Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (7): 1711-1719.doi: 10.12307/2026.047
Previous Articles Next Articles
Human umbilical cord mesenchymal stem cell-derived exosomes alleviate blood-brain barrier damage in mice with septic encephalopathy
Xia Linfeng1, 2, Wang Lu3, Long Qianfa4, Tang Rongwu2, Luo Haodong5, Tang Yi1, Zhong Jun2, Liu Yang1, 2
- 1School of Clinical Medicine, North Sichuan Medical College, Nanchong 637000, Sichuan Province, China; 2Department of Neurosurgery, 3Department of Radiology, The Third People’s Hospital of Mianyang (Sichuan Mental Health Center), Mianyang 621000, Sichuan Province, China; 4Department of Neurosurgery, Xi’an Central Hospital, Xi’an 710003, Shaanxi Province, China; 5School of Clinical Medicine, Southwest Medical University, Luzhou 646000, Sichuan Province, China
-
Received:2024-12-19Revised:2025-04-22Accepted:2025-05-29Online:2026-03-08Published:2025-08-19 -
Contact:Liu Yang, MD, Chief physician, School of Clinical Medicine, North Sichuan Medical College, Nanchong 637000, Sichuan Province, China; Department of Neurosurgery, The Third People’s Hospital of Mianyang (Sichuan Mental Health Center), Mianyang 621000, Sichuan Province, China -
About author:Xia Linfeng, Master candidate, Physician, School of Clinical Medicine, North Sichuan Medical College, Nanchong 637000, Sichuan Province, China; Department of Neurosurgery, The Third People’s Hospital of Mianyang (Sichuan Mental Health Center), Mianyang 621000, Sichuan Province, China -
Supported by:Mianyang Municipal Health Commission Support Project, No. 202201 (to LY); Sichuan Medical Association Support Project, No. Q22020 (to ZJ)
CLC Number:
Cite this article
Xia Linfeng, Wang Lu, Long Qianfa, Tang Rongwu, Luo Haodong, Tang Yi, Zhong Jun, Liu Yang. Human umbilical cord mesenchymal stem cell-derived exosomes alleviate blood-brain barrier damage in mice with septic encephalopathy[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1711-1719.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

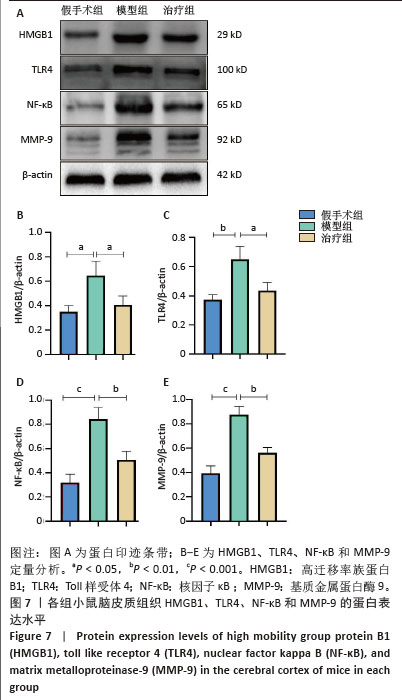
2.2 实验动物数量分析 参加实验小鼠数量为52只,进入结果分析小鼠数量为52只,中途无小鼠死亡、脱落。 2.3 各组小鼠脑皮质组织内炎症因子的表达以及外泌体对脓毒症小鼠的抑炎作用 与假手术组相比,模型组肿瘤坏死因子α和白细胞介素1β的表达水平均显著升高;与模型组相比,治疗组肿瘤坏死因子α和白细胞介素1β的表达水平均显著降低(P < 0.05,图2),说明腹腔注射脂多糖可以引起小鼠脑皮质炎症的发生,且外泌体可以减轻炎症反应。 2.4 各组小鼠血脑屏障通透性的改变 与假手术组相比,模型组脑含水量明显增加,而外泌体可明显降低脑组织含水量,说明外泌体抑制了脂多糖所引起的脑水肿,治疗组较模型组血脑屏障功能更加完整,见图3A。与假手术组相比,模型组脑皮质组织中伊文思蓝含量明显增加;与模型组相比,治疗组脑皮质组织中伊文思蓝含量明显减少,见图3B,说明外泌体可以降低模型组小鼠血脑屏障通透性,维持血脑屏障的完整性。 "
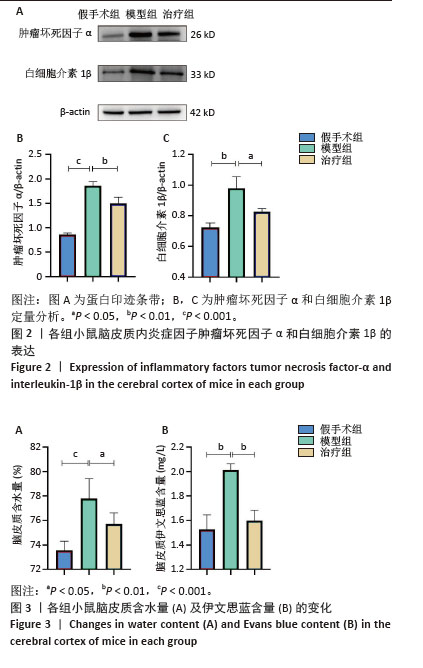

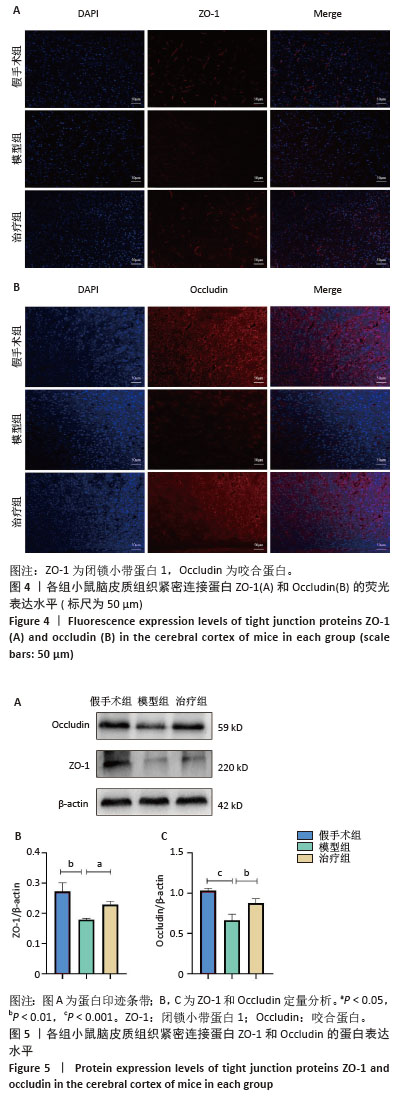
2.5 各组小鼠脑皮质组织紧密连接蛋白ZO-1和Occludin的荧光表达水平 免疫荧光结果显示,假手术组脑皮质组织可见高荧光强度ZO-1及Occludin阳性细胞,模型组脑皮质组织荧光强度降低,阳性染色细胞比例下降;与模型组相比,治疗组的荧光强度升高,阳性染色细胞比例增加,见图4。由此可见脂多糖会破坏小鼠血脑屏障的紧密连接屏障完整性,而外泌体上调了血脑屏障紧密连接蛋白数量,减轻了脂多糖对血脑屏障紧密连接屏障的破坏。 2.6 各组小鼠脑皮质组织紧密连接蛋白ZO-1和Occludin蛋白表达水平 Western blot结果显示,与假手术组比较,模型组小鼠脑皮质组织中ZO-1和Occludin蛋白表达显著降低,外泌体干预后ZO-1和Occludin蛋白表达显著升高,见图5。以上结果说明,脂多糖破坏了小鼠血脑屏障的功能和稳定性,而外泌体则可以保护小鼠血脑屏障的稳定性。 "
| [1] FLEISCHMANN C, SCHERAG A, ADHIKARI NK, et al. Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations. Am J Respir Crit Care Med. 2016;193(3): 259-272. [2] HUANG Y, CHEN R, JIANG L, et al. Basic research and clinical progress of sepsis-associated encephalopathy. J Intensive Med. 2021;1(2):90-95. [3] IWASHYNA TJ, ELY EW, SMITH DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787-1794. [4] 唐梅,马艳,张西京,等.脓毒症脑病的诊疗进展[J].空军军医大学学报,2023,44(4):375-379+384. [5] GAO Q, HERNANDES MS. Sepsis-Associated Encephalopathy and Blood-Brain Barrier Dysfunction. Inflammation. 2021;44(6):2143-2150. [6] 王雪,刘阳,徐剑峰,等.脐带间充质干细胞来源外泌体对脑出血模型小鼠海马神经元的保护作用[J].中国组织工程研究,2022, 26(31):4928-4934. [7] YIN S, JI C, WU P, et al. Human umbilical cord mesenchymal stem cells and exosomes: bioactive ways of tissue injury repair. Am J Transl Res. 2019;11(3):1230-1240. [8] PATEL G, AGNIHOTRI TG, GITTE M, et al. Exosomes: a potential diagnostic and treatment modality in the quest for counteracting cancer. Cell Oncol (Dordr). 2023;46(5):1159-1179. [9] ROSZKOWSKI S. Therapeutic potential of mesenchymal stem cell-derived exosomes for regenerative medicine applications. Clin Exp Med. 2024;24(1):46. [10] LIU SF, LI LY, ZHUANG JL, et al. Update on the application of mesenchymal stem cell-derived exosomes in the treatment of Parkinson’s disease: A systematic review. Front Neurol. 2022;13: 950715. [11] LI J, HUANG Y, SUN H, et al. Mechanism of mesenchymal stem cells and exosomes in the treatment of age-related diseases. Front Immunol. 2023;14:1181308. [12] TAN F, LI X, WANG Z, et al. Clinical applications of stem cell-derived exosomes. Signal Transduct Target Ther. 2024;9(1):17. [13] BANKS WA, SHARMA P, BULLOCK KM, et al. Transport of Extracellular Vesicles across the Blood-Brain Barrier: Brain Pharmacokinetics and Effects of Inflammation. Int J Mol Sci. 2020;21(12):4407. [14] YAGHOUBI Y, MOVASSAGHPOUR A, ZAMANI M, et al. Human umbilical cord mesenchymal stem cells derived-exosomes in diseases treatment. Life Sci. 2019;233:116733. [15] 李潇,颜海鹏,肖政辉.脓毒症动物模型的制备方法及影响因素[J].实验动物与比较医学,2022,42(3):207-212. [16] MA Y, SHE X, LIU Y, et al. MSC-derived exosomal miR-140-3p improves cognitive dysfunction in sepsis-associated encephalopathy by HMGB1 and S-lactoylglutathione metabolism. Commun Biol. 2024;7(1):562. [17] YIN XY, TANG XH, WANG SX, et al. HMGB1 mediates synaptic loss and cognitive impairment in an animal model of sepsis-associated encephalopathy. J Neuroinflammation. 2023;20(1):69. [18] YANG YL, CHENG X, LI WH, et al. Kaempferol Attenuates LPS-Induced Striatum Injury in Mice Involving Anti-Neuroinflammation, Maintaining BBB Integrity, and Down-Regulating the HMGB1/TLR4 Pathway. Int J Mol Sci. 2019;20(3):491. [19] WANG TH, XIONG LL, YANG SF, et al. LPS Pretreatment Provides Neuroprotective Roles in Rats with Subarachnoid Hemorrhage by Downregulating MMP9 and Caspase3 Associated with TLR4 Signaling Activation. Mol Neurobiol. 2017;54(10):7746-7760. [20] GU Z, YIN Z, SONG P, et al. Safety and biodistribution of exosomes derived from human induced pluripotent stem cells. Front Bioeng Biotechnol. 2022;10:949724. [21] ZHAO R, WANG L, WANG T, et al. Inhalation of MSC-EVs is a noninvasive strategy for ameliorating acute lung injury. J Control Release. 2022; 345:214-230. [22] CUI F, CHEN Y, WU X, et al. Mesenchymal stem cell-derived exosomes carrying miR-486-5p inhibit glycolysis and cell stemness in colorectal cancer by targeting NEK2. BMC Cancer. 2024;24(1):1356. [23] ZHANG C, LIAO W, LI W, et al. Human umbilical cord mesenchymal stem cells derived extracellular vesicles alleviate salpingitis by promoting M1-to-M2 transformation. Front Physiol. 2023;14:1131701. [24] ZHONG X, CHEN Z, WANG Y, et al. JQ1 attenuates neuroinflammation by inhibiting the inflammasome-dependent canonical pyroptosis pathway in SAE. Brain Res Bull. 2022;189:174-183. [25] LUO Q, XIAN P, WANG T, et al. Antioxidant activity of mesenchymal stem cell-derived extracellular vesicles restores hippocampal neurons following seizure damage. Theranostics. 2021;11(12):5986-6005. [26] ZHOU Y, BAI L, TANG W, et al. Research progress in the pathogenesis of sepsis-associated encephalopathy. Heliyon. 2024;10(12):e33458. [27] LU X, QIN M, WALLINE JH, et al. Clinical phenotypes of sepsis-associated encephalopathy: a retrospective cohort study. Shock. 2023;59(4): 583-590. [28] GE X, MENG Q, LIU X, et al. Extracellular vesicles from normal tissues orchestrate the homeostasis of macrophages and attenuate inflammatory injury of sepsis. Bioeng Transl Med. 2023;9(1):e10609. [29] LIU X, MENG P, LIU Z, et al. New insights on targeting extracellular vesicle release by GW4869 to modulate lipopolysaccharide-induced neuroinflammation in mice model. Nanomedicine (Lond). 2024;19(30):2619-2632. [30] JU Y, HU Y, YANG P, et al. Extracellular vesicle-loaded hydrogels for tissue repair and regeneration. Mater Today Bio. 2022;18:100522. [31] SAVI FF, DE OLIVEIRA A, DE MEDEIROS GF, et al. What animal models can tell us about long-term cognitive dysfunction following sepsis: A systematic review. Neurosci Biobehav Rev. 2021;124:386-404. [32] KUO WT, ODENWALD MA, TURNER JR, et al. Tight junction proteins occludin and ZO-1 as regulators of epithelial proliferation and survival. Ann N Y Acad Sci. 2022;1514(1):21-33. [33] DITHMER S, BLASIG IE, FRASER PA, et al. The Basic Requirement of Tight Junction Proteins in Blood-Brain Barrier Function and Their Role in Pathologies. Int J Mol Sci. 2024;25(11):5601. [34] SUNNY A, JAMES RR, MENON SR, et al. Matrix Metalloproteinase-9 inhibitors as therapeutic drugs for traumatic brain injury. Neurochem Int. 2024;172:105642. [35] ZAGREAN AM, HERMANN DM, OPRIS I, et al. Multicellular Crosstalk Between Exosomes and the Neurovascular Unit After Cerebral Ischemia. Therapeutic Implications. Front Neurosci. 2018;12:811. [36] WANG Y, LIU J, WANG H, et al. Mesenchymal Stem Cell-Derived Exosomes Ameliorate Diabetic Kidney Disease Through the NLRP3 Signaling Pathway. Stem Cells. 2023;41(4):368-383. [37] ZHANG N, LUO Y, ZHANG H, et al. Exosomes Derived from Mesenchymal Stem Cells Ameliorate the Progression of Atherosclerosis in ApoE-/- Mice via FENDRR. Cardiovasc Toxicol. 2022;22(6):528-544. [38] FANG S, LIU Z, WU S, et al. Pro-angiognetic and pro-osteogenic effects of human umbilical cord mesenchymal stem cell-derived exosomal miR-21-5p in osteonecrosis of the femoral head. Cell Death Discov. 2022;8(1):226. [39] KARIMI A, POURREZA S, VAJDI M, et al. Evaluating the effects of curcumin nanomicelles on clinical outcome and cellular immune responses in critically ill sepsis patients: A randomized, double-blind, and placebo-controlled trial. Front Nutr. 2022;9:1037861. [40] YANG Y, GAO L, XI J, et al. Mesenchymal stem cell-derived extracellular vesicles mitigate neuronal damage from intracerebral hemorrhage by modulating ferroptosis. Stem Cell Res Ther. 2024;15(1):255. [41] ABBASI R, ALAMDARI-MAHD G, MALEKI-KAKELAR H, et al. Recent advances in the application of engineered exosomes from mesenchymal stem cells for regenerative medicine. Eur J Pharmacol. 2025;989:177236. |
| [1] | Song Puzhen, Ma Hebin, Chen Hongguang, Zhang Yadong. Effect of bone marrow mesenchymal stem cell-derived exosomes combined with transforming growth factor beta 1 on macrophages [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1616-1623. |
| [2] | Cai Ziming, Yu Qinghe, Ma Pengfei, Zhang Xin, Zhou Longqian, Zhang Chongyang, Lin Wenping. Heme oxygenase-1 alleviates lipopolysaccharide-induced inflammatory response in nucleus pulposus mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1624-1631. |
| [3] | Zou Yulian, Chen Chaopei, Huang Haixia, Lan Yuyan, Liu Min, Huang Ting. Resveratrol promotes osteogenic differentiation of bone marrow mesenchymal stem cells in an inflammatory microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1669-1678. |
| [4] | He Jiale, Huang Xi, Dong Hongfei, Chen Lang, Zhong Fangyu, Li Xianhui. Acellular dermal matrix combined with adipose-derived stem cell exosomes promotes burn wound healing [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1699-1710. |
| [5] | Chen Yulin, He Yingying, Hu Kai, Chen Zhifan, Nie Sha Meng Yanhui, Li Runzhen, Zhang Xiaoduo , Li Yuxi, Tang Yaoping. Effect and mechanism of exosome-like vesicles derived from Trichosanthes kirilowii Maxim. in preventing and treating atherosclerosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1768-1781. |
| [6] | Han Teng, Ma Hong, Yang Ruoyi, Luo Yi, Li Chao. Oral squamous cell carcinoma-derived exosomal delivery of angiopoietin-2 is involved in tumor angiogenesis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1755-1767. |
| [7] | Huang Jiawen, Pan Zhiyi, Xue Wenjun, Lian Yuanpei, Xu Jianda. Plant-derived vesicles and malignant tumor therapy: cross-species communication and modulation of host cell responses [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1828-1838. |
| [8] | Wang Baiyan, Yang Shu, Wang Yiming, Wu Mengqing, Xiao Yu, Guo Zixuan, Zhang Boyi, Feng Shuying. Exosome-delivered CRISPR/Cas system enables gene editing in target cells [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1839-1849. |
| [9] | Wang Zhenze, Liu Fende, Zhang Rui, Li Wujun. Mesenchymal stem cells in treatment of arteriosclerosis obliterans of lower extremities: systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1869-1876. |
| [10] | Zuo Na, Tang Qi, Yu Meng, Tao Kai. Effect of miR-196b-5p in adipose-derived stem cell exosomes on burn wound healing in rats [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 43-49. |
| [11] | Yuan Weiyuan, Lei Qinhui, Li Xiuqi, Lu Tiezhu, Fu Ziwen, Liang Zhili, Ji Shaoyang, Li Yijia, Ren Yu . Therapeutic effects of adipose-derived mesenchymal stem cells and their exosomes on dexamethasone-induced sarcopenia in mice [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 58-67. |
| [12] | Wu Zhijing, Li Jiali, Zhang Jiaxin, Wang Tangrong, Zheng Yuzhou, Sun Zixuan. Alpha-ketoglutarate engineered small extracellular vesicles delay skin aging [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 120-129. |
| [13] | Zhang Zhaowei, Chen Ouzile, Bai Mingru, Wang Chenglin. Therapeutic potential of bioactive substances secreted by dental mesenchymal stem cells for bone repair [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 163-174. |
| [14] | Liu Nian, Dong Xinyue, Wang Songpeng, Xu Yingjiang, Zhang Xiaoming. Stem cell exosomes and biomaterial-assisted exosomes in bone defect repair [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 175-183. |
| [15] | Lyu Ruyue, Gu Lulu, Liu Qian, Zhou Siyi, Li Beibei, Xue Letian, Sun Peng. Regulatory mechanisms of exosome secretion and its application prospects in biomedicine [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 184-193. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||