Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (5): 1003-1012.doi: 10.12307/2025.282
Previous Articles Next Articles
Metformin exerts a protective effect on articular cartilage in osteoarthritis rats by inhibiting the PI3K/AKT/mTOR pathway
Xu Tianjie1, Fan Jiaxin1, Guo Xiaoling1, Jia Xiang1, Zhao Xingwang2, Liu kainan3, Wang Qian1
- 1School of Basic Medical Sciences, North China University of Science and Technology, Tangshan 063000, Hebei Province, China; 2Department of Orthopedics, Affiliated Hospital of North China University of Science and Technology, Tangshan 063000, Hebei Province, China; 3College of Basic Medicine, Xingtai Medical College, Xingtai 054000, Hebei Province, China
-
Received:2023-12-25Accepted:2024-02-29Online:2025-02-18Published:2024-06-04 -
Contact:Wang Qian, MD, Associate professor, Master’s supervisor, School of Basic Medical Sciences, North China University of Science and Technology, Tangshan 063000, Hebei Province, China -
About author:Xu Tianjie, Master, School of Basic Medical Sciences, North China University of Science and Technology, Tangshan 063000, Hebei Province, China
CLC Number:
Cite this article
Xu Tianjie, Fan Jiaxin, Guo Xiaoling, Jia Xiang, Zhao Xingwang, Liu kainan, Wang Qian. Metformin exerts a protective effect on articular cartilage in osteoarthritis rats by inhibiting the PI3K/AKT/mTOR pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1003-1012.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

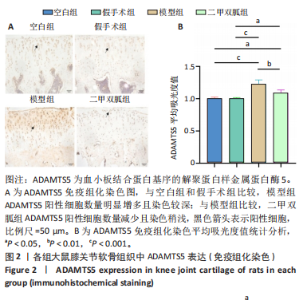
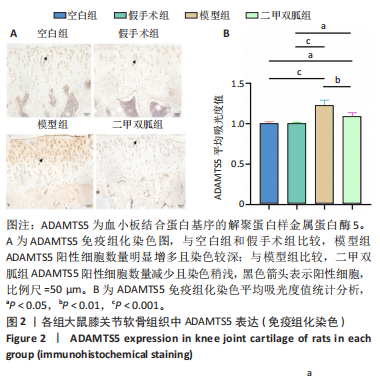
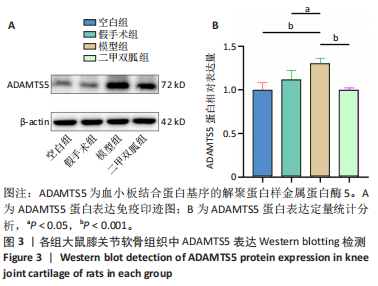
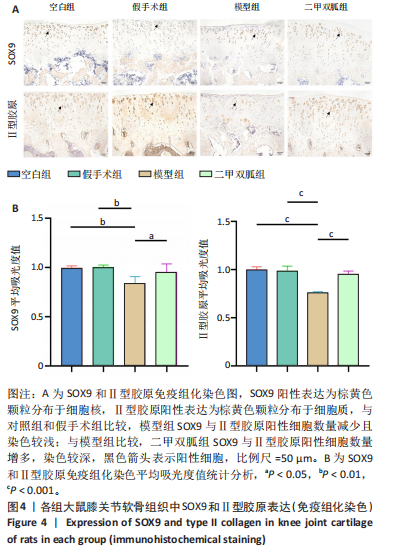
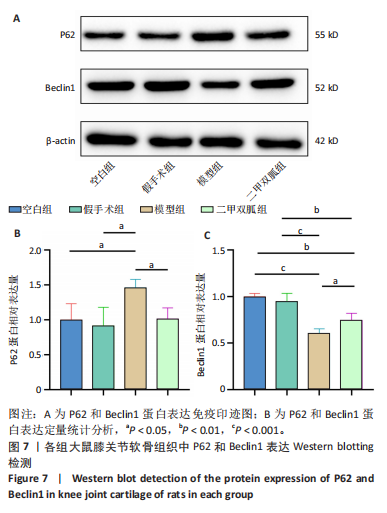
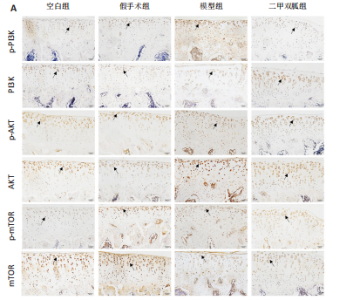
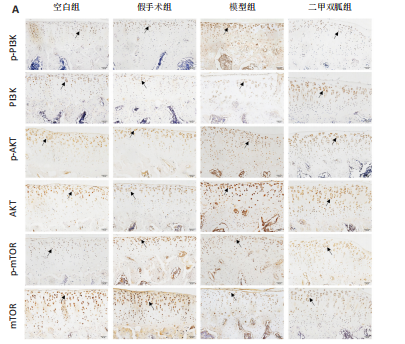
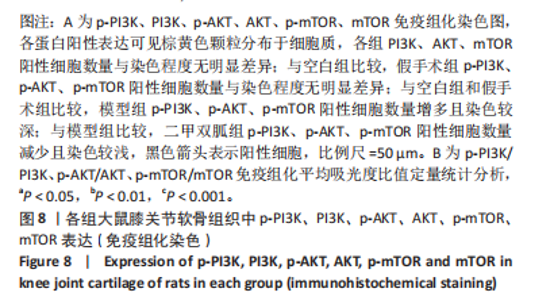
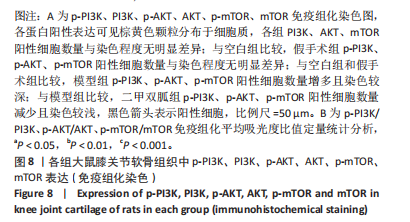
2.1 实验动物数量分析 40只SD大鼠全部进入结果分析。 2.2 各组大鼠膝关节软骨病理观形态察结果 见图1。 苏木精-伊红染色结果显示,空白组软骨表面光滑,组织形态正常,软骨细胞单个排列,假手术组软骨形态与空白组无明显差别;模型组软骨表面不规则,软骨组织出现缺损,软骨层变薄,软骨细胞呈簇状分布且细胞数量减少;二甲双胍组软骨表面光滑,软骨层明显增厚,软骨细胞数量增多且排列整齐。 甲苯胺蓝染色结果显示,空白组和假手术组软骨细胞可见蓝紫色的细胞核,软骨基质中的蛋白多糖染色均匀,呈蓝色或蓝紫色,潮线完整;模型组软骨细胞数量减少,软骨基质中的蛋白多糖染色较浅,潮线不完整;相较于模型组,二甲双胍组软骨细胞数量增多,软骨基质染色深染,但略浅于空白组和假手术组。 番红O-固绿染色结果显示,空白组和假手术组软骨细胞可见蓝色的细胞核,软骨基质染色均匀,呈红色,潮线完整;模型组软骨细胞数量减少,部分软骨组织番红染色较浅,潮线不完整;二甲双胍组软骨细胞数量增多,潮线完整,软骨基质较模型组深染,但仍浅于空白组和假手术组。 空白组、假手术组、模型组与二甲双胍组大鼠膝关节软骨Mankin评分分别为0,0.33±0.50,5.67±1.12,1.56±0.73,空白组与假手术组Mankin评分比较差异无显著性意义(P > 0.05),二甲双胍组、模型组Mankin评分高于空白组和假手术组(P < 0.05),二甲双胍组Mankin评分低于模型组(P < 0.05)。 2.3 各组大鼠膝关节软骨组织中ADAMTS5表达 免疫组化染色结果显示,各组大鼠膝关节软骨组织软骨细胞内均有不同程度ADAMTD5蛋白表达,可见棕黄色颗粒分布于细胞质内。与空白组比较,假手术组ADAMTS5阳性细胞数量与染色程度无明显差异;与空白组和假手术组比较,模型组ADAMTS5阳性细胞数量明显增多且染色较深;与模型组比较,二甲双胍组ADAMTS5阳性细胞数量减少且染色稍浅,见图2A。免疫组化染色平均吸光度值分析结果显示,假手术组大鼠软骨组织中ADAMTS5蛋白阳性表达与空白组比较无明显差异(P > 0.05);与空白组和假手术组比较,模型组大鼠软骨组织中ADAMTD5蛋白阳性表达增多(P < 0.01);与模型组比较,二甲双胍组大鼠软骨组织中ADAMTS5蛋白阳性表达降低(P < 0.01),见图2B。 Western blotting检测结果显示,与空白组比较,假手术组大鼠软骨组织中ADAMTS5蛋白表达无明显差异(P > 0.05);与空白组和假手术组比较,模型组大鼠软骨组织中ADAMTD5表达升高(P < 0.001,P < 0.05);与模型组比较,二甲双胍组大鼠软骨组织中ADAMTS5蛋白表达降低(P < 0.001),见图3。Western blotting检测结果与免疫组化学染色结果一致。 2.4 各组骨关节炎大鼠软骨组织中SOX9和Ⅱ型胶原表达 免疫组化染色结果显示,各组软骨组织软骨细胞内均有不同程度SOX9和Ⅱ型胶原蛋白表达,SOX9阳性表达为棕黄色颗粒分布于细胞核,Ⅱ型胶原阳性表达为棕黄色颗粒分布于细胞质。与空白组比较,假手术组SOX9和Ⅱ型胶原阳性细胞数量与染色程度无明显差异;与对照组和假手术组比较,模型组SOX9与Ⅱ型胶原阳性细胞数量减少且染色较浅;与模型组比较,二甲双胍组SOX9与Ⅱ型胶原阳性细胞数量增多,染色较深,见图4A。免疫组化染色平均吸光度值分析结果显示,假手术组软骨组织中SOX9和Ⅱ型胶原蛋白表达与空白组无明显差异(P > 0.05);与空白组和假手术组比较,模型组软骨组织中SOX9和Ⅱ型胶原蛋白表达降低(P < 0.01或P < 0.001);与模型组比较,二甲双胍组软骨组织中SOX9和Ⅱ型胶原蛋白表达升高 (P < 0.05,P < 0.001),见图4B。 Western blotting检测结果显示,假手术组与空白组软骨组织中SOX9和Ⅱ型胶原蛋白表达无明显差异(P > 0.05);与空白组和假手术组比较,模型组软骨组织中SOX9和Ⅱ型胶原蛋白表达降低(P < 0.01或P < 0.001);与模型组比较,二甲双胍组软骨组织中SOX9和Ⅱ型胶原蛋白升高(P < 0.05,P < 0.01),但仍低于空白组(P < 0.05),见图5。Western blotting检测结果与免疫组化染色结果 一致。 2.5 各组大鼠膝关节软骨组织中P62、Beclin1表达 免疫组化染色结果显示,各组软骨组织软骨细胞内均有不同程度的P62和Beclin1蛋白表达,P62与Beclin1阳性表达均呈棕黄色分布于细胞质内。与空白组比较,假手术组P62与Beclin1阳性细胞数量与染色程度无明显差异;与空白组和假手术组比较,模型组P62阳性细胞数量增多且染色较深,Beclin1阳性细胞数量减少且染色较浅;与模型组比较,二甲双胍组P62阳性细胞数量减少且染色较浅,Beclin1阳性细胞数量增多且染色较染,见图6A。免疫组化染色图平均吸光度值分析分析显示,空白组软骨组织中P62、Beclin1蛋白表达与假手术组无明显差异(P > 0.05);与空白组和假手术组比较,模型组软骨组织中P62蛋白表达升高(P < 0.01),Beclin1蛋白表达降低(P < 0.001);与模型组比较,二甲双胍组软骨组织中P62蛋白表达降低 (P < 0.05),Beclin1蛋白表达升高(P < 0.05),见图6B。 Western blotting检测结果显示,空白组软骨组织中P62、Beclin1蛋白表达与假手术组无明显差异(P > 0.05);与空白组和假手术组比较,模型组软骨组织中P62蛋白表达升高(P < 0.05),Beclin1蛋白表达降低(P < 0.001);与模型组比较,二甲双胍组软骨组织中P62蛋白表达降低(P < 0.05),Beclin1蛋白表达升高(P < 0.05),见图7。Western blotting检测结果与免疫组化染色结果一致。 2.6 各组大鼠膝关节软骨组织中PI3K/AKT/mTOR信号通路蛋白表达 免疫组化染色结果显示,各组软骨组织软骨细胞内均有不同程度的PI3K、p-PI3K、AKT、p-AKT、mTOR、p-mTOR蛋白表达,各蛋白阳性表达可见棕黄色颗粒分布于细胞质。各组PI3K、AKT、mTOR阳性细胞数量与染色程度无明显差异;与空白组比较,假手术组p-PI3K、p-AKT、p-mTOR阳性细胞数量与染色程度无明显差异;与空白组和假手术组比较,模型组p-PI3K、p-AKT、p-mTOR阳性细胞数量增多且染色较深;与模型组比较,二甲双胍组p-PI3K、p-AKT、p-mTOR阳性细胞数量减少且染色较浅,见图8A。免疫组化染色染色平均吸光度值定量分析结果显示,假手术组p-PI3K/PI3K、p-AKT/AKT和p-mTOR/mTOR蛋白平均吸光度比值与空白组比较差异无显著性意义(P > 0.05);与空白组和假手术组比较,模型组p-PI3K/PI3K、p-AKT/AKT和p-mTOR/mTOR蛋白平均吸光度比值升高(P < 0.01或P < 0.001);与模型组比较,二甲双胍组p-PI3K/PI3K、p-AKT/AKT和p-mTOR/mTOR蛋白平均吸光度比值降低(P < 0.05),见图8B。 Western blotting检测结果显示,各组PI3K、AKT、mTOR蛋白表达比较差异无显著性意义(P > 0.05);假手术组p-PI3K、p-AKT、p-mTOR蛋白表达与空白组比较差异无显著性意义(P > 0.05);与空白组和假手术组比较,模型组p-PI3K、p-AKT、p-mTOR蛋白表达升高(P < 0.05,或P < 0.01或P < 0.001);与模型组比较,二甲双胍组p-PI3K、p-AKT、p-mTOR蛋白表达降低(P < 0.05),见图9。 "

| [1] CAI X, YUAN S, ZENG Y, et al. New Trends in Pharmacological Treatments for Osteoarthritis. Front Pharmacol. 2021;12:645842. [2] LONG H, LIU Q, YIN H, et al. Prevalence Trends of Site-Specific Osteoarthritis From 1990 to 2019: Findings From the Global Burden of Disease Study 2019. Arthritis Rheumatol. 2022;74(7):1172-1183. [3] HE Y, LI Z, ALEXANDER PG, et al. Pathogenesis of Osteoarthritis: Risk Factors, Regulatory Pathways in Chondrocytes, and Experimental Models. Biology (Basel). 2020;9(8):194. [4] FUGGLE N, CURTIS E, SHAW S, et al. Safety of Opioids in Osteoarthritis: Outcomes of a Systematic Review and Meta-Analysis. Drugs Aging. 2019;36(Suppl 1):129-143. [5] YAO Q, WU X, TAO C, et al. Osteoarthritis: pathogenic signaling pathways and therapeutic targets. Signal Transduct Target Ther. 2023; 8(1):56. [6] BLASIOLI DJ, KAPLAN DL. The Roles of Catabolic Factors in the Development of Osteoarthritis. Tissue Eng Part B Rev. 2014;20(4): 355-363. [7] PARK C, JEONG JW, LEE DS, et al. Sargassum serratifolium Extract Attenuates Interleukin-1β-Induced Oxidative Stress and Inflammatory Response in Chondrocytes by Suppressing the Activation of NF-κB, p38 MAPK, and PI3K/Akt. Int J Mol Sci. 2018;19(8):2308. [8] SUN K, LUO J, GUO J, et al. The PI3K/AKT/mTOR signaling pathway in osteoarthritis: a narrative review. Osteoarthritis Cartilage. 2020;28(4): 400-409. [9] ALA M, ALA M. Metformin for Cardiovascular Protection, Inflammatory Bowel Disease, Osteoporosis, Periodontitis, Polycystic Ovarian Syndrome, Neurodegeneration, Cancer, Inflammation and Senescence: What Is Next? ACS Pharmacol Transl Sci. 2021;4(6):1747-1770. [10] PARK MJ, MOON SJ, BAEK JA, et al. Metformin Augments Anti-Inflammatory and Chondroprotective Properties of Mesenchymal Stem Cells in Experimental Osteoarthritis. J Immunol. 2019;203(1):127-136. [11] LI J, ZHANG B, LIU WX, et al. Metformin limits osteoarthritis development and progression through activation of AMPK signalling. Ann Rheum Dis. 2020;79(5):635-645. [12] YAN J, FENG G, MA L, et al. Metformin alleviates osteoarthritis in mice by inhibiting chondrocyte ferroptosis and improving subchondral osteosclerosis and angiogenesis. J Orthop Surg Res. 2022;17(1):333. [13] YAN S, DONG W, LI Z, et al. Metformin regulates chondrocyte senescence and proliferation through microRNA-34a/SIRT1 pathway in osteoarthritis. J Orthop Surg Res. 2023;18(1):198. [14] WANG J, WANG X, CAO Y, et al. Therapeutic potential of hyaluronic acid/chitosan nanoparticles for the delivery of curcuminoid in knee osteoarthritis and an in vitro evaluation in chondrocytes. Int J Mol Med. 2018;42(5):2604-2614. [15] 冯晓峰,张荣凯,祁伟仲,等.二甲双胍干预骨关节炎模型小鼠早期骨关节炎软骨及软骨下骨变化[J]. 中国组织工程研究,2019, 23(19):3031-3036. [16] YAN J, DING D, FENG G, et al. Metformin reduces chondrocyte pyroptosis in an osteoarthritis mouse model by inhibiting NLRP3 inflammasome activation. Exp Ther Med. 2022;23(3):222. [17] 罗臻,李宏栩,卢启贵,等.红姜提取物保护早期膝骨关节炎模型大鼠的关节软骨[J].中国组织工程研究,2021,25(32):5155-5161. [18] HWANG HS, KIM HA. Chondrocyte Apoptosis in the Pathogenesis of Osteoarthritis. Int J Mol Sci. 2015;16(11):26035-26054. [19] FANELLI A, GHISI D, APRILE PL, et al. Cardiovascular and cerebrovascular risk with nonsteroidal anti-inflammatory drugs and cyclooxygenase 2 inhibitors: latest evidence and clinical implications. Ther Adv Drug Saf. 2017;8(6):173-182. [20] LIN H, AO H, GUO G, et al. The Role and Mechanism of Metformin in Inflammatory Diseases. J Inflamm Res. 2023;16:5545-5564. [21] JIN P, JIANG J, ZHOU L, et al. Disrupting metformin adaptation of liver cancer cells by targeting the TOMM34/ATP5B axis. EMBO Mol Med. 2022;14(12):e16082. [22] MARTIN-MONTALVO A, MERCKEN EM, MITCHELL SJ, et al. Metformin improves healthspan and lifespan in mice. Nat Commun. 2013;4:2192. [23] SANCHEZ-LOPEZ E, CORAS R, TORRES A, et al. Synovial inflammation in osteoarthritis progression. Nat Rev Rheumatol. 2022;18(5): 258-275. [24] KRISHNAN Y, GRODZINSKY AJ. Cartilage Diseases. Matrix Biol. 2018;71-72:51-69. [25] MARTÍNEZ-MORENO D, JIMÉNEZ G, GÁLVEZ-MARTÍN P, et al. Cartilage biomechanics: A key factor for osteoarthritis regenerative medicine. Biochim Biophys Acta Mol Basis Dis. 2019;1865(6):1067-1075. [26] HUSSAIN S, SUN M, GUO Y, et al. SFMBT2 positively regulates SOX9 and chondrocyte proliferation. Int J Mol Med. 2018;42(6):3503-3512. [27] XU R, WU J, ZHENG L, et al. Undenatured type II collagen and its role in improving osteoarthritis. Ageing Res Rev. 2023;91:102080. [28] LI T, PENG J, LI Q, et al. The Mechanism and Role of ADAMTS Protein Family in Osteoarthritis. Biomolecules. 2022;12(7):959. [29] YAO M, ZHANG C, NI L, et al. Cepharanthine Ameliorates Chondrocytic Inflammation and Osteoarthritis via Regulating the MAPK/NF-κB-Autophagy Pathway. Front Pharmacol. 2022;13:854239. [30] SUN K, JING X, GUO J, et al. Mitophagy in degenerative joint diseases. Autophagy. 2021;17(9):2082-2092. [31] 谢一潋,杨乃彬,王丽萍,等.姜黄素通过激活肝细胞自噬减轻脂多糖/D-氨基半乳糖诱导的大鼠急性肝损伤[J].中国病理生理杂志, 2020,36(5):860-864. [32] 管津智,姜泉,夏聪敏,等.清热活血方对CIA大鼠自噬相关蛋白p62表达的影响[J].中国中医基础医学杂志,2023,29(4):588-592. [33] BOUDERLIQUE T, VUPPALAPATI KK, NEWTON PT, et al. Targeted deletion of Atg5 in chondrocytes promotes age-related osteoarthritis. Ann Rheum. 2016;75(3):627-631. [34] LV X, ZHAO T, DAI Y, et al. New insights into the interplay between autophagy and cartilage degeneration in osteoarthritis. Front Cell Dev Biol. 2022;10:1089668. [35] HAYER S, PUNDT N, PETERS MA, et al. PI3Kgamma regulates cartilage damage in chronic inflammatory arthritis. FASEB J. 2009;23(12): 4288-4298. [36] AZIZ AUR, FARID S, QIN K, et al. PIM Kinases and Their Relevance to the PI3K/AKT/mTOR Pathway in the Regulation of Ovarian Cancer. Biomolecules. 2018;8(1):E7. [37] ZHOU J, JIANG Y, CHEN H, et al. Tanshinone I attenuates the malignant biological properties of ovarian cancer by inducing apoptosis and autophagy via the inactivation of PI3K/AKT/mTOR pathway. Cell Prolif. 2019;53(2): e12739. [38] WANG K, CHU M, WANG F, et al. Putative functional variants of PI3K/AKT/mTOR pathway are associated with knee osteoarthritis susceptibility. J Clin Lab Anal. 2020;34(6):e23240. [39] LI J, JIANG M, YU Z, et al. Artemisinin relieves osteoarthritis by activating mitochondrial autophagy through reducing TNFSF11 expression and inhibiting PI3K/AKT/mTOR signaling in cartilage. Cell Mol Biol Lett. 2022;27(1):62. |
| [1] | Yin Lu, Jiang Chuanfeng, Chen Junjie, Yi Ming, Wang Zihe, Shi Houyin, Wang Guoyou, Shen Huarui. Effect of Complanatoside A on the apoptosis of articular chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1541-1547. |
| [2] | Li Huayuan, Li Chun, Liu Junwei, Wang Ting, Li Long, Wu Yongli. Effect of warm acupuncture on PINK1/Parkin pathway in the skeletal muscle of rats with chronic fatigue syndrome [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1618-1625. |
| [3] | Zhou Panpan, Cui Yinglin, Zhang Wentao, Wang Shurui, Chen Jiahui, Yang Tong . Role of cellular autophagy in cerebral ischemic injury and the regulatory mechanism of traditional Chinese medicine [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1650-1658. |
| [4] | Zhu Hanmin, Wang Song, Xiao Wenlin, Zhang Wenjing, Zhou Xi, He Ye, Li Wei, . Mitophagy regulates bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1676-1683. |
| [5] | Zheng Rongfa, Mo Weibin, Huang Peng, Chen Junji, Liang Ting, Zi Fangyu, Li Guofeng. Effects of electroacupuncture on the expression of metabolic enzymes and autophagy genes in gastrocnemius muscle tissues of exercising rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1127-1136. |
| [6] | Chen Yuning, Jiang Ying, Liao Xiangyu, Chen Qiongjun, Xiong Liang, Liu Yue, Liu Tong. Buqi Huoxue Compounds intervene with the expression of related factors and autophagy related proteins in a rat model of cerebral ischemia/reperfusion [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1152-1158. |
| [7] | Liu Lingyun, He Guixin, Qin Weibin, Song Hui, Zhang Liwen, Tang Weizhi, Yang Feifei, Zhu Ziyi, Ou Yangbin . Improvement of myocardial injury by traditional Chinese medicine: mitochondrial calcium homeostasis mediates macrophage autophagy and pyroptosis pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1276-1284. |
| [8] | Wu Guangtao, Qin Gang, He Kaiyi, Fan Yidong, Li Weicai, Zhu Baogang, Cao Ying . Causal relationship between immune cells and knee osteoarthritis: a two-sample bi-directional Mendelian randomization analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1081-1090. |
| [9] | Ma Weibang, Xu Zhe, Yu Qiao, Ouyang Dong, Zhang Ruguo, Luo Wei, Xie Yangjiang, Liu Chen. Screening and cytological validation of cartilage degeneration-related genes in exosomes from osteoarthritis synovial fluid [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7783-7789. |
| [10] | Sima Xinli, Liu Danping, Qi Hui. Effect and mechanism of metformin-modified bone marrow mesenchymal stem cell exosomes on regulating chondrocytes [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7728-7734. |
| [11] | Liu Xuan, Ding Yuqing, Xia Ruohan, Wang Xianwang, Hu Shujuan. Exercise prevention and treatment of insulin resistance: role and molecular mechanism of Keap1/nuclear factor erythroid2-related factor 2 signaling pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7578-7588. |
| [12] | Gong Yuehong, Wang Mengjun, Ren Hang, Zheng Hui, Sun Jiajia, Liu Junpeng, Zhang Fei, Yang Jianhua, Hu Junping. Machine learning combined with bioinformatics screening of key genes for pulmonary fibrosis associated with cellular autophagy and experimental validation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7679-7689. |
| [13] | Zhang Fei, Zuo Jun. Inhibition of hypertrophic scar in rats by beta-sitosterol-laden mesoporous silica nanoparticles [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7301-7309. |
| [14] | Zhao Xuemei, Wang Rui, Ao · Wuliji, Bao Shuyin, Jiang Xiaohua. Effects of Agiophyllum Oligo Saccharides on inflammation and apoptosis of mouse synovial cells [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6939-6946. |
| [15] | Wu Zhenhua, Zhang Xiwei, Wang Yipin, Li Qianqian. Relationship between seven serum lipid traits and osteoarthritis: a large sample analysis of European population in IEU OPEN GWAS database [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 7004-7014. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||