Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (13): 3217-3225.doi: 10.12307/2026.308
Effect of zoledronic acid on jaw bone marrow mesenchymal stem cells in mice with bisphosphonate-related osteonecrosis of the jaw
Li Pengli1, Yang Yanmei2, Hu Yawen1, Liu Hongqi1, Wang Manyi3, Yan Jianfei3, Gu Bin2
- 1Graduate School of Chinese PLA General Hospital, Beijing 100853, China; 2Department of Stomatology, First Medical Center of Chinese PLA General Hospital, Beijing 100853, China; 3Stomatological Hospital of Fourth Military Medical University, Xi'an 710032, Shaanxi Province, China
-
Received:2025-04-03Revised:2025-05-31Accepted:2025-06-12Online:2026-05-08Published:2025-12-24 -
Contact:Gu Bin, PhD, Chief physician, Professor, Department of Stomatology, First Medical Center of Chinese PLA General Hospital, Beijing 100853, China; Yan Jianfei, PhD, Attending physician, Stomatological Hospital of Fourth Military Medical University, Xi'an 710032, Shaanxi Province, China -
About author:Li Pengli, Master candidate, Graduate School of Chinese PLA General Hospital, Beijing 100853, China -
Supported by:Open Project of National Clinical Research Center for Geriatric Diseases, No. NCRCG-PLAGH-2022017 (to GB); Military Logistics Research Project, No. JKAWS22J1006 (to GB)
CLC Number:
Cite this article
Li Pengli, Yang Yanmei, Hu Yawen, Liu Hongqi, Wang Manyi, Yan Jianfei, Gu Bin. Effect of zoledronic acid on jaw bone marrow mesenchymal stem cells in mice with bisphosphonate-related osteonecrosis of the jaw[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(13): 3217-3225.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
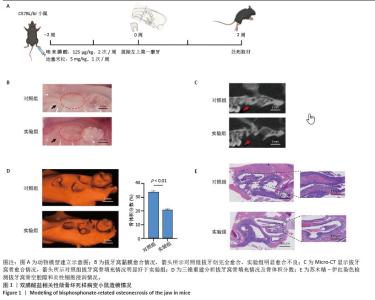
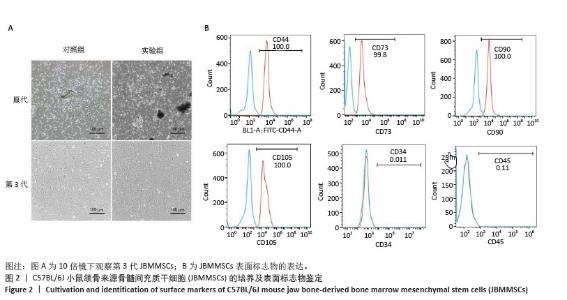
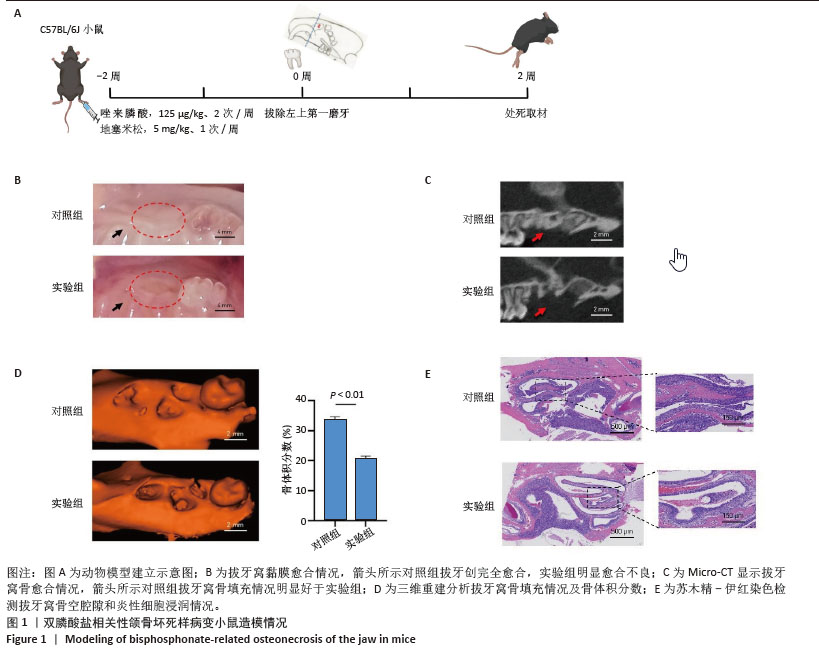
2.1 双膦酸盐相关性颌骨坏死样病变小鼠拔牙窝愈合不良 为了研究双膦酸盐相关性颌骨坏死的潜在发病机制,通过注射唑来膦酸同时拔除小鼠左侧上颌第一磨牙来模拟人双膦酸盐相关性颌骨坏死病变过程,建立双膦酸盐相关性颌骨坏死样病变小鼠模型(图1A)。收集两组小鼠上颌骨,分析拔牙窝愈合情况。对照组(8/8)小鼠拔牙创口完全愈合,而实验组(6/8)小鼠拔牙窝伤口未完全愈合,未愈合率达到75% (图1B)。通过微计算机断层扫描(Micro-CT)与三维重建分析显示,与对照组相比,实验组小鼠拔牙窝区域的骨体积分数和骨矿物质改建均显著降低(图1C,D)。苏木精-伊红染色结果显示实验组小鼠拔牙窝骨空腔隙和炎性细胞浸润更严重(图1E)。 "
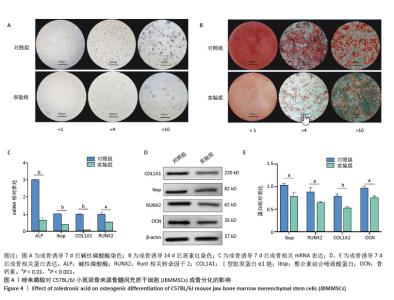
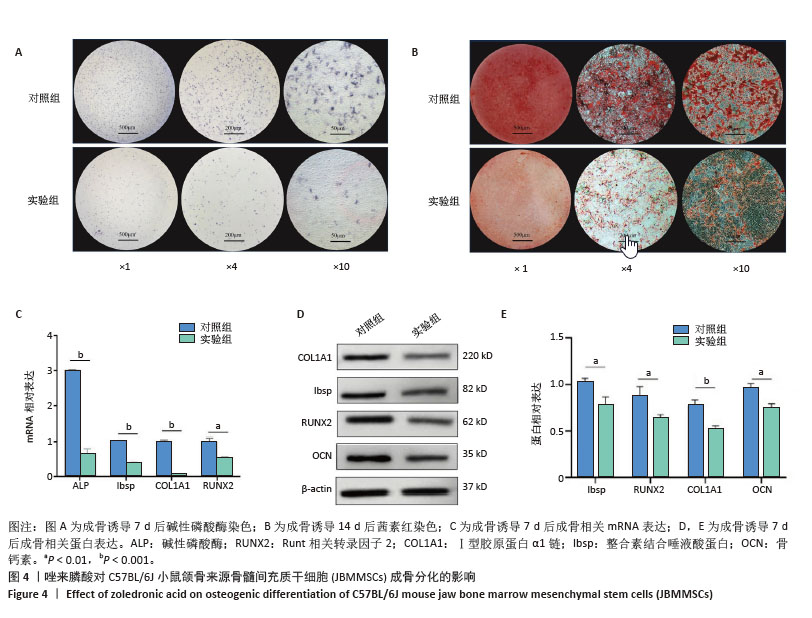
2.4 唑来膦酸对JBMMSCs成骨分化功能的影响 两组JBMMSCs成骨诱导7 d后,碱性磷酸酶染色结果显示,实验组JBMMSCs碱性磷酸酶染色明显弱于对照组(图4A)。成骨诱导14 d后进行茜素红染色,镜下观察到实验组JBMMSCs钙结节数量明显少于对照组(图4B)。成骨诱导7 d后采用qPCR检测成骨标志物碱性磷酸酶、整合素结合唾液酸蛋白、Ⅰ型胶原蛋白α1链、Runt相关转录因子2的mRNA表达水平变化(图4C),以及Western blot检测Ⅰ型胶原蛋白α1链、整合素结合唾液酸蛋白、骨钙素、Runt相关转录因子2蛋白表达水平变化(图4D,E),检测结果均显示实验组成骨相关的基因和蛋白表达降低,差异有显著性意义。上述结果表明唑来膦酸会抑制JBMMSCs的成骨分化功能。 "
| [1] SONG S, GUO Y, YANG Y, et al. Advances in pathogenesis and therapeutic strategies for osteoporosis. Pharmacol Ther. 2022;237:108168. [2] KOBAYASHI T, MORIMOTO T, ITO K, et al. Denosumab vs. bisphosphonates in primary osteoporosis: a meta-analysis of comparative safety in randomized controlled trials. Osteoporos Int. 2024;35(8):1377-1393. [3] HO WC, CHANG CC, WU WT, et al. Effect of Osteoporosis Treatments on Osteoarthritis Progression in Postmenopausal Women: A Review of the Literature. Curr Rheumatol Rep. 2024;26(5):188-195. [4] HAMADEH IS, NGWA BA, GONG Y. Drug induced osteonecrosis of the jaw. Cancer Treat Rev. 2015;41(5): 455-464. [5] FUGGLE N, AL-DAGHRI N, BOCK O, et al. Novel formulations of oral bisphosphonates in the treatment of osteoporosis. Aging Clin Exp Res. 2023;35(6):1375-1376. [6] MARX RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003;61(9):1115-1117. [7] DIOGUARDI M, DI COSOLA M, COPELLI C, et al. Oral bisphosphonate-induced osteonecrosis complications in patients undergoing tooth extraction: a systematic review and literature updates. Eur Rev Med Pharmacol Sci. 2023;27(13):6359-6373. [8] TAJIMA S, MATSUNO H, MATSUMOTO F, et al. A case of bisphosphonate-related osteonecrosis of the maxilla with orbital cellulitis. Ear Nose Throat J. 2025;104(1):22-24. [9] FOTOPOULOS I, ZISIS V, LILLIS T, et al. A Case Report of Ibandronic Acid Induced Non-Exposed BRONJ Involving the Maxillary Sinus. J Oral Maxillofac Res. 2023;14(4):e5. [10] DRUDGE-COATES L, VAN DEN WYNGAERT T, SCHIØDT M, et al. Preventing, identifying, and managing medication-related osteonecrosis of the jaw: a practical guide for nurses and other allied healthcare professionals. Support Care Cancer. 2020;28(9):4019-4029. [11] BAGAN JV, JIMENEZ Y, MURILLO J, et al. Jaw osteonecrosis associated with bisphosphonates: multiple exposed areas and its relationship to teeth extractions. Study of 20 cases. Oral Oncol. 2006;42(3):327-329. [12] SIDDIQI A, PAYNE AG, ZAFAR S. Bisphosphonate-induced osteonecrosis of the jaw: a medical enigma? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(3):e1-8. [13] RUGGIERO SL, DODSON TB, AGHALOO T, et al. American Association of Oral and Maxillofacial Surgeons’ Position Paper on Medication-Related Osteonecrosis of the Jaws-2022 Update. J Oral Maxillofac Surg. 2022;80(5):920-943. [14] CREMERS SC, PILLAI G, PAPAPOULOS SE. Pharmacokinetics/pharmacodynamics of bisphosphonates: use for optimisation of intermittent therapy for osteoporosis. Clin Pharmacokinet. 2005;44(6): 551-570. [15] WANG Q, LIU J, GUO T, et al. Epidermal Growth Factor Reverses the Inhibitory Effects of the Bisphosphonate, Zoledronic Acid, on Human Oral Keratinocytes and Human Vascular Endothelial Cells In Vitro via the Epidermal Growth Factor Receptor (EGFR)/Akt/Phosphoinositide 3-Kinase (PI3K) Signaling Pathway. Med Sci Monit. 2019;25:700-710. [16] FAVOT CL, FORSTER C, GLOGAUER M. The effect of bisphosphonate therapy on neutrophil function: a potential biomarker. Int J Oral Maxillofac Surg. 2013;42(5):619-626. [17] SUNG CM, KIM RJ, HAH YS, et al. In vitro effects of alendronate on fibroblasts of the human rotator cuff tendon. BMC Musculoskelet Disord. 2020;21(1):19. [18] SEDGHIZADEH PP, YOOSEPH S, FADROSH DW, et al. Metagenomic investigation of microbes and viruses in patients with jaw osteonecrosis associated with bisphosphonate therapy. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(6):764-770. [19] TAI TW, CHEN CY, SU FC, et al. Reactive oxygen species are required for zoledronic acid-induced apoptosis in osteoclast precursors and mature osteoclast-like cells. Sci Rep. 2017;7:44245. [20] KOCH FP, MERKEL C, ZIEBART T, et al. Influence of bisphosphonates on the osteoblast RANKL and OPG gene expression in vitro. Clin Oral Investig. 2012;16(1):79-86. [21] UDAGAWA N, KOIDE M, NAKAMURA M, et al. Osteoclast differentiation by RANKL and OPG signaling pathways. J Bone Miner Metab. 2021; 39(1):19-26. [22] QU X, SUN Z, WANG Y, et al. Zoledronic acid promotes osteoclasts ferroptosis by inhibiting FBXO9-mediated p53 ubiquitination and degradation. PeerJ. 2021;9:e12510. [23] PATNTIRAPONG S, SINGHATANADGIT W, CHANRUANGVANIT C, et al. Zoledronic acid suppresses mineralization through direct cytotoxicity and osteoblast differentiation inhibition. J Oral Pathol Med. 2012;41(9):713-720. [24] MANZANO-MORENO FJ, RAMOS-TORRECILLAS J, DE LUNA-BERTOS E, et al. High doses of bisphosphonates reduce osteoblast-like cell proliferation by arresting the cell cycle and inducing apoptosis. J Craniomaxillofac Surg. 2015;43(3):396-401. [25] HUANG X, HUANG S, GUO F, et al. Dose-dependent inhibitory effects of zoledronic acid on osteoblast viability and function in vitro. Mol Med Rep. 2016;13(1):613-622. [26] YANG X, LU Y, LI Z, et al. Low concentrations of zoledronic acid are better at regulating bone formation and repair. Intractable Rare Dis Res. 2013;2(1):18-23. [27] HUANG KC, CHENG CC, CHUANG PY, et al. The effects of zoledronate on the survival and function of human osteoblast-like cells. BMC Musculoskelet Disord. 2015;16:355. [28] BASSAN MARINHO MACIEL G, MARINHO MACIEL R, LINHARES FERRAZZO K, et al. Etiopathogenesis of medication-related osteonecrosis of the jaws: a review. J Mol Med (Berl). 2024;102(3): 353-364. [29] FREIBERGER JJ, PADILLA-BURGOS R, MCGRAW T, et al. What is the role of hyperbaric oxygen in the management of bisphosphonate-related osteonecrosis of the jaw: a randomized controlled trial of hyperbaric oxygen as an adjunct to surgery and antibiotics. J Oral Maxillofac Surg. 2012;70(7):1573-1583. [30] RUFATO CED, PRADO MC, LUFT RL, et al. Use of platelet concentrates in oral surgery of patients with osteonecrosis: a scoping review. Braz Dent J. 2023;34(2):1-13. [31] RIPAMONTI CI, CISLAGHI E, MARIANI L, et al. Efficacy and safety of medical ozone (O(3)) delivered in oil suspension applications for the treatment of osteonecrosis of the jaw in patients with bone metastases treated with bisphosphonates: Preliminary results of a phase I-II study. Oral Oncol. 2011;47(3):185-190. [32] SIM IW, BORROMEO GL, TSAO C, et al. Teriparatide Promotes Bone Healing in Medication-Related Osteonecrosis of the Jaw: A Placebo-Controlled, Randomized Trial. J Clin Oncol. 2020;38(26):2971-2980. [33] OWOSHO AA, ESTILO CL, HURYN JM, et al. Pentoxifylline and tocopherol in the management of cancer patients with medication-related osteonecrosis of the jaw: an observational retrospective study of initial case series. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122(4):455-459. [34] OKAWA H, KONDO T, HOKUGO A, et al. Mechanism of bisphosphonate-related osteonecrosis of the jaw (BRONJ) revealed by targeted removal of legacy bisphosphonate from jawbone using competing inert hydroxymethylene diphosphonate. Elife. 2022;11:e76207. [35] SHEN X, ZHU W, ZHANG P, et al. Macrophage miR-149-5p induction is a key driver and therapeutic target for BRONJ. JCI Insight. 2022; 7(16):e159865. [36] MOVILA A, MAWARDI H, NISHIMURA K, et al. Possible pathogenic engagement of soluble Semaphorin 4D produced by γδT cells in medication-related osteonecrosis of the jaw (MRONJ). Biochem Biophys Res Commun. 2016;480(1):42-47. [37] SONG M, ALSHAIKH A, KIM T, et al. Preexisting Periapical Inflammatory Condition Exacerbates Tooth Extraction-induced Bisphosphonate-related Osteonecrosis of the Jaw Lesions in Mice. J Endod. 2016; 42(11):1641-1646. [38] ADACHI N, AYUKAWA Y, YASUNAMI N, et al. Preventive effect of fluvastatin on the development of medication-related osteonecrosis of the jaw. Sci Rep. 2020;10(1):5620. [39] VESZELYNÉ KOTÁN E, BARTHA-LIEB T, PARISEK Z, et al. Database analysis of the risk factors of bisphosphonate-related osteonecrosis of the jaw in Hungarian patients. BMJ Open. 2019;9(5):e025600. [40] 王一名,张武阳,李晨,等.小鼠双膦酸盐相关性颌骨坏死建模的研究进展[J].中国实用口腔科杂志,2021,14(3):351-355. [41] WANG G, PENG T, CHEN L, et al. Mevalonate pathway inhibition reduces bladder cancer metastasis by modulating RhoB protein stability and integrin β1 localization. Commun Biol. 2024;7(1):1476. |
| [1] | Sun Lei, Zhang Qi, Zhang Yu. Pro-osteoblastic effect of chlorogenic acid protein microsphere/polycaprolactone electrospinning membrane [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1877-1884. |
| [2] | Wu Yanting, Li Yu, Liao Jinfeng. Magnesium oxide nanoparticles regulate osteogenesis- and angiogenesis-related gene expressions to promote bone defect healing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1885-1895. |
| [3] | Jiang Xinghai, Song Yulin, Li Dejin, Shao Jianmin, Xu Junzhi, Liu Huakai, Wu Yingguo, Shen Yuehui, Feng Sicheng. Vascular endothelial growth factor 165 genes transfected into bone marrow mesenchymal stem cells to construct a vascularized amphiphilic peptide gel module [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1903-1911. |
| [4] | Wang Qisa, Lu Yuzheng, Han Xiufeng, Zhao Wenling, Shi Haitao, Xu Zhe. Cytocompatibility of 3D printed methyl acrylated hyaluronic acid/decellularized skin hydrogel scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1912-1920. |
| [5] | Wang Zhenze, Liu Fende, Zhang Rui, Li Wujun. Mesenchymal stem cells in treatment of arteriosclerosis obliterans of lower extremities: systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1869-1876. |
| [6] | Hu Xiongke, Liu Shaohua, Tan Qian, Liu Kun, Zhu Guanghui. Shikonin intervention with bone marrow mesenchymal stem cells improves microstructure of femur in aged mice [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1609-1615. |
| [7] | Cai Ziming, Yu Qinghe, Ma Pengfei, Zhang Xin, Zhou Longqian, Zhang Chongyang, Lin Wenping. Heme oxygenase-1 alleviates lipopolysaccharide-induced inflammatory response in nucleus pulposus mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1624-1631. |
| [8] | Yuan Xiaoshuang, Yang Xu, Yang Bo, Chen Xiaoxu, Tian Ting, Wang Feiqing, Li Yanju, Liu Yang, Yang Wenxiu. Effect of conditioned medium of diffuse large B-cell lymphoma cells on proliferation and apoptosis of human bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1632-1640. |
| [9] | Li Zhenyu, Zhang Siming, Bai Jiaxiang, Zhu Chen. Osthole improves osteogenic differentiation function of bone marrow mesenchymal stem cells under high-glucose conditions [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1641-1648. |
| [10] | Han Nianrong, Huang Yifei, Akram · Osman, Liu Yanlu, Hu Wei . Programmed cell death receptor-1 suppresses osteogenic differentiation of rat bone marrow mesenchymal stem cells in a high-glucose microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1649-1657. |
| [11] | Jin Dongsheng, Zhao Zhanghong, Zhu Ziyin, Zhang Sen, Sun Zuyan, Deng Jiang. Effects of icariin-loaded microsphere-three-dimensional scaffold on osteogenic differentiation of rabbit bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1658-1668. |
| [12] | Zou Yulian, Chen Chaopei, Huang Haixia, Lan Yuyan, Liu Min, Huang Ting. Resveratrol promotes osteogenic differentiation of bone marrow mesenchymal stem cells in an inflammatory microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1669-1678. |
| [13] | Wang Qiuhua, Du Ziwei, Wang Wenshuang, Zhao Dongmei, Zhang Xiaoqing. Differences in metabolism, proliferation, differentiation of adipose-derived mesenchymal stem cells, and differentiation into vascular smooth muscle cells between male and female rats [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1687-1698. |
| [14] | He Jiale, Huang Xi, Dong Hongfei, Chen Lang, Zhong Fangyu, Li Xianhui. Acellular dermal matrix combined with adipose-derived stem cell exosomes promotes burn wound healing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1699-1710. |
| [15] | Xia Linfeng, Wang Lu, Long Qianfa, Tang Rongwu, Luo Haodong, Tang Yi, Zhong Jun, Liu Yang. Human umbilical cord mesenchymal stem cell-derived exosomes alleviate blood-brain barrier damage in mice with septic encephalopathy [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1711-1719. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||