Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (9): 1796-1802.doi: 10.12307/2025.136
Previous Articles Next Articles
Cervical lordosis ratio can be used as a decision-making indicator for selection of posterior surgical approach for multi-level cervical spondylotic myelopathy
Miao Jiahang, Ma Sheng, Li Qupeng, Yu Huilin, Hu Tianyu, Gao Xiao, Feng Hu
- Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China
-
Received:2023-12-05Accepted:2024-01-29Online:2025-03-28Published:2024-10-09 -
Contact:Feng Hu, Master’s supervisor, Chief physician, Professor, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China -
About author:Miao Jiahang, Master candidate, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China
CLC Number:
Cite this article
Miao Jiahang, Ma Sheng, Li Qupeng, Yu Huilin, Hu Tianyu, Gao Xiao, Feng Hu. Cervical lordosis ratio can be used as a decision-making indicator for selection of posterior surgical approach for multi-level cervical spondylotic myelopathy[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1796-1802.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
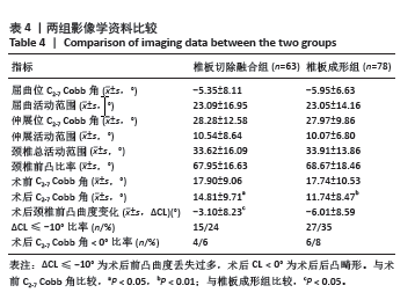
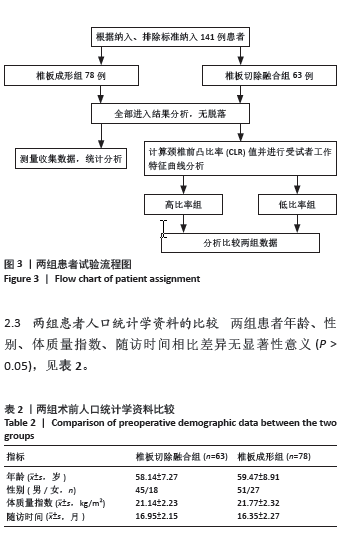
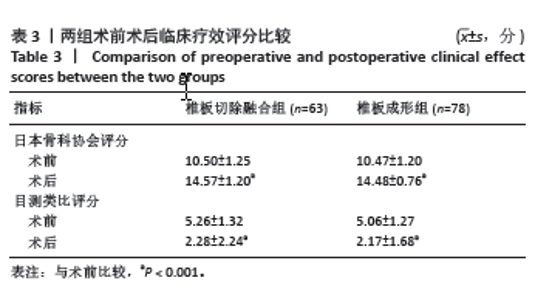
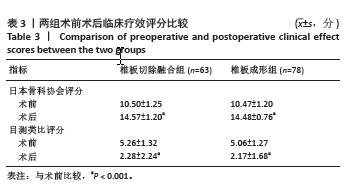
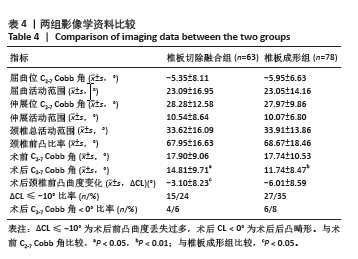
2.5 两组患者影像学指标的比较 在影像学方面,两术式组患者术前动力位的各项指标(屈曲位C2-7 Cobb角、伸展位C2-7 Cobb角、屈曲活动范围、伸展活动范围、颈椎总活动范围、颈椎前凸比率)比较,差异无显著性意义(P > 0.05)。其中,椎板切除融合组\椎板成形组术前与术后的C2-7 Cobb角进行比较,发现差异均有显著性意义(P=0.039,P=0.002)。对两组的术前术后前凸曲度差值(ΔCL)进行比较,发现差异有显著性意义(P=0.043)。在术后前凸曲度丢失过多(ΔCL≤-10°)和术后后凸畸形(CL < 0°)的发生率方面,椎板切除融合组为24%和6%,椎板成形组为35%和8%。见表4。"
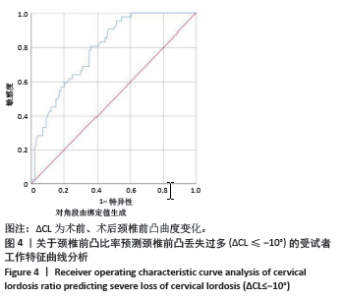
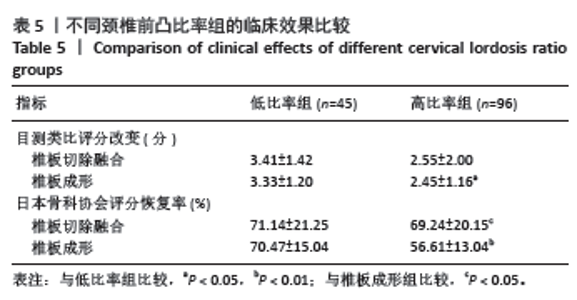
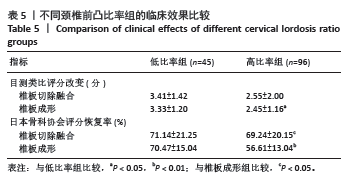
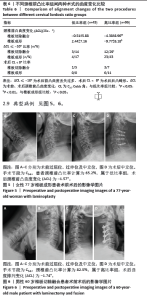
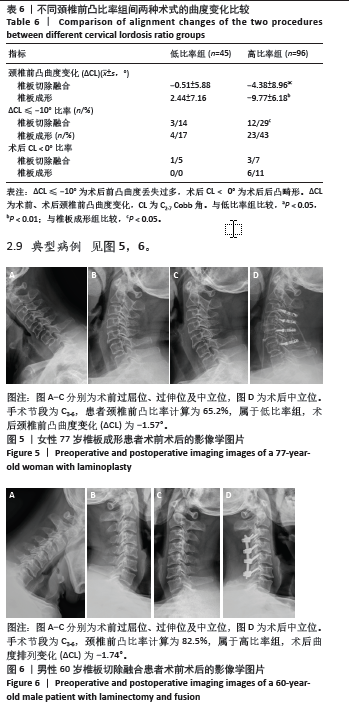
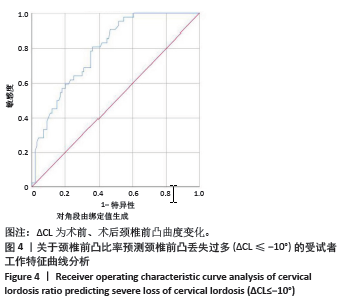
2.6 CLR对术后颈椎前凸曲度丢失过多(ΔCL≤-10°)预测的ROC曲线分析 通过ROC曲线分析(图4),曲线下面积为0.792,状态变量为ΔCL≤-10°,临界值为68.5%,敏感性为81%,特异性为63.6%。根据CLR临界值将患者分为高比率组(≥68.5%)和低比率组(< 68.5%)。 2.7 不同CLR比率组下两种术式的临床效果评分的比较 通过对不同比率组患者的临床结果进行比较,在低比率组中,椎板切除融合术和椎板成形术在目测类比评分改变、JOA评分恢复率方面差异无显著性意义(P > 0.05),在高比率组中,椎板切除融合术和椎板成形术在目测类比评分改变方面差异无显著性意义(P=0.849),但在JOA评分恢复率方面,差异有显著性意义(P=0.001)。见表5。 2.8 不同CLR比率组下两术式组颈椎前凸曲度相关指标的比较 在不同比率组下进一步对两个术式的术后颈椎前凸曲度变化进行比较,在低比率组中,两术式组间术后颈椎前凸曲度变化(ΔCL)差异无显著性意义(P=0.141),在术后前凸曲度丢失过多(ΔCL≤-10°)方面,椎板切除融合组和椎板成形组分别为14%和17%,差别较小;在后凸畸形方面,椎板切除融合组和椎板成形组分别为5%和0%。在高比率组中,两术式组之间术后颈椎前凸曲度变化差异有显著性意义(P=0.001),在术后前凸曲度丢失过多(ΔCL≤-10°)方面,椎板切除融合组和椎板成形组分别为29%和43%,差别较大;在术后后凸畸形方面,椎板切除融合组和椎板成形组分别为7%和11%。此外,无论是椎板切除融合术还是椎板成形术,高比率组的颈椎前凸曲度变化(ΔCL)始终是要大于低比率组(P=0.045,P < 0.001)。见表6。 2.9 典型病例 见图5,6。 2.10 不良事件 此次研究纳入141例患者在并发症方面,共有2例患者发生C5神经根麻痹,其中椎板成形组1例(1.3%),椎板切除融合组1例(1.6%),全部在术后3-6个月显著好转;共3例患者出现术后切口感染,其中椎板成形组2例,椎板切除融合组1例,术后使用敏感抗生素两三周后感染消退(症状好转,辅助检查指标恢复正常);所有患者均未出现其他手术相关并发症,如脑脊液漏、血肿、食管气管瘘、声音嘶哑、脊髓神经损伤、肌力进行性下降等不良事件;均未出现患者伤残、危及生命或死亡等严重不良事件。"
| [1] LAW MD, BERNHARDT M, WHITE AA. Cervical spondylotic myelopathy: a review of surgical indications and decision making. Yale J Biol Med. 1993; 66(3):165-177. [2] LIU F, YANG SD, HUO LS, et al. Laminoplasty versus laminectomy and fusion for multilevel cervical compressive myelopathy: a meta-analysis. Medicine (Baltim). 2016;95(23):e3588. [3] ADOGWA O, HUANG K, HAZZARD M, et al. Outcomes after cervical laminectomy with instrumented fusion versus expansile laminoplasty: a propensity matched study of 3185 patients. J Clin Neurosci. 2015;22(3):549-553. [4] KUMAR VG, REA GL, MERVIS LJ, et al. Cervical spondylotic myelopathy: functional and radiographic long-term outcome after laminectomy and posterior fusion. Neurosurgery. 1999;44(4):771-778. [5] SODEYAMA T, GOTO S, MOCHIZUKI M, et al. Effect of decompression enlargement laminoplasty for posterior shifting of the spinal cord. Spine (Phila Pa 1976). 1999;24(15):1527-1532. [6] KONG C, LI XY, SUN XY, et al. The ratio of C2-C7 Cobb angle to T1 slope is an effective parameter for the selection of posterior surgical approach for patients with multisegmental cervical spondylotic myelopathy. J Orthop Sci. 2020;25(6):953-959. [7] FUJISHIRO T, HAYAMA S, OBO T, et al. Gap between flexion and extension ranges of motion: a novel indicator to predict the loss of cervical lordosis after laminoplasty in patients with cervical spondylotic myelopathy. J Neurosurg Spine. 2021;35(1):8-17. [8] ONO K, MURATA S, MATSUSHITA M, et al. Cervical Lordosis Ratio as a Novel Predictor for the Loss of Cervical Lordosis After Laminoplasty. Neurospine. 2021;18(2):311-318. [9] WHITE AA 3RD, JOHNSON RM, PANJABI MM, et al. Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop Relat Res. 1975;(109): 85-96. [10] 李程,郭开今,李强,等. Arch钛板与侧块螺钉固定治疗颈椎后纵韧带骨化症疗效比较[J]. 实用骨科杂志,2017,23(10):873-878. [11] XU R, HAMAN SP, EBRAHEIM NA, et al. The anatomic relation of lateral mass screws to the spinal nerves. A comparison of the Magerl, Anderson, and An techniques. Spine (Phila Pa 1976). 1999;24(19):2057-2061. [12] 伍少玲,马超,伍时玲,等. 颈椎功能障碍指数量表的效度与信度研究[J]. 中国康复医学杂志,2008,23(7):625-628. [13] 王宇,李翔宇,刘承鑫,等. 多节段颈椎前路术后颈椎前凸角丢失的危险因素分析[J]. 首都医科大学学报,2022,43(1):149-155. [14] HIRABAYASHI K, MIYAKAWA J, SATOMI K, et al. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976). 1981; 6(4):354-364. [15] BABA H, UCHIDA K, MAEZAWA Y, et al. Lordotic alignment and posterior migration of the spinal cord following en bloc open-door laminoplasty for cervical myelopathy: a magnetic resonance imaging study. J Neurol. 1996; 243(9):626-632. [16] LEE CH, JAHNG TA, HYUN SJ, et al. Expansive Laminoplasty Versus Laminectomy Alone Versus Laminectomy and Fusion for Cervical Ossification of the Posterior Longitudinal Ligament: Is There a Difference in the Clinical Outcome and Sagittal Alignment?. Clin Spine Surg. 2016; 29(1):E9-E15. [17] STEPHENS BF, RHEE JM, NEUSTEIN TM, et al. Laminoplasty Does not Lead to Worsening Axial Neck Pain in the Properly Selected Patient With Cervical Myelopathy: A Comparison With Laminectomy and Fusion. Spine (Phila Pa 1976). 2017;42(24):1844-1850. [18] PARACINO R, FASINELLA MR, MANCINI F, et al. Review of laminoplasty versus laminectomy in the surgical management of cervical spondylotic myelopathy. Surg Neurol Int. 2021;12:44.. [19] 郑博隆,郝定均,杨小彬,等.单开门椎板成形术和椎板切除并侧块螺钉内固定术治疗颈椎后纵韧带骨化症的疗效比较[J].脊柱外科杂志, 2018,16(1):14-21. [20] LEE SH, SUK KS, KANG KC, et al. Outcomes and Related Factors of C5 Palsy Following Cervical Laminectomy With Instrumented Fusion Compared With Laminoplasty. Spine (Phila Pa 1976). 2016;41(10):E574-E579. [21] EPSTEIN NE. Commentary on article: Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: A meta-analysis of clinical and radiological outcomes by Chang-Hyun Lee et al. Surg Neurol Int. 2015;6(Suppl 14):S379-S382. [22] LIN S, ZHOU F, SUN Y, et al. The severity of operative invasion to the posterior muscular-ligament complex influences cervical sagittal balance after open-door laminoplasty. Eur Spine J. 2015;24(1):127-135. [23] FUNABA M, IMAJO Y, SUZUKI H, et al. The Deterioration of Cervical Kyphosis During Neck Flexion after Laminoplasty Affects the Surgical Outcome of Cervical Spondylotic Myelopathy. Global Spine J. 2023;13(8): 2497-2507. [24] 严宏伟. 后路经肌间隙保留伸肌群的颈椎椎板成形术治疗脊髓型颈椎病[J]. 颈腰痛杂志,2022,43(2):287-288. [25] ISEDA K, TAKAHASHI K, NAKAJIMA M. Indication of C2-C7 Cervical Laminoplasty with Muscle and Ligament Preservation in Patients with Kyphosis. World Neurosurg. 2023;175:e44-e54. [26] IIZUKA H, NAKAJIMA T, IIZUKA Y, et al. Cervical malalignment after laminoplasty: relationship to deep extensor musculature of the cervical spine and neurological outcome. J Neurosurg Spine. 2007;7(6):610-614. [27] KIM TH, LEE SY, KIM YC, et al. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976). 2013;38(16):E992-E997. [28] ZHANG JT, LI JQ, NIU RJ, et al. Predictors of cervical lordosis loss after laminoplasty in patients with cervical spondylotic myelopathy. Eur Spine J. 2017;26(4):1205-1210. [29] LI XY, KONG C, SUN XY, et al. Influence of the Ratio of C2-C7 Cobb Angle to T1 Slope on Cervical Alignment After Laminoplasty. World Neurosurg. 2019;124:e659-e666. [30] CHENG X, CHEN Z, SUN X, et al. Favorable cervical extension capacity preventing loss of cervical lordosis after laminoplasty due to spontaneous restoration of initial lordosis. Spine J. 2024;24(1):94-100. |
| [1] | Zhang Rui, Wang Kun, Shen Zicong, Mao Lu, Wu Xiaotao. Effects of endoscopic foraminoplasty and laminoplasty on biomechanical properties of intervertebral disc and isthmus [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 833-839. |
| [2] | Sun Jun, Zhan Mingbin, Liu Xizhe, Liu Shaoyu. Comparison of the opening angle and cervical vertebra function of two different hinge rongeurs in French-door laminoplasty [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(27): 4337-4344. |
| [3] | Ling Xiaoming, Zhang Chunlin, Yan Xu, Shao Chenglong. Cervical microendoscopic laminoplasty remarkably improves cervical curvature in the treatment of the spinal cord line type III cervical spondylotic myelopathy [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(22): 3555-3560. |
| [4] | Niu Cehao, Zhang Chunlin, Yan Xu, Fu Su, Feng Yang, Zhu Andi. Posterior vertebral structure and its influence on measurement of disc herniation volume [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(18): 2897-2902. |
| [5] | Lu Pan, Zhang Chunlin, Wang Yongkui, Yan Xu, Dong Chao, Yue Yisen, Li Long, Zhu Andi. Volume changes of cervical herniated discs after open-door laminoplasty and conservative treatment as assessed by three-dimensional volume method [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1395-1401. |
| [6] | Zhong Hua, Guan Haishan. C2 and C3 vertebral arch bone impact after posterior cervical single open-door laminoplasty: lateral X-ray evaluation of cervical spine within 2 years [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(36): 5862-5867. |
| [7] | Li Long, Zhang Chunlin, Shao Chenglong, Yan Xu, Wang Yongkui, Liu Xiaokang, Li Dongzhe. Evaluation of natural resorption of herniated cervical intervertebral disc with different degrees of degeneration after cervical microendoscopic laminoplasty by three-dimensional volume method [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(36): 5832-5837. |
| [8] | Zhao Lingtong, Hu Bing. Modified open-door laminoplasty with preserved posterior cervical musculo-ligamentous complex in the treatment of cervical spondylotic myelopathy: neurological function and axial symptoms [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(33): 5345-5350. |
| [9] | Zhang Chunlin, Zhao Xiao, Yan Xu, Ning Yongming, Cao Zhengming. Cervical microendoscopic laminoplasty and intervertebral disc resorption after conservative treatment assessed with three-dimensional volume method [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(30): 4774-4780. |
| [10] | Wu Yanyu, Zhang Chunlin, Shao Chenglong, Yan Xu, Liu Xiaokang, Wang Yongkui, Li Dongzhe. Quantitative measurement of resorption of cervical herniated disc after cervical microendoscopic laminoplasty by two-dimensional distance method and three-dimensional volume method [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3390-3394. |
| [11] |
Zhang Chunlin, Liu Yang, Shang Lijie, Yan Xu, Ning Yongming, Li Dongzhe, Dong Chao, Cao Zhengming.
Observation of herniated
cervical intervertebral disc volume based on quantitative volume measurement “monitoring” based on PACS software |
| [12] | Chen Yuyue, Zou Xiaobao, Ma Xiangyang, Wang Binbin, Yang Haozhi, Ge Su, Zhang Shuang, Ni Ling, Xia Hong, Wu Zenghui. Comparison of cervical motion range and curvature after C3 laminectomy and mini-titanium plate fixation after single-door vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(12): 1805-1809. |
| [13] | Chang Jianzhong, Xiao Wei, Jin Qi, Sun Chengjun, Zhou Yichi, Zhao Zufa, Mao Xiaobing. C3 laminectomy versus C3 laminoplasty for treating multi-segment cervical spondylotic myelopathy: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(16): 2608-2613. |
| [14] | Wang Wei, Ma Junfeng, Cui Zijian, Zhang Lilong, Jiang Zehua, Lu Yun. Meta-analysis of posterior cervical laminectomy titanium mini-plate versus lateral mass screw fixation for treating multilevel cervical spondylotic myelopathy [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(16): 2614-2624. |
| [15] | Liang Wei-zhi, Gao Jin-wei, Fu Lei, Cui Xiao-hu, Jia Jun-feng. Two kinds of decompression and implant internal fixation for the treatment of cervical spinal stenosis: C5 nerve root palsy and stability [J]. Chinese Journal of Tissue Engineering Research, 2013, 17(35): 6345-6350. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||