Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (30): 6538-6546.doi: 10.12307/2025.950
Previous Articles Next Articles
Brain-computer interface combined with different therapies for limb dysfunction in stroke patients: effectiveness and mechanism analysis
Wang Xuesong1, 2, 3, Wang Yue1, 4, Xu Yan1, 2, 3, Zeng Wenhui1, 2, 3, Lu Wenming1, 2, Tang Xingkun1, 2, Chen Wenjie2, Ye Junsong1, 3, 5, 6
- 1Subcenter for Stem Cell Clinical Translation, First Affiliated Hospital of Gannan Medical University, Ganzhou 341000, Jiangxi Province, China; 2School of Rehabilitation Medicine, 4College of Nursing, Gannan Medical University, Ganzhou 341000, Jiangxi Province, China; 3Ganzhou Key Laboratory of Stem Cell and Regenerative Medicine, Ganzhou 341000, Jiangxi Province, China; 5Jiangxi Provincial Key Laboratory of Stem Cell and Regenerative Medicine, Ganzhou 341000, Jiangxi Province, China; 6Key Laboratory of Prevention and Treatment of Cardiovascular and Cerebrovascular Diseases, Ministry of Education, Ganzhou 341000, Jiangxi Province, China
-
Received:2024-10-08Accepted:2024-11-30Online:2025-10-28Published:2025-03-29 -
Contact:Ye Junsong, PhD, Professor, Subcenter for Stem Cell Clinical Translation, First Affiliated Hospital of Gannan Medical University, Ganzhou 341000, Jiangxi Province, China; Ganzhou Key Laboratory of Stem Cell and Regenerative Medicine, Ganzhou 341000, Jiangxi Province, China; Jiangxi Provincial Key Laboratory of Stem Cell and Regenerative Medicine, Ganzhou 341000, Jiangxi Province, China; Key Laboratory of Prevention and Treatment of Cardiovascular and Cerebrovascular Diseases, Ministry of Education, Ganzhou 341000, Jiangxi Province, China -
About author:Wang Xuesong, Master candidate, Subcenter for Stem Cell Clinical Translation, First Affiliated Hospital of Gannan Medical University, Ganzhou 341000, Jiangxi Province, China; School of Rehabilitation Medicine, Gannan Medical University, Ganzhou 341000, Jiangxi Province, China; Ganzhou Key Laboratory of Stem Cell and Regenerative Medicine, Ganzhou 341000, Jiangxi Province, China -
Supported by:National Natural Science Foundation of China, No. 32060232 (to YJS); Natural Science Foundation of Jiangxi Province, No. 20212BAB206075 (to YJS)
CLC Number:
Cite this article
Wang Xuesong, Wang Yue, Xu Yan, Zeng Wenhui, Lu Wenming, Tang Xingkun, Chen Wenjie, Ye Junsong. Brain-computer interface combined with different therapies for limb dysfunction in stroke patients: effectiveness and mechanism analysis[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6538-6546.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
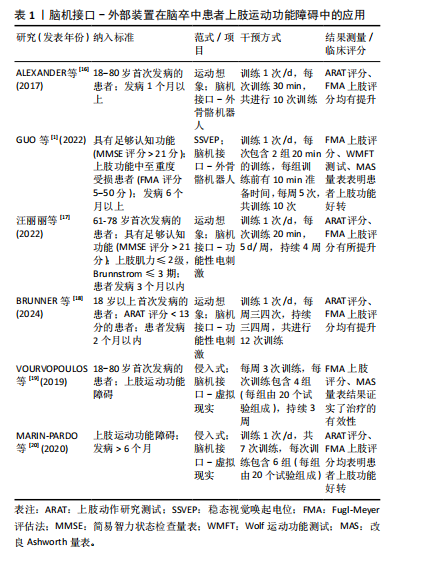
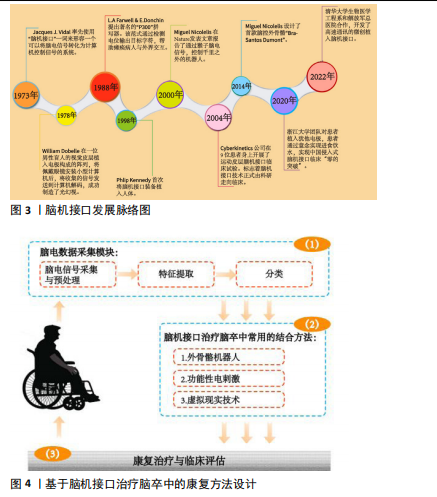
2.1 脑机接口治疗脑卒中患者肢体功能障碍的应用 基于脑电图的脑机接口是一种不依赖人体外周神经传输及肌肉运动,在人脑与外界机器之间建立联系的新型人机交互技术。脑机接口技术首次被提出可以追溯到20世纪70年代,并在近50年来迅速发展,目前已经成为治疗脑卒中最具前景的技术之一,见图3。 脑机接口技术通过设备收集患者的脑电图并将其解码,最后以控制计算机光标或外骨骼机器人等外部设备来提供反馈。该方法通过将大脑活动信号间接转化为运动动作,进而促进参与运动神经控制环路的体感皮质激活,以达到脑卒中患者运动功能训练的目的[10]。目前,基于脑电图的脑机接口通过结合外骨骼机器人、功能性电刺激和虚拟现实技术对脑卒中患者肢体功能障碍有非常显著的治疗效果[11-14],见图4。 2.1.1 脑机接口治疗脑卒中上肢功能障碍 脑机接口技术最初在康复领域的探索动机实际上是用于重度脑卒中患者上肢功能障碍的恢复[15]。因为重度脑卒中患者并不具备接受作业治疗或诱导运动治疗等常规康复疗法所需的最低运动能力。近年来,临床上脑机接口治疗上肢功能障碍取得了令人满意的结果,见表1。"
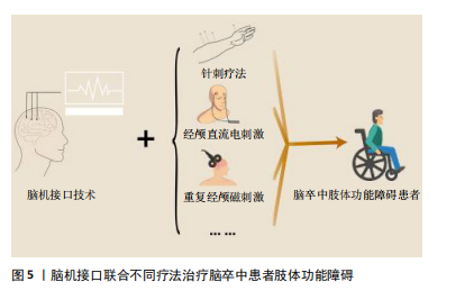
脑机接口结合外骨骼机器人是目前治疗脑卒中患者上肢功能障碍的主要形式,与常规康复疗法相比,外骨骼机器人可以进一步增强上肢运动功能[21-22],该方法主要通过提供感觉运动反馈并诱导大脑的可塑性,进而诱导受损的肢体运动能力[23]。脑卒中康复临床试验中,脑机接口-外骨骼机器人有不同类型的模式可供选择,如主动、被动和辅助模式[24-25],治疗师可根据患者的病情和损伤情况来匹配相应的模式。例如在被动模式下,麻痹肢体的运动完全由机器人控制,患者不进行任何运动;在辅助模式下,机器人则可以结合运动想象范式完成患者期望的肢体运动,这些模式对患者的运动进行运动学和动力学的测量,并通过扭矩、力、位置和关节角度等几个控制参数调整其功能[12]。虽然目前临床上报告了许多脑机接口结合外骨骼机器人治疗的满意结果,然而一项包含410例患者的随机对照临床研究结果表明,与结合外骨骼机器人相比,脑机接口与功能性电刺激可能是促进上肢功能恢复更好的组合[26]。 功能性电刺激疗法以自下而上的方式作用于患者,通过外周刺激诱导大脑的可塑性。将功能性电刺激连接到脑机接口系统,肌肉收缩成为患者意图的直接结果,将其转化为自上而下/自下而上的耦合周期,进一步促进大脑的可塑性。从脑机接口-功能性电刺激治疗严重的上肢瘫痪脑卒中患者结果观察到,脑机接口可以激活双侧大脑半球,显著增强大脑感觉运动皮质的事件相关去同步化,并使感觉运动皮质和顶叶激活[27]。另一项研究通过观察采用运动想象范式脑机接口结合功能性电刺激疗法患者的脑电图,发现脑电图模式逐渐集中并转移到感觉运动区和运动前区,患者在基于运动想象控制功能性电刺激系统的作用下,外周和中枢系统被同步激活,进一步促进了上肢运动功能的恢复[28]。 对比于外骨骼机器人及功能性电刺激,脑机接口与虚拟现实的结合在临床上越来越受欢迎。脑机接口-虚拟现实系统可以增加训练的吸引力来提高个人动机,从而通过促进脑功能的恢复改善患者的上肢功能[29-30]。VOURVOPOULOS等[31]首次将脑机接口与虚拟现实技术相结合,后续的研究中通过运动想象范式对1例男性脑卒中患者进行3周的训练治疗,大脑功能磁共振成像(fMRI)结果表明患者大脑激活区域增加,Fugl-Meyer评估(Fugl-Meyer Assessment,FMA)上肢评分显著提高[32]。 2.1.2 脑机接口治疗脑卒中下肢功能障碍 下肢功能障碍同样是脑卒中常见的功能损伤病症,主要表现在患者对下肢肌肉的运动控制和协调性受损,并使患者的行走能力被严重限制。目前脑机接口治疗脑卒中患者下肢功能障碍的疗效已被多项临床研究证实[33-34]。XIE等[35]开发了一种特殊的视觉刺激形式,以引起稳态运动视觉唤起电位,该范式可以克服光灯闪烁和对比度变化引起的视觉疲劳。该团队将稳态运动视觉唤起电位-脑机接口结合下肢康复机器人对31例脑卒中患者进行为期4周的下肢康复训练,随机对照临床研究结果显示患者下肢的FMA评分显著提高[36]。 功能性电刺激在临床上已被广泛使用治疗脑卒中患者下肢功能障碍,其通过将电脉冲直接作用到股四头肌、胫骨前肌和腓肠肌等下肢肌肉群,有效刺激患者腿部肌肉的激活,并减少痉挛。研究人员通过将脑机接口与功能性电刺激相结合,对9例患者进行为期4周的治疗,并采用步态速度、主动背屈关节活动度、六分钟步行试验和FMA下肢评分对治疗效果进行评估,结果显示该疗法不同程度上改善了患者的行走速度和踝关节活动度,并提升了患者六分钟步行试验和FMA下肢评分[34]。此外,对比于单独使用功能性电刺激治疗,采用脑机接口-功能性电刺激训练后患肢行走的步速和节奏等方面均有更明显的恢复[37]。 如治疗上肢运动障碍一样,虚拟现实系统结合脑机接口在治疗脑卒中患者下肢功能障碍方面也非常具有潜力。研究人员让受试者在跑步机上行走,并将头皮收集的脑电图解码成下肢关节角度,以控制虚拟现实环境中的行走动画,通过该方法引导闭链运动,并观察8 d内受试者的下肢活动度恢复情况,结果证实在8 d后脑机接口-虚拟现实有效改善了患者的步态[38]。总之,脑机接口-虚拟现实通过让患者沉浸式感受丰富的视觉、听觉和触觉反馈,增强训练的趣味性并提升患者的主动参与感,有效促进大脑中运动控制相关的神经网络活化和功能重组,最终改善脑卒中患者的下肢运动功能。 2.2 基于不同策略提高脑机接口技术治疗脑卒中患者的上肢功能障碍 近年来鉴于脑机接口技术在康复领域的有效性,研究人员开发出了多种联合方法用于脑卒患者肢体功能的治疗。这些“鸡尾酒式”的联合手段通过不同的治疗机制产生了有价值的融合,见图5。"
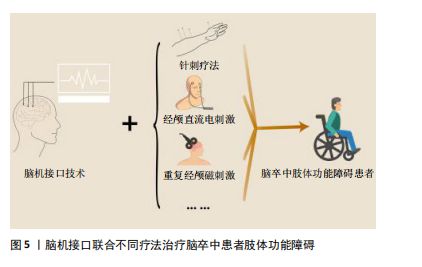
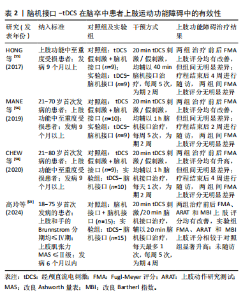
2.2.1 脑机接口技术联合中医疗法治疗脑卒中患者的上肢功能障碍 肌肉痉挛是脑卒中患者发病后的常见表征,其归属于中医学“症证”“筋病”范畴。在《灵枢·经筋》中有“经筋治病,寒则反折筋急;热则筋弛纵不收,阴痿不用”,意为经筋之病,遇冷会出现拘挛的现象,而遇热会变得松弛。温针灸是将针刺与艾灸相结合的一种方法,具有温通经脉、行气活血的作用,许多临床和循证医学的结果也证实温针灸可以调治肢体运动功能障碍。研究人员通过温针灸联合运动想象-脑机接口技术对脑卒中患者进行4周的康复治疗,结果表明对比于单纯使用温针灸疗法,将温针灸与脑机接口训练有机结合可进一步改善患者上肢的运动功能[39]。头皮针抽提法源于《针灸问对》,被广泛用于临床上脑卒中患者的肢体肌力康复。另一项研究将其与运动想象-脑机接口技术联合治疗脑卒中上肢功能障碍,在为期4周的治疗后,相较于单纯使用头皮抽提法的患者上肢FMA评分以及改良Barthel指数显著提升,结果具有统计学差异[40]。马震震[41]通过将头电针结合运动想象-脑机接口技术治疗脑卒中患者的上肢功能障碍,对比于仅采用运动想象-脑机接口治疗,患者的FMA上肢运动功能、手臂动作测试评分在时间项具有统计学差异。此外,该研究表明联合治疗可加强患侧半球间的功能联系,主要针对患侧枕下回与患侧颞上回、颞中回及健侧海马,增强其连接功能,提示海马、丘脑等皮质下核团是联合疗法参与调控等重要脑区。联合疗法还能通过提高视空间处理功能网络之间的联系,诱导视觉网络-默认模式网络-额顶控制网络功能强化促进患者功能恢复。通过正电子发射计算机断层扫描对针刺后的大脑进行扫描发现,下丘脑、岛脑和皮质下结构的血流量增加[42]。除可以与传统针刺疗法的结合外,低频经皮穴位电刺激通过结合脑机接口在特定的穴位产生重复刺激调节脑功能区,对比常规康复疗法,患者上肢的FMA以及MAS评分显著提升[43]。另一项研究通过脑机接口-虚拟现实对患者进行“虚拟针灸”治疗,该研究并非在患者进行脑机接口-虚拟现实训练的基础上进行针灸治疗,而是通过虚拟现实模拟针灸感觉,通过对比患者进行针灸与“虚拟针灸”的脑电图,研究人员发现两者仅存在轻微的差异[44]。这表明基于脑机接口-虚拟现实技术的“虚拟针灸”作为科研和临床的创新方法是有希望的,该方法可以从神经及大脑的角度提供对针灸的透彻解释,并有效节省医疗资源。 2.2.2 脑机接口技术联合常规康复疗法治疗脑卒中患者的上肢功能障碍 除采用针刺疗法联合脑机接口治疗外,研究人员还通过绳带辅助本体感觉神经肌肉促进技术与脑机接口联合训练脑卒中患者的上肢功能[45]。分别采用香港版偏瘫上肢功能测试分级(FTHUE-HK)、FMA上肢功能评分和改良Barthel指数对患者治疗后上肢功能进行评估,结果证实以上方法具有良好的优越性。绳带疗法与本体感觉神经肌肉促进训练已被证实具有出色的兼容性,可以通过增强运动控制能力促进本体感觉,增强空间定向力改善患者的运动模式,将其与脑机接口结合可获得更好的治疗效果。该疗法通过中枢与外周的合并刺激进一步增强大脑上肢运动相关区域的激活,治疗机制遵循中枢-外周-中枢闭环康复理论[46],此外,一项基于296例患者的随机对照临床研究证实,与单纯进行常规康复训练相比,将其结合脑机接口技术可以进一步改善上肢运动功能[47]。脑机接口技术能够促进运动模式和神经肌肉联系的重建。将脑机接口技术与常规康复疗法相结合,可以帮助患者实现精确的运动控制和规划,并重新塑造大脑的运动信号,发挥协同和互补的作用。通过长期的联合训练,增强上肢的力量,并促进上肢运动功能的恢复。王建文等[48]通过脑机接口技术联合肩关节特定屈曲角度训练治疗脑卒中患者上肢功能障碍,对比单独使用脑机接口治疗,患者上肢的FMA、MAS评分明显升高。研究显示,脑机接口技术利用神经信号促进与外部设备的互动,从而使患者能够通过想象控制外部设备,并促进大脑神经重塑。在脑机接口训练上肢运动的基础上,肩关节特定屈曲角度训练侧重于在特定关节角度的运动重建。这种联合方法能够通过调整肩关节角度来准确定位并激活相关肌肉群,从而进一步增强患者对运动的控制和力量输出。 2.2.3 脑机接口技术联合物理因子疗法治疗脑卒中患者的上肢功能障碍 近年来物理因子疗法也被用于联合脑机接口技术治疗脑卒中患者肢体功能障碍。重复经颅磁刺激已被证明可以增加脑卒中患者病变半球的皮质兴奋性[49-50]。 通过重复经颅磁刺激联合脑机接口-虚拟现实训练治疗脑卒中患者,对比于单独采用重复经颅磁刺激治疗,患者的FMA上肢评分、FTHUE-HK分级及改良Barthel指数结果具有统计学意义上的提高[51]。脑机接口解码精度在实际应用中起着至关重要的作用,而重复经颅磁刺激使得皮质激活明显增强,这种生理特性的增强有助于提高脑机接口的解码精度,将两者结合可以功能互补,获得更好的治疗效果[52]。 经颅直流电刺激作为一种非侵入性的中枢刺激技术常用于神经调节和运动恢复,可以通过阳极刺激促进皮质兴奋,也可以通过阴极抑制皮质兴奋。此外,经颅直流电刺激还可以影响不同大脑区域之间的神经耦合,并调节运动想象时大脑的相位同步[53-54]。为调查经颅直流电刺激和脑机接口技术结合是否可以进一步改善患者上肢的运动障碍并探索治疗机制,研究人员应用神经成像来跟踪神经结构和功能的恢复[55],结果表明在慢性脑卒中患者进行经颅直流电刺激和运动想象-脑机接口训练治疗后,大脑白质结构和皮质功能的神经可塑性被进一步增强,运动相关区域之间运动兴奋性和大脑白质完整性的增加同样揭示联合治疗的增益作用。虽然该疗法在患者脑部发现了令人满意的结果,然而却并没有发现上肢功能障碍的改善。MANE等[56]将经颅直流电刺激治疗结合运动想象-脑机接口训练对脑卒中患者进行2周干预,结果发现对比于未使用经颅直流电刺激治疗的患者,联合治疗组受试者的事件相关去同步化水平明显升高,但同样未发现有明显的上肢功能改善。事件相关去同步化的机制被认为是由于底层神经元群体的同步性下降。由于阳极经颅直流电刺激增加大脑同侧M1区的皮质兴奋性[57],因此在进行运动想象时可能会导致更多的去同步神经元激活,进而促进感觉运动皮质和顶叶激活。另一项研究在对患者进行为期2周的联合治疗后也发现,运动想象-脑机接口训练可以改善脑卒中患者的上肢功能障碍,但与经颅直流电刺激的联合使用并没有使得上肢运动功能进一步好转[58]。然而,有研究与之相驳,高玲等[59]将视听觉和运动反馈脑机接口联合经颅直流电刺激治疗脑卒中上肢功能障碍,并对上肢功能进行评估,FMA上肢评分、上肢动作研究量表和改良Barthel指数结果均表明联合治疗效果要优于单独采用脑机接口或经颅直流电刺激治疗组。造成以上结论争议的原因可能是由于患者的选择所致。最近的文献表明,脑卒中后运动功能的恢复遵循相对可预测的“比例恢复规则” [60-62],该规则描述了恢复的可能性约为最大可能的70%。皮质脊髓束的完整性是决定遵守该规则的一个重要因素,那些没有完整的皮质脊髓束的患者往往是治疗规则的“不适应者”,若有更严重的损伤,则恢复能力更差,这也验证了经颅直流电刺激与脑机接口联合治疗结果在不同患者间的差异相对较大[63]。此外治疗时间也可能会导致结果出现差异性,当联合治疗的干预时间为2周时,联合治疗组相较于单纯脑机接口治疗组对患者上肢运动的改善无差异,然而当干预时间延长至4周时,联合治疗组的患者上肢FMA、ARAT和MBI评分显著升高,见表2。"
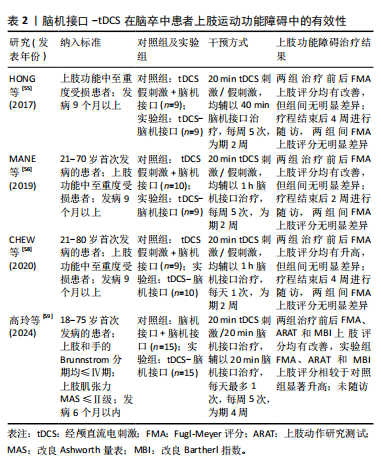

以上结果说明,经颅直流电刺激结合脑机接口作为脑卒中患者改善上肢功能的有效治疗策略目前还存在争议,如需采用此方法还需要进一步扩增样本数量以及长时间的回访调查以证明该策略的有效性。 2.3 基于不同策略提高脑机接口疗法治疗脑卒中患者的下肢功能障碍 行走功能障碍是脑卒中最不利的影响之一。中国有70%-80%的脑卒中患者因下肢功能障碍而无法独立生活,即使是在脑卒中后的慢性阶段,30%的患者也无法独立行走[64]。脑机接口技术作为一种可以增强神经可塑性的治疗方法,已在多项临床试验中证实可以促进脑卒中患者下肢功能障碍的恢复[65-66]。随着脑机接口技术在临床上的广泛使用,许多研究表明基于不同策略提高脑机接口对下肢功能障碍的治疗效果极具探究价值。 2.3.1 脑机接口联合常规康复疗法治疗脑卒中患者的下肢功能障碍 一项Meta分析对运动想象-脑机接口与常规康复疗法相结合的有效性进行了报道,从FMA下肢评分、改良Barthel指数、步长和节奏的结果来看,对比于仅采用常规康复疗法,这种联合策略可以进一步改善亚急性期和慢性期脑卒中患者下肢运动功能障碍[66]。常规的康复疗法在一定程度上可促进下肢运动功能的改善,但仍存在一些缺点,如常规疗法通常侧重于远端肢体调控,因此忽视了中枢脑神经可塑性的关键作用。而单一的运动想象训练对脑卒中患者步态的康复同样并没有显著的优势,因为在训练过程中单一的运动想象训练未能充分利用运动想象期间产生的生理特征信号,无法实现高效的闭环康复训练[67]。通过脑机接口提高中枢兴奋性,再辅以常规康复疗法,中枢干预与外周干预相辅相成,可以起到中枢-外周-中枢闭环康复训练的作用。一项随机对照临床研究揭示了常规康复疗法(物理治疗和针灸治疗)与其基础上接受脑机接口-功能性电刺激的疗效差别,结果表明在两组患者经过20次的治疗后,运动功能、行走功能和日常生活活动均有所改善,此外相较于常规康复治疗组,额外接受脑机接口-功能性电刺激治疗的患者FMA下肢评分显著升高[68]。 2.3.2 脑机接口联合物理因子疗法治疗脑卒中患者的下肢功能障碍 经颅直流电刺激与运动想象-脑机接口技术联合治疗脑卒中患者下肢功能障碍目前同样具有争议,研究人员通过fMRI数据采集单独使用运动想象-脑机接口和运动想象-脑机接口结合经颅直流电刺激治疗前后患者脑部的低频波动、区域同质性和功能连接性振幅,这些指标与患者大脑功能活动和连接性相关[69]。该研究结果揭示了运动想象-脑机接口对大脑功能重组的积极效果,然而对比于联合治疗组并没有发现明显的差异性,甚至出现相反的影响。此外,两种治疗方法均可以促进患者下肢FMA评分,但是组间无统计学差异。有学者提出了相反的观点,LIMA等[70]整合了一种新型联合治疗系统:包括经颅直流电刺激、运动想象-脑机接口、虚拟现实和可以通过脑电图控制的电动踏板,电动踏板以实时闭环设计提供运动训练,促进足部区域周围的皮质兴奋性,而脑机接口通过采集患者脑电指挥电动踏板。结果表明,受累肢体的运动功能、协调、速度以及感觉均有所提升,采用该联合方法可进一步增强脑部的神经可塑性。下肢复杂运动任务涉及大脑辅助运动区、M1、原发性体感皮质和运动前区,脑机接口联合经颅直流电刺激可加强大脑M1区域皮质兴奋性进而促进经颅直流电刺激固有的神经调节作用[71]。 总之,经颅直流电刺激联合脑机接口训练治疗下肢功能障碍的有效性需要进一步探究。造成以上结果的差异原因除患者的选择和治疗时间外,可能还与经颅直流电刺激不同的电极配置有关,研究表明经颅直流电刺激对脑机接口的性能有积极影响,然而,当经颅直流电刺激不对称设置时脑机接口的性能不会提升[72]。因此,未来还需进一步增加患者的样本量,并标准化干预的方式,以探究脑机接口联合不同策略治疗患者肢体功能障碍的有效性。"

| [1] GUO N, WANG X, DUANMU D, et al. SSVEP-Based Brain Computer Interface Controlled Soft Robotic Glove for Post-Stroke Hand Function Rehabilitation. IEEE Trans Neural Syst Rehabil Eng. 2022;30:1737-1744. [2] CAI S, ZHOU Y, YANG S, et al. The neural effects of acupuncture for stroke: a protocol for systematic review and meta-analysis based on fMRI. Front Neurosci. 2024;18:1443834. [3] LEBEDEV MA, NICOLELIS MA. Brain-Machine Interfaces: From Basic Science to Neuroprostheses and Neurorehabilitation. Physiol Rev. 2017;97(2):767-837. [4] WOLPAW JR, BIRBAUMER N, HEETDERKS WJ, et al. Brain-computer interface technology: a review of the first international meeting. IEEE Trans Rehabil Eng. 2000;8(2):164-173. [5] FARWELL LA, DONCHIN E. Talking off the top of your head: toward a mental prosthesis utilizing event-related brain potentials. Electroencephalogr Clin Neurophysiol. 1988;70(6):510-523. [6] PFURTSCHELLER G. Event-related synchronization (ERS): an electrophysiological correlate of cortical areas at rest. Electroencephalogr Clin Neurophysiol. 1992;83(1):62-69. [7] MIDDENDORF M, MCMILLAN G, CALHOUN G, et al. Brain-computer interfaces based on the steady-state visual-evoked response. IEEE Trans Rehabil Eng. 2000;8(2):21121-21124. [8] 丁晶,余情,唐莺莹,等.基于头皮脑电信号的无创脑机接口在神经系统疾病中的临床应用上海专家共识[J].上海医学,2024,47(4): 199-213. [9] 袁艳秋,张秀芳,陈杰,等.经颅电刺激技术联合脑机接口技术对脑卒中患者认知功能及上肢功能的影响[J].实用心脑肺血管病杂志,2024,32(4):71-75+79. [10] MASLOVA O, KOMAROVA Y, SHUSHARINA N, et al. Non-invasive EEG-based BCI spellers from the beginning to today: a mini-review. Front Hum Neurosci. 2023;17:1216648. [11] PICHIORRI F, MATTIA D. Brain-computer interfaces in neurologic rehabilitation practice. Handb Clin Neurol. 2020;168:101-116. [12] KHAN MA, DAS R, IVERSEN HK, et al. Review on motor imagery based BCI systems for upper limb post-stroke neurorehabilitation: From designing to application. Comput Biol Med. 2020;123:103843. [13] 杨帮华.运动想象脑机接口在神经系统疾病康复中的应用[J].康复学报, 2023,33(6):477-485. [14] 杨帮华,马骏,邱文政.面向脑卒中疾病的运动想象脑机接口技术[J].人工智能,2021(6):70-78. [15] MANE R, CHOUHAN T, GUAN C. BCI for stroke rehabilitation: motor and beyond. J Neural Eng. 2020;17(4):041001. [16] FROLOV AA, MOKIENKO O, LYUKMANOV R, et al. Post-stroke Rehabilitation Training with a Motor-Imagery-Based Brain-Computer Interface (BCI)-Controlled Hand Exoskeleton: A Randomized Controlled Multicenter Trial. Front Neurosci. 2017;11:400. [17] 汪丽丽,张颖,王春方,等.基于脑机接口的电刺激训练对脑卒中患者上肢功能障碍康复的临床研究 [J]. 生物医学工程与临床, 2022,26(2):163-168. [18] BRUNNER I, LUNDQUIST CB, PEDERSEN AR, et al. Brain computer interface training with motor imagery and functional electrical stimulation for patients with severe upper limb paresis after stroke: a randomized controlled pilot trial. J Neuroeng Rehabil. 2024;21(1):10. [19] VOURVOPOULOS A, PARDO OM, LEFEBVRE S, et al. Effects of a Brain-Computer Interface With Virtual Reality (VR) Neurofeedback: A Pilot Study in Chronic Stroke Patients. Front Hum Neurosci. 2019;13:210. [20] MARIN-PARDO O, LAINE CM, RENNIE M, et al. A Virtual Reality Muscle-Computer Interface for Neurorehabilitation in Chronic Stroke: A Pilot Study. Sensors (Basel). 2020;20(13):3754. [21] MEHRHOLZ J, POHL M, PLATZ T, et al. Electromechanical and robot-assisted arm training for improving activities of daily living, arm function, and arm muscle strength after stroke. Cochrane Database Syst Rev. 2018;9(9):Cd006876. [22] SWINNEN E, BECKWÉE D, MEEUSEN R, et al. Does robot-assisted gait rehabilitation improve balance in stroke patients? A systematic review. Top Stroke Rehabil. 2014;21(2):87-100. [23] ANG KK, CHUA KS, PHUA KS, et al. A Randomized Controlled Trial of EEG-Based Motor Imagery Brain-Computer Interface Robotic Rehabilitation for Stroke. Clin EEG Neurosci. 2015;46(4):310-320. [24] BASTERIS A, NIJENHUIS SM, STIENEN AH, et al. Training modalities in robot-mediated upper limb rehabilitation in stroke: a framework for classification based on a systematic review. J Neuroeng Rehabil. 2014;11:111. [25] SAID RR, HEYAT MBB, SONG K, et al. A Systematic Review of Virtual Reality and Robot Therapy as Recent Rehabilitation Technologies Using EEG-Brain-Computer Interface Based on Movement-Related Cortical Potentials. Biosensors (Basel). 2022;12(12):1134. [26] XIE L, YANG YX, JIANG H, et al. Brain-machine interface-based training for improving upper extremity function after stroke: A meta-analysis of randomized controlled trials. Front Neurosci. 2022;16:949575. [27] LI M, LIU Y, WU Y, et al. Neurophysiological substrates of stroke patients with motor imagery-based Brain-Computer Interface training. Int J Neurosci. 2014;124(6):403-415. [28] MIAO Y, CHEN S, ZHANG X, et al. BCI-Based Rehabilitation on the Stroke in Sequela Stage. Neural Plast. 2020;2020:8882764. [29] WEN D, LIANG B, ZHOU Y, et al. The Current Research of Combining Multi-Modal Brain-Computer Interfaces With Virtual Reality. IEEE J Biomed Health Inform. 2021;25(9):3278-3287. [30] NIETO-ESCAMEZ F, CORTÉS-PÉREZ I, OBRERO-GAITÁN E, et al. Virtual Reality Applications in Neurorehabilitation: Current Panorama and Challenges. Brain Sci. 2023;13(5):819. [31] VOURVOPOULOS A, BERMÚDEZ IBS. Motor priming in virtual reality can augment motor-imagery training efficacy in restorative brain-computer interaction: a within-subject analysis. J Neuroeng Rehabil. 2016;13(1):69. [32] VOURVOPOULOS A, JORGE C, ABREU R, et al. Efficacy and Brain Imaging Correlates of an Immersive Motor Imagery BCI-Driven VR System for Upper Limb Motor Rehabilitation: A Clinical Case Report. Front Hum Neurosci. 2019;13:244. [33] YUAN Z, PENG Y, WANG L, et al. Effect of BCI-Controlled Pedaling Training System With Multiple Modalities of Feedback on Motor and Cognitive Function Rehabilitation of Early Subacute Stroke Patients. IEEE Trans Neural Syst Rehabil Eng. 2021;29:2569-2577. [34] MCCRIMMON C M, KING C E, WANG P T, et al. Brain-controlled functional electrical stimulation therapy for gait rehabilitation after stroke: a safety study. J Neuroeng Rehabil. 2015;12:57. [35] XIE J, XU G, WANG J, et al. Steady-state motion visual evoked potentials produced by oscillating Newton’s rings: implications for brain-computer interfaces. PLoS One. 2012;7(6):e39707. [36] ZHAO CG, JU F, SUN W, et al. Effects of Training with a Brain-Computer Interface-Controlled Robot on Rehabilitation Outcome in Patients with Subacute Stroke: A Randomized Controlled Trial. Neurol Ther. 2022;11(2):679-695. [37] CHUNG E, LEE BH, HWANG S. Therapeutic effects of brain-computer interface-controlled functional electrical stimulation training on balance and gait performance for stroke: A pilot randomized controlled trial. Medicine (Baltimore). 2020;99(51):e22612. [38] LUU T P, HE Y, BROWN S, et al. Gait adaptation to visual kinematic perturbations using a real-time closed-loop brain-computer interface to a virtual reality avatar. J Neural Eng. 2016;13(3):036006. [39] 杨桂芬,汪亚群,李波,等.温针灸联合基于脑机接口技术的主动式康复训练治疗中风上肢痉挛性偏瘫27例[J].浙江中医杂志, 2023,58(9):673-674. [40] 杨桂芬,汪亚群,孙迪,等.头皮针抽提法联合基于脑机接口技术的主动式康复训练系统对脑卒中患者上肢运动功能康复的影响[J].浙江中医杂志,2022,57(9):676. [41] 马震震.脑机接口联合电针调控促进卒中后上肢运动功能恢复的临床机制研究[D].上海:上海中医药大学,2021. [42] HSIEH J C, TU CH, CHEN FP, et al. Activation of the hypothalamus characterizes the acupuncture stimulation at the analgesic point in human: a positron emission tomography study. Neurosci Lett. 2001; 307(2):105-108. [43] 辛辉,李鹏,李秀丽,等.低频经皮穴位电刺激联合平衡针与脑机接口技术对脑卒中患者上肢运动功能的影响[J].针灸临床杂志, 2022,38(10):10-15. [44] ZHANG Y, HUA W, ZHOU Z, et al. A novel acupuncture technique at the Zusanli point based on virtual reality and EEG: a pilot study. Front Neurosci. 2024;18:1269903. [45] 梁天佳,龙耀斌,陆丽燕,等.绳带辅助本体感觉神经肌肉促进技术训练联合绳带辅助脑机接口训练对脑卒中偏瘫上肢康复效果的随机对照试验[J].中国康复理论与实践,2024,30(8):972-978. [46] JIA J. Exploration on neurobiological mechanisms of the central-peripheral-central closed-loop rehabilitation. Front Cell Neurosci. 2022;16:982881. [47] WANG A, TIAN X, JIANG D, et al. Rehabilitation with brain-computer interface and upper limb motor function in ischemic stroke: A randomized controlled trial. Med. 2024;5(6):559-569.e4. [48] 王建文,王辉,党瑞.肩关节特定屈曲角度训练联合脑机接口训练对卒中后上肢运动功能障碍患者上肢运动功能及认知功能的影响[J].实用心脑肺血管病杂志,2024,32(11):115-119.
[49] ZHANG JJY, ANG J, SAFFARI SE, et al. Repetitive Transcranial Magnetic Stimulation for Motor Recovery After Stroke: A Systematic Review and Meta-Analysis of Randomized Controlled Trials With Low Risk of Bias. Neuromodulation. 2024:S1094-7159(24)00665-2. doi: 10.1016/j.neurom.2024.07.010. [50] CHEN M, HUANG Z, CHEN Y, et al. Repetitive Transcranial Magnetic Stimulation on Individualized Spots Based on Task functional Magnetic Resonance Imaging Improves Swallowing Function in Poststroke Dysphagia. Brain Connect. 2024;14(10):513-526. [51] 谭雅菲.重复经颅磁刺激联合脑机接口对脑卒中患者上肢运动功能的影响[D].石家庄:河北医科大学,2022. [52] SHU X, CHEN S, CHAI G, et al. Neural Modulation By Repetitive Transcranial Magnetic Stimulation (rTMS) for BCI Enhancement in Stroke Patients. Annu Int Conf IEEE Eng Med Biol Soc. 2018;2018: 2272-2275. [53] HE W, WEI P, ZHOU Y, et al. Modulation effect of transcranial direct current stimulation on phase synchronization in motor imagery brain-computer interface. Annu Int Conf IEEE Eng Med Biol Soc. 2014;2014: 1270-1273. [54] ZHANG S, GAO X, CUI H, et al. Transcranial Direct Current Stimulation-based Neuromodulation Improves the Performance of Brain-Computer Interfaces Based on Steady-State Visual Evoked Potential. IEEE Trans Neural Syst Rehabil Eng. 2023:PP. doi: 10.1109/TNSRE.2023.3245079. [55] HONG X, LU Z K, TEH I, et al. Brain plasticity following MI-BCI training combined with tDCS in a randomized trial in chronic subcortical stroke subjects: a preliminary study. Sci Rep. 2017;7(1):9222. [56] MANE R, CHEW E, PHUA KS, et al. Prognostic and Monitory EEG-Biomarkers for BCI Upper-Limb Stroke Rehabilitation. IEEE Trans Neural Syst Rehabil Eng. 2019;27(8):1654-1664. [57] NITSCHE M A, PAULUS W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol. 2000;527 Pt 3(Pt 3):633-639. [58] CHEW E, TEO WP, TANG N, et al. Using Transcranial Direct Current Stimulation to Augment the Effect of Motor Imagery-Assisted Brain-Computer Interface Training in Chronic Stroke Patients-Cortical Reorganization Considerations. Front Neurol. 2020;11:948. [59] 高玲,褚凤明,贾凡,等.基于视听觉和运动反馈的脑机接口结合经颅直流电刺激对脑卒中患者上肢功能的效果[J].中国康复理论与实践,2024,30(2):202-209. [60] BYBLOW WD, STINEAR CM, BARBER PA, et al. Proportional recovery after stroke depends on corticomotor integrity. Ann Neurol. 2015; 78(6):848-859. [61] WINTERS C, VAN WEGEN EE, DAFFERTSHOFER A, et al. Generalizability of the Proportional Recovery Model for the Upper Extremity After an Ischemic Stroke. Neurorehabil Neural Repair. 2015;29(7):614-622. [62] STINEAR CM, BYBLOW WD, ACKERLEY SJ, et al. Proportional Motor Recovery After Stroke: Implications for Trial Design. Stroke. 2017; 48(3):795-798. [63] ANG K K, GUAN C, PHUA K S, et al. Facilitating effects of transcranial direct current stimulation on motor imagery brain-computer interface with robotic feedback for stroke rehabilitation. Arch Phys Med Rehabil. 2015;96(3 Suppl):S79-S87. [64] ZHANG T, ZHAO J, LI X, et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of stroke rehabilitation. Stroke Vasc Neurol. 2020;5(3):250-259. [65] CALABRÒ RS, SORRENTINO G, CASSIO A, et al. Robotic-assisted gait rehabilitation following stroke: a systematic review of current guidelines and practical clinical recommendations. Eur J Phys Rehabil Med. 2021;57(3):460-471. [66] ZHAO LJ, JIANG LH, ZHANG H, et al. Effects of Motor Imagery Training for Lower Limb Dysfunction in Patients With Stroke: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Am J Phys Med Rehabil. 2023;102(5):409-418. [67] SILVA S, BORGES LR, SANTIAGO L, et al. Motor imagery for gait rehabilitation after stroke. Cochrane Database Syst Rev. 2020;9(9): Cd013019. [68] LUO X. Effects of motor imagery-based brain-computer interface-controlled electrical stimulation on lower limb function in hemiplegic patients in the acute phase of stroke: a randomized controlled study. Front Neurol. 2024;15:1394424. [69] HU M, CHENG HJ, JI F, et al. Brain Functional Changes in Stroke Following Rehabilitation Using Brain-Computer Interface-Assisted Motor Imagery With and Without tDCS: A Pilot Study. Front Hum Neurosci. 2021;15:692304. [70] LIMA JPS, SILVA LA, DELISLE-RODRIGUEZ D, et al. Unraveling Transformative Effects after tDCS and BCI Intervention in Chronic Post-Stroke Patient Rehabilitation-An Alternative Treatment Design Study. Sensors (Basel). 2023;23(23):9302. [71] RODRIGUEZ-UGARTE MS, IÁÑEZ E, ORTIZ-GARCIA M, et al. Effects of tDCS on Real-Time BCI Detection of Pedaling Motor Imagery. Sensors (Basel). 2018;18(4):1136. [72] ORTIZ M, IÁÑEZ E, GAXIOLA-TIRADO JA, et al. Study of the Functional Brain Connectivity and Lower-Limb Motor Imagery Performance After Transcranial Direct Current Stimulation. Int J Neural Syst. 2020; 30(8):2050038. [73] ZHANG H, JIAO L, YANG S, et al. Brain-computer interfaces: the innovative key to unlocking neurological conditions. Int J Surg. 2024; 110(9):5745-5762. [74] LO YT, LIM MJR, KOK CY, et al. Neural Interface-Based Motor Neuroprosthesis in Poststroke Upper Limb Neurorehabilitation: An Individual Patient Data Meta-analysis. Arch Phys Med Rehabil. 2024;105(12):2336-2349. [75] SAWAY BF, PALMER C, HUGHES C, et al. The evolution of neuromodulation for chronic stroke: From neuroplasticity mechanisms to brain-computer interfaces. Neurotherapeutics. 2024;21(3):e00337. |
| [1] | Wang Mi, Ma Shujie, Liu Yang, Qi Rui. Identification and validation of characterized gene NFE2L2 for ferroptosis in ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(7): 1466-1474. |
| [2] | Gao Yang, Qin Hewei, Liu Dandan. ACSL4 mediates ferroptosis and its potential role in atherosclerotic cardiovascular disease [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(6): 1239-1247. |
| [3] | Zhang Xiaoyu, Wei Shanwen, Fang Jiawei, Ni Li. Prussian blue nanoparticles restore mitochondrial function in nucleus pulposus cells through antioxidation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7318-7325. |
| [4] | Wang He, Yu Shaohong, . Meta-analysis of transcranial direct current stimulation in improving lower limb motor dysfunction in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6556-6565. |
| [5] | Ping Xingfeng, Huang Zongxuan, Li Kai, Xie Guangmin, Lyu Junying. Regularity of prescriptions for ischemic stroke based on latent structure combined with association rules [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6277-6284. |
| [6] | Wang Jiaru, Zhang Ying, Yang Yong, Qi Wen, Xiao Huaye, Ma Qiuping, Yang Lianzhao, Luo Ziwei, He Yaqing, Zhang Jiangyin, Wei Jiawen, Meng Yuan, Tan Silian. Systematic review of machine learning models for predicting functional recovery and prognosis in stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6317-6325. |
| [7] | Nan Songhua, Peng Chaojie, Cui Yinglin. Mitochondrial dysfunction and brain aging: a bibliometrics analysis based on the Web of Science Core Collection database [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(26): 5642-5651. |
| [8] | Wang Zhifeng, Yang Jiao, Xi Yujiang, Xu Shuangfeng, Shi Ting, Lan Junfeng, Hao Zhihui, He Pengfen, Yang Aiming, Pan Pan, Wang Jian. Biomarkers affecting the progression of mild to moderate cognitive impairment after stroke: #br# a non-targeted metabolomics analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5116-5126. |
| [9] | Cao Haijie, Song Huijie, Sun Yalu, Zhang Guangyou, Li Xiang. A wearable exoskeleton with posture feedback improves abnormal gait in patients with stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5127-5133. |
| [10] | Deng Yiran, Wang Xianliang, Li Dandan. Meta-analysis of exercise intervention on cardiopulmonary function in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5203-5211. |
| [11] | Hu Tong, Li Xuan, Yuan Jing, Wang Wei. Different electromagnetic stimulation programs improve post-stroke dysphagia: a network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5224-5236. |
| [12] | Lin Huijie, Huang Yun, Huang Zhihua, Jiang Lixia. Hot topics on exosomes as drug delivery system in central nervous system diseases [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(23): 5013-5021. |
| [13] | Yang Shuo, Zhang Zhen, Bai Shuo, Sheng Li, Shen Liang, Sun Qingfeng, Gao Beiyao, Ge Ruidong, Jiang Shan. Mitochondrial dysfunction in tendinopathy: possibility of mitochondria-targeting therapy [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(20): 4276-4285. |
| [14] | Zhang Qiming, Liao Di, Zhong Zhiliang, Lin Lihua, Zheng Xiang, Li Qiong, Shan Sharui. Effect of deep muscle stimulation combined with electromyographic biofeedback on the spasms of the triceps surae and gait changes after stroke [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(2): 385-392. |
| [15] | Wang Ruikun, Gao Weijuan, Zhang Haoran, Liu Yijie, Bu Jiaxin, Yuan Mei, Qin Yuxin, Zhang Yi. Effects of Buyang Huanwu Tang and its main components on pyroptosis in brain tissue of rats with middle cerebral artery occlusion and reperfusion [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(18): 3819-3825. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||