的分泌。此外,间充质干细胞来源外泌体还能够将线粒体转移至巨噬细胞内,增强其吞噬活性,并通过促进氧化磷酸化抑制促炎细胞因子的产生。由于强大的抗炎和免疫抑制作用,间充质干细胞在减轻炎症和促进肺组织损伤后的再生修复方面具有显著的临床意义。ZHANG等[61]发现,骨髓间充质干细胞改善了小鼠肺部炎症反应,同时逆转了白细胞介素1β、肿瘤坏死因子α和白细胞介素10等炎症因子的有害变化;细胞实验结果还表明,骨髓间充质干细胞在体外共培养中能够恢复脂多糖诱导的肺泡上皮细胞和巨噬细胞的线粒体呼吸功能障碍,进一步支持了间充质干细胞在炎症相关肺损伤修复中的潜在应用价值。CD8+ T细胞浸润增加可加剧肺部炎症反应及组织损伤,而抑制CD8+ T细胞活性有助于改善疾病进程。研究表明,骨髓间充质干细胞可通过分泌亚锡钙素2来减少CD8+ T细胞,从而缓解小鼠的炎症反应[62]。CXC趋化因子受体3是CD8+ T细胞迁移到多种组织的重要趋化因子受体,尤其是在炎症和感染状态下[63],其表达显著增强CD8+ T细胞的细胞毒作用,并促进γ-干扰素的产生[64]。ZHU等[65]发现,经骨髓间充质干细胞治疗后,小鼠肺部CD8+ T细胞CXC趋化因子受体3的表达水平显著降低,表明骨髓间充质干细胞能够通过抑制CD8+ T细胞中CXC趋化因子受体3的表达来减轻肺部损伤及炎症反应。调节性T细胞在炎症消退和肺组织修复中同样发挥关键作用,并促进肺泡上皮细胞的增殖。研究发现,骨髓间充质干细胞通过促进调节性T细胞向肺部聚集,减少肺泡腔内炎性细胞的浸润,同时逆转了肺纤维化进程,进而发挥抗炎、免疫调节、抗纤维化作用[66]。 间充质干细胞及其外泌体的潜在治疗作用,见表2。"
| [1] ZHUO Y, LI WS, LU W, et al. TGF-β1 mediates hypoxia-preconditioned olfactory mucosa mesenchymal stem cells improved neural functional recovery in Parkinson’s disease models and patients. Mil Med Res. 2024; 11(1):48. [2] HUANG R, CHEN T, WANG S, et al. Mesenchymal Stem Cells for Prophylaxis of Chronic Graft-vs-Host Disease After Haploidentical Hematopoietic Stem Cell Transplant: An Open-Label Randomized Clinical Trial. JAMA Oncol. 2024;10(2):220-226. [3] NORTHWAY WH JR, ROSAN RC, PORTER DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med. 1967;276(7):357-368. [4] YU H, LI D, ZHAO X, et al. Fetal origin of bronchopulmonary dysplasia: contribution of intrauterine inflammation. Mol Med. 2024;30(1):135. [5] 张珂,饶兴愉.新生儿呼吸窘迫综合征患儿发生支气管肺发育不良的Nomogram预测模型的建立与评估[J].重庆医科大学学报,2024,49(10):1110-1118. [6] FAWKE J, LUM S, KIRKBY J, et al. Lung function and respiratory symptoms at 11 years in children born extremely preterm: the EPICure study. Am J Respir Crit Care Med. 2010;182(2):237-245. [7] YOUNGE N, GOLDSTEIN RF, BANN CM, et al. Survival and Neurodevelopmental Outcomes among Periviable Infants. N Engl J Med. 2017;376(7):617-628. [8] 周应祯,王婷,付星梦,等.支气管肺发育不良的预后[J].中国当代儿科杂志, 2025,27(1):115-120. [9] ENZER KG, BAKER CD, WISNIEWSKI BL. Bronchopulmonary Dysplasia. Clin Chest Med. 2024;45(3):639-650. [10] ZAKRZEWSKI W, DOBRZYŃSKI M, SZYMONOWICZ M, et al. Stem cells: past, present, and future. Stem Cell Res Ther. 2019;10(1):68. [11] KIMBLE A, ROBBINS ME, PEREZ M. Pathogenesis of Bronchopulmonary Dysplasia: Role of Oxidative Stress from ‘Omics’ Studies. Antioxidants (Basel). 2022;11(12):2380. [12] XUEFEI Y, XINYI Z, QING C, et al. Effects of Hyperoxia on Mitochondrial Homeostasis: Are Mitochondria the Hub for Bronchopulmonary Dysplasia? Front Cell Dev Biol. 2021;9:642717. [13] WU D, LIANG M, DANG H, et al. Hydrogen protects against hyperoxia-induced apoptosis in type II alveolar epithelial cells via activation of PI3K/Akt/Foxo3a signaling pathway. Biochem Biophys Res Commun. 2018;495(2):1620-1627. [14] MÖBIUS MA, FREUND D, VADIVEL A, et al. Oxygen Disrupts Human Fetal Lung Mesenchymal Cells. Implications for Bronchopulmonary Dysplasia. Am J Respir Cell Mol Biol. 2019;60(5):592-600. [15] POPOVA AP, BENTLEY JK, CUI TX, et al. Reduced platelet-derived growth factor receptor expression is a primary feature of human bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol. 2014; 307(3):L231-L239. [16] POPOVA AP. Mesenchymal Cells and Bronchopulmonary Dysplasia: New Insights about the Dark Side of Oxygen. Am J Respir Cell Mol Biol. 2019;60(5): 501-502. [17] LEIJTEN J, GEORGI N, MOREIRA TEIXEIRA L, et al. Metabolic programming of mesenchymal stromal cells by oxygen tension directs chondrogenic cell fate. Proc Natl Acad Sci U S A. 2014; 111(38):13954-13959. [18] KRINNER A, ZSCHARNACK M, BADER A, et al. Impact of oxygen environment on mesenchymal stem cell expansion and chondrogenic differentiation. Cell Prolif. 2009;42(4):471-484. [19] NARALA VR, FUKUMOTO J, HERNÁNDEZ-CUERVO H, et al. Akap1 genetic deletion increases the severity of hyperoxia-induced acute lung injury in mice. Am J Physiol Lung Cell Mol Physiol. 2018; 314(5):L860-L870. [20] RATNER V, SOSUNOV SA, NIATSETSKAYA ZV, et al. Mechanical ventilation causes pulmonary mitochondrial dysfunction and delayed alveolarization in neonatal mice. Am J Respir Cell Mol Biol. 2013; 49(6):943-950. [21] 李梦曌,孙文强,朱雪萍.线粒体功能障碍在早产儿支气管肺发育不良发病机制中的研究进展[J].临床肺科杂志,2024, 29(7):1089-1092. [22] KANDASAMY J, OLAVE N, BALLINGER SW, et al. Vascular Endothelial Mitochondrial Function Predicts Death or Pulmonary Outcomes in Preterm Infants. Am J Respir Crit Care Med. 2017; 196(8):1040-1049. [23] WILLIS GR, FERNANDEZ-GONZALEZ A, ANASTAS J, et al. Mesenchymal Stromal Cell Exosomes Ameliorate Experimental Bronchopulmonary Dysplasia and Restore Lung Function through Macrophage Immunomodulation. Am J Respir Crit Care Med. 2018;197(1):104-116. [24] PHINNEY DG, DI GIUSEPPE M, NJAH J, et al. Mesenchymal stem cells use extracellular vesicles to outsource mitophagy and shuttle microRNAs. Nat Commun. 2015;6:8472. [25] DUTRA SILVA J, SU Y, CALFEE CS, et al. Mesenchymal stromal cell extracellular vesicles rescue mitochondrial dysfunction and improve barrier integrity in clinically relevant models of ARDS. Eur Respir J. 2021;58(1):2002978. [26] ISLAM MN, DAS SR, EMIN MT, et al. Mitochondrial transfer from bone-marrow-derived stromal cells to pulmonary alveoli protects against acute lung injury. Nat Med. 2012;18(5):759-765. [27] YUN EJ, LORIZIO W, SEEDORF G, et al. VEGF and endothelium-derived retinoic acid regulate lung vascular and alveolar development. Am J Physiol Lung Cell Mol Physiol. 2016;310(4):L287-L298. [28] ZHANG Y, HAO Z, WANG P, et al. Exosomes from human umbilical cord mesenchymal stem cells enhance fracture healing through HIF-1α-mediated promotion of angiogenesis in a rat model of stabilized fracture. Cell Prolif. 2019;52(2):e12570. [29] WANG J, ZHANG A, HUANG F, et al. MSC-EXO and tempol ameliorate bronchopulmonary dysplasia in newborn rats by activating HIF-1α. Pediatr Pulmonol. 2023;58(5):1367-1379. [30] CHOU HC, CHANG CH, CHEN CH, et al. Consecutive daily administration of intratracheal surfactant and human umbilical cord-derived mesenchymal stem cells attenuates hyperoxia-induced lung injury in neonatal rats. Stem Cell Res Ther. 2021;12(1):258. [31] ZHAO H, WANG X, FANG B. HIF1A promotes miR-210/miR-424 transcription to modulate the angiogenesis in HUVECs and HDMECs via sFLT1 under hypoxic stress. Mol Cell Biochem. 2022;477(8):2107-2119. [32] ZOU XY, YU Y, LIN S, et al. Comprehensive miRNA Analysis of Human Umbilical Cord-Derived Mesenchymal Stromal Cells and Extracellular Vesicles. Kidney Blood Press Res. 2018;43(1):152-161. [33] QU Q, LIU L, CUI Y, et al. miR-126-3p containing exosomes derived from human umbilical cord mesenchymal stem cells promote angiogenesis and attenuate ovarian granulosa cell apoptosis in a preclinical rat model of premature ovarian failure. Stem Cell Res Ther. 2022;13(1):352. [34] MOREIRA A, WINTER C, JOY J, et al. Intranasal delivery of human umbilical cord Wharton’s jelly mesenchymal stromal cells restores lung alveolarization and vascularization in experimental bronchopulmonary dysplasia. Stem Cells Transl Med. 2020;9(2):221-234. [35] LIU J, YAN Z, YANG F, et al. Exosomes Derived from Human Umbilical Cord Mesenchymal Stem Cells Accelerate Cutaneous Wound Healing by Enhancing Angiogenesis through Delivering Angiopoietin-2. Stem Cell Rev Rep. 2021;17(2):305-317. [36] ANTAR SA, ASHOUR NA, MARAWAN ME, et al. Fibrosis: Types, Effects, Markers, Mechanisms for Disease Progression, and Its Relation with Oxidative Stress, Immunity, and Inflammation. Int J Mol Sci. 2023;24(4):4004. [37] MASSAGUÉ J, SHEPPARD D. TGF-β signaling in health and disease. Cell. 2023; 186(19):4007-4037. [38] REN LL, LI XJ, DUAN TT, et al. Transforming growth factor-β signaling: From tissue fibrosis to therapeutic opportunities. Chem Biol Interact. 2023;369:110289. [39] ONG CH, THAM CL, HARITH HH, et al. TGF-β-induced fibrosis: A review on the underlying mechanism and potential therapeutic strategies. Eur J Pharmacol. 2021;911:174510. [40] USUNIER B, BROSSARD C, L’HOMME B, et al. HGF and TSG-6 Released by Mesenchymal Stem Cells Attenuate Colon Radiation-Induced Fibrosis. Int J Mol Sci. 2021;22(4):1790. [41] GONG SC, YOON Y, JUNG PY, et al. Antifibrotic TSG-6 Expression Is Synergistically Increased in Both Cells during Coculture of Mesenchymal Stem Cells and Macrophages via the JAK/STAT Signaling Pathway. Int J Mol Sci. 2022; 23(21):13122. [42] PARK SA, KIM MJ, PARK SY, et al. EW-7197 inhibits hepatic, renal, and pulmonary fibrosis by blocking TGF-β/Smad and ROS signaling. Cell Mol Life Sci. 2015;72(10):2023-2039. [43] SUN L, HE X, KONG J, et al. Menstrual blood-derived stem cells exosomal miR-let-7 to ameliorate pulmonary fibrosis through inhibiting ferroptosis by Sp3/HDAC2/Nrf2 signaling pathway. Int Immunopharmacol. 2024;126:111316. [44] SUN L, ZHU M, FENG W, et al. Exosomal miRNA Let-7 from Menstrual Blood-Derived Endometrial Stem Cells Alleviates Pulmonary Fibrosis through Regulating Mitochondrial DNA Damage. Oxid Med Cell Longev. 2019;2019:4506303. [45] ZHAO Y, DU L, SUN J, et al. Exosomal miR-218 derived from mesenchymal stem cells inhibits endothelial-to-mesenchymal transition by epigenetically modulating of BMP2 in pulmonary fibrosis. Cell Biol Toxicol. 2023;39(6):2919-2936. [46] SU LJ, ZHANG JH, GOMEZ H, et al. Reactive Oxygen Species-Induced Lipid Peroxidation in Apoptosis, Autophagy, and Ferroptosis. Oxid Med Cell Longev. 2019;2019:5080843. [47] CHEN Q, LIN J, DENG Z, et al. Exosomes derived from human umbilical cord mesenchymal stem cells protect against papain-induced emphysema by preventing apoptosis through activating VEGF-VEGFR2-mediated AKT and MEK/ERK pathways in rats. Regen Ther. 2022;21:216-224. [48] YANG W, HUANG C, WANG W, et al. Bone mesenchymal stem cell-derived exosomes prevent hyperoxia-induced apoptosis of primary type II alveolar epithelial cells in vitro. PeerJ. 2022;10:e13692. [49] TAN BWQ, SIM WL, CHEONG JK, et al. MicroRNAs in chronic airway diseases: Clinical correlation and translational applications. Pharmacol Res. 2020;160:105045. [50] SUI X, LIU W, LIU Z. Exosomal lncRNA-p21 derived from mesenchymal stem cells protects epithelial cells during LPS-induced acute lung injury by sponging miR-181. Acta Biochim Biophys Sin (Shanghai). 2021; 53(6):748-757. [51] CHEN T, ZHENG L, LUO P, et al. Crosstalk between m6A modification and autophagy in cancer. Cell Biosci. 2024;14(1):44. [52] ZHANG Y, ZHANG J, FU Z. Role of autophagy in lung diseases and ageing. Eur Respir Rev. 2022;31(166):220134. [53] LI M, PAN B, SHI Y, et al. Increased expression of CHOP and LC3B in newborn rats with bronchopulmonary dysplasia. Int J Mol Med. 2018;42(3):1653-1665. [54] SURESHBABU A, SYED M, DAS P, et al. Inhibition of Regulatory-Associated Protein of Mechanistic Target of Rapamycin Prevents Hyperoxia-Induced Lung Injury by Enhancing Autophagy and Reducing Apoptosis in Neonatal Mice. Am J Respir Cell Mol Biol. 2016;55(5):722-735. [55] WEI X, YI X, LV H, et al. Correction: MicroRNA-377-3p released by mesenchymal stem cell exosomes ameliorates lipopolysaccharide-induced acute lung injury by targeting RPTOR to induce autophagy. Cell Death Dis. 2020;11(9):746. [56] SHRESTHA D, YE GX, STABLEY D, et al. Pulmonary immune cell transcriptome changes in double-hit model of BPD induced by chorioamnionitis and postnatal hyperoxia. Pediatr Res. 2021;90(3):565-575. [57] WANG Y, HUANG R, LU Y, et al. Immuno-protective vesicle-crosslinked hydrogel for allogenic transplantation. Nat Commun. 2024;15(1):5176. [58] HUANG Y, WU Q, TAM PKH. Immunomodulatory Mechanisms of Mesenchymal Stem Cells and Their Potential Clinical Applications. Int J Mol Sci. 2022; 23(17):10023. [59] YUAN D, BAO Y, EL-HASHASH A. Mesenchymal stromal cell-based therapy in lung diseases; from research to clinic. Am J Stem Cells. 2024;13(2):37-58. [60] MORRISON TJ, JACKSON MV, CUNNINGHAM EK, et al. Mesenchymal Stromal Cells Modulate Macrophages in Clinically Relevant Lung Injury Models by Extracellular Vesicle Mitochondrial Transfer. Am J Respir Crit Care Med. 2017;196(10):1275-1286. [61] ZHANG K, GAO Y, DENG Y, et al. Studies on the effects of bone marrow stem cells on mitochondrial function and the alleviation of ARDS. Mol Cell Biochem. 2021;476(1):93-107. [62] CHEN X, LIU Q, HUANG W, et al. Stanniocalcin-2 contributes to mesenchymal stromal cells attenuating murine contact hypersensitivity mainly via reducing CD8+ Tc1 cells. Cell Death Dis. 2018;9(5):548. [63] CALDEIRA-DANTAS S, FURMANAK T, SMITH C, et al. The Chemokine Receptor CXCR3 Promotes CD8+ T Cell Accumulation in Uninfected Salivary Glands but Is Not Necessary after Murine Cytomegalovirus Infection. J Immunol. 2018;200(3):1133-1145. [64] GUO K, YOMBO DJK, WANG Z, et al. The chemokine receptor CXCR3 promotes CD8+ T cell-dependent lung pathology during influenza pathogenesis. Sci Adv. 2024;10(1):eadj1120. [65] ZHU J, FENG B, XU Y, et al. Mesenchymal stem cells alleviate LPS-induced acute lung injury by inhibiting the proinflammatory function of Ly6C+ CD8+ T cells. Cell Death Dis. 2020;11(10):829. [66] TAKAO S, NAKASHIMA T, MASUDA T, et al. Human bone marrow-derived mesenchymal stromal cells cultured in serum-free media demonstrate enhanced antifibrotic abilities via prolonged survival and robust regulatory T cell induction in murine bleomycin-induced pulmonary fibrosis. Stem Cell Res Ther. 2021;12(1):506. [67] EE MT, THÉBAUD B. The Therapeutic Potential of Stem Cells for Bronchopulmonary Dysplasia: “It’s About Time” or “Not so Fast” ? Curr Pediatr Rev. 2018;14(4):227-238. [68] PIERRO M, IONESCU L, MONTEMURRO T, et al. Short-term, long-term and paracrine effect of human umbilical cord-derived stem cells in lung injury prevention and repair in experimental bronchopulmonary dysplasia. Thorax. 2013;68(5):475-484. [69] WANG Y, CAO Z, WEI Q, et al. VH298-loaded extracellular vesicles released from gelatin methacryloyl hydrogel facilitate diabetic wound healing by HIF-1α-mediated enhancement of angiogenesis. Acta Biomater. 2022;147:342-355. [70] HAN MM, HE XY, TANG L, et al. Nanoengineered mesenchymal stem cell therapy for pulmonary fibrosis in young and aged mice. Sci Adv. 2023;9(29):eadg5358. [71] HUANG A, LIU D, QI X, et al. Self-assembled GFFYK peptide hydrogel enhances the therapeutic efficacy of mesenchymal stem cells in a mouse hindlimb ischemia model. Acta Biomater. 2019;85:94-105. [72] YUAN T, LI K, GUO L, et al. Modulation of immunological properties of allogeneic mesenchymal stem cells by collagen scaffolds in cartilage tissue engineering. J Biomed Mater Res A. 2011;98(3):332-341. [73] ALVARADO-VELEZ M, ENAM SF, MEHTA N, et al. Immuno-suppressive hydrogels enhance allogeneic MSC survival after transplantation in the injured brain. Biomaterials. 2021;266:120419. [74] ANSARI S, CHEN C, HASANI-SADRABADI MM, et al. Hydrogel elasticity and microarchitecture regulate dental-derived mesenchymal stem cell-host immune system cross-talk. Acta Biomater. 2017;60:181-189. [75] ZHAO N, COYNE J, ABUNE L, et al. Exogenous Signaling Molecules Released from Aptamer-Functionalized Hydrogels Promote the Survival of Mesenchymal Stem Cell Spheroids. ACS Appl Mater Interfaces. 2020;12(22):24599-24610. [76] ZHANG K, ZHAO X, CHEN X, et al. Enhanced Therapeutic Effects of Mesenchymal Stem Cell-Derived Exosomes with an Injectable Hydrogel for Hindlimb Ischemia Treatment. ACS Appl Mater Interfaces. 2018;10(36):30081-30091. [77] HO SS, MURPHY KC, BINDER BY, et al. Increased Survival and Function of Mesenchymal Stem Cell Spheroids Entrapped in Instructive Alginate Hydrogels. Stem Cells Transl Med. 2016; 5(6):773-781. [78] DURAND N, ZUBAIR AC. Autologous versus allogeneic mesenchymal stem cell therapy: The pros and cons. Surgery. 2022;171(5):1440-1442. [79] GOPALARETHINAM J, NAIR AP, IYER M, et al. Advantages of mesenchymal stem cell over the other stem cells. Acta Histochem. 2023;125(4):152041. [80] DERKS LLM, VAN BOXTEL R. Stem cell mutations, associated cancer risk, and consequences for regenerative medicine. Cell Stem Cell. 2023;30(11):1421-1433. [81] TAN F, LI X, WANG Z, et al. Clinical applications of stem cell-derived exosomes. Signal Transduct Target Ther. 2024;9(1):17. [82] HAN Y, ZHU Y, YOUNGBLOOD HA, et al. Nebulization of extracellular vesicles: A promising small RNA delivery approach for lung diseases. J Control Release. 2022; 352:556-569. [83] GARCIA-APONTE OF, KAHLENBERG S, KOUROUPIS D, et al. Effects of Hydrogels on Mesenchymal Stem/Stromal Cells Paracrine Activity and Extracellular Vesicles Production. J Extracell Vesicles. 2025;14(3):e70057. [84] JU Y, HU Y, YANG P, et al. Extracellular vesicle-loaded hydrogels for tissue repair and regeneration. Mater Today Bio. 2022; 18:100522. [85] HANNA M, ELNASSAG SS, MOHAMED DH, et al. Melatonin and mesenchymal stem cells co-administration alleviates chronic obstructive pulmonary disease via modulation of angiogenesis at the vascular-alveolar unit. Pflugers Arch. 2024; 476(7):1155-1168. |
| [1] | Liu Hongjie, Mu Qiuju, Shen Yuxue, Liang Fei, Zhu Lili. Metal organic framework/carboxymethyl chitosan-oxidized sodium alginate/platelet-rich plasma hydrogel promotes healing of diabetic infected wounds [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1929-1939. |
| [2] |
Dong Chunyang, Zhou Tianen, Mo Mengxue, Lyu Wenquan, Gao Ming, Zhu Ruikai, Gao Zhiwei.
Action mechanism of metformin combined with Eomecon chionantha Hance dressing in treatment of deep second-degree burn wounds#br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2001-2013.
|
| [3] | Wu Yanting, Li Yu, Liao Jinfeng. Magnesium oxide nanoparticles regulate osteogenesis- and angiogenesis-related gene expressions to promote bone defect healing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1885-1895. |
| [4] | Jiang Xinghai, Song Yulin, Li Dejin, Shao Jianmin, Xu Junzhi, Liu Huakai, Wu Yingguo, Shen Yuehui, Feng Sicheng. Vascular endothelial growth factor 165 genes transfected into bone marrow mesenchymal stem cells to construct a vascularized amphiphilic peptide gel module [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1903-1911. |
| [5] | Yang Xuetao, Zhu Menghan, Zhang Chenxi, Sun Yimin, Ye Ling. Applications and limitations of antioxidant nanomaterials in oral cavity [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2044-2053. |
| [6] | Liu Yang, Liu Donghui , Xu Lei, Zhan Xu, Sun Haobo, Kang Kai. Role and trend of stimuli-responsive injectable hydrogels in precise myocardial infarction therapy [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2072-2080. |
| [7] | Wang Zheng, Cheng Ji, Yu Jinlong, Liu Wenhong, Wang Zhaohong, Zhou Luxing. Progress and future perspectives on the application of hydrogel materials in stroke therapy [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2081-2090. |
| [8] | Guo Yuchao, Ni Qianwei, Yin Chen, Jigeer·Saiyilihan, Gao Zhan . Quaternized chitosan hemostatic materials: synthesis, mechanism, and application [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2091-2100. |
| [9] | Hu Xiongke, Liu Shaohua, Tan Qian, Liu Kun, Zhu Guanghui. Shikonin intervention with bone marrow mesenchymal stem cells improves microstructure of femur in aged mice [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1609-1615. |
| [10] | Song Puzhen, Ma Hebin, Chen Hongguang, Zhang Yadong. Effect of bone marrow mesenchymal stem cell-derived exosomes combined with transforming growth factor beta 1 on macrophages [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1616-1623. |
| [11] | Cai Ziming, Yu Qinghe, Ma Pengfei, Zhang Xin, Zhou Longqian, Zhang Chongyang, Lin Wenping. Heme oxygenase-1 alleviates lipopolysaccharide-induced inflammatory response in nucleus pulposus mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1624-1631. |
| [12] | Yuan Xiaoshuang, Yang Xu, Yang Bo, Chen Xiaoxu, Tian Ting, Wang Feiqing, Li Yanju, Liu Yang, Yang Wenxiu. Effect of conditioned medium of diffuse large B-cell lymphoma cells on proliferation and apoptosis of human bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1632-1640. |
| [13] | Li Zhenyu, Zhang Siming, Bai Jiaxiang, Zhu Chen. Osthole improves osteogenic differentiation function of bone marrow mesenchymal stem cells under high-glucose conditions [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1641-1648. |
| [14] | Han Nianrong, Huang Yifei, Akram · Osman, Liu Yanlu, Hu Wei . Programmed cell death receptor-1 suppresses osteogenic differentiation of rat bone marrow mesenchymal stem cells in a high-glucose microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1649-1657. |
| [15] | Jin Dongsheng, Zhao Zhanghong, Zhu Ziyin, Zhang Sen, Sun Zuyan, Deng Jiang. Effects of icariin-loaded microsphere-three-dimensional scaffold on osteogenic differentiation of rabbit bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1658-1668. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||