Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (31): 5007-5013.doi: 10.3969/j.issn.2095-4344.2017.31.015
Previous Articles Next Articles
Postoperative gait analysis of acute posterolateral rotatory dislocation of knee joint and its guiding significance
Huang Hua-qiang, Yun Zhu, Jiang Hai, Fu Wei-li, Li Jian, Tang Xin
- Department of Orthopedics, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China
-
Online:2017-11-08Published:2017-12-01 -
Contact:Tang Xin, M.D., Associate professor, Department of Orthopedics, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China -
About author:Huang Hua-qiang, M.D., Department of Orthopedics, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China
CLC Number:
Cite this article
Huang Hua-qiang, Yun Zhu, Jiang Hai, Fu Wei-li, Li Jian, Tang Xin. Postoperative gait analysis of acute posterolateral rotatory dislocation of knee joint and its guiding significance[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(31): 5007-5013.
share this article

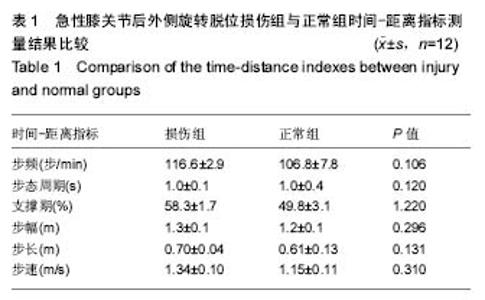
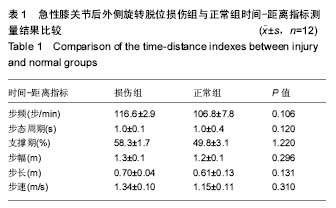
2.1 参与者数量分析 按意向性处理,纳入12例急性膝关节后外侧旋转脱位患者,将患者患侧膝关节作为损伤组,健侧膝关节作为正常组,全部进入结果,无脱落。试验流程图见图3。 2.2 随访结果 所有患者均获随访,随访时间为17-55个月。患者切口均Ⅰ期愈合,无切口感染、皮肤坏死及深静脉血栓等并发症;2例发生关节腔积液,经穿刺抽液等处理后好转;所有患者随访期无再脱位发生。末次随访时,患者后抽屉试验均为阴性,1例Lachman试验Ⅱ度阳性,1例外翻应力试验Ⅰ度阳性。 2.3 损伤组与正常组时间-距离指标测量结果 急性膝关节后外侧旋转脱位损伤组步频、步态周期、支撑期、步幅、步长、步速与正常组相比差异均无显著性意义(P > 0.05),见表1。"
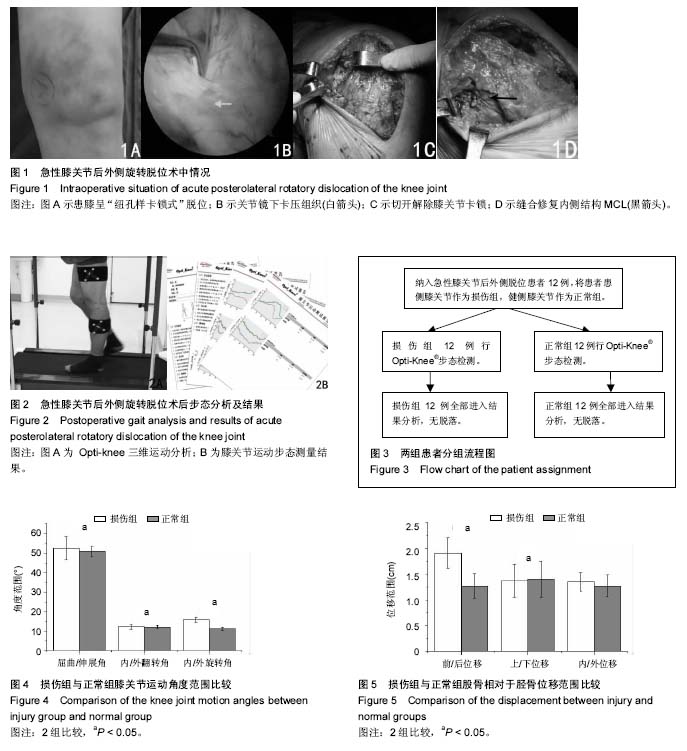
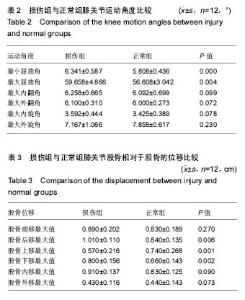
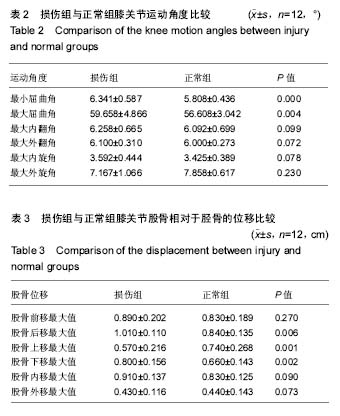
2.4 运动角度最大值、最小值及变化范围的比较 步行状态下,损伤组膝关节最小屈曲角、最大屈曲角大于正常组,而损伤组最大内/外翻角、内/外旋角与正常组相比,差异均无显著性意义(P > 0.05),见表2。 如图4示,步行状态下,损伤组膝关节屈曲/伸展角度范围[(52.483±6.027)° vs. (50.800±2.832)°,t=1.252,P=0.019]、内/外翻角度范围[(12.192±1.235)° vs. (12.092±0.808)°,t=0.355,P=0.034]及内/外旋转角度范围[(15.792±1.270)° vs. (11.283±0.823)°,t=18.418,P=0.005]均大于正常组。 2.5 位移最大值、最小值及运动范围的分析 步行状态下,损伤组膝关节股骨相对于胫骨后移、下移最大值大于正常组,上移最大值则有所减小(P < 0.05);而前移、内移和外移最大值2组相比,差异无显著性意义(P > 0.05),见表3。 如图5示,步行状态下,损伤组股骨相对于胫骨前/后移范围大于正常组[(1.910±0.300) cm vs. (1.270±0.241) cm,t=9.324,P=0.025],上/下位移小于正常组[(1.370± 0.320) cm vs. (1.400±0.346) cm,t=-0.758,P=0.000];比较2组内/外位移范围[(1.350±0.178) cm vs. (1.270± 0.211),t=1.350,P=0.102],差异无显著性意义。 "
| [1] Arom GA, Yeranosian MG, Petrigliano FA, et al. The changing demographics of knee dislocation: a retrospective database review. Clin Orthop Relat Res. 2014;472(9):2609-2614.[2] Benoit DL, Ramsey DK, Lamontagne M, et al. Effect of skin movement artifact on knee kinematics during gait and cutting motions measured in vivo. Gait Posture. 2006;24(2):152-164.[3] Schenck RC Jr, Richter DL, Wascher DC. Knee Dislocations:Lessons Learned From 20-Year Follow-up. Orthop J Sports Med. 2014;2(5): 232596711453487.[4] 何锐,杨柳,郭林,等. 急诊关节镜下清创复位联合二期韧带重建治疗急性膝关节后外侧旋转脱位[J]. 中国骨科临床与基础研究杂志, 2012, 4(2): 102-109.[5] Wascher DC. High-velocity knee dislocation with vascular injury.Treatment principles. Clin Sports Med. 2000;19(3): 457-477.[6] Howells NR, Brunton LR, Robinson J, et al. Acute knee dislocation: an evidence based approach to the management of the multiligament injured knee. Injury. 2011;42(11): 1198-1204.[7] Fanelli GC. Multiple ligament-injured (dislocated) knee. Sports Med Arthrosc. 2011;19(2): 81.[8] Capito N, Gregory MH, Volgas D, et al. Evaluation and management of an irreducible posterolateral knee dislocation. J Knee Surg. 2013;26(1): S136-S141.[9] Smyth MP , Koh JL. A review of surgical and nonsurgical outcomes of medial knee injuries. Sports Med Arthrosc. 2015; 23(2): e15-22.[10] Werner BC. Medial injury in knee dislocations: what are the common injury patterns and surgical outcomes? Clin Orthop Relat Res. 2014;472(9): 2658-2666. [11] 孙正宇,张承昊,唐新,等. 一期修复重建膝关节脱位多发韧带损伤的疗效观察[J]. 中国修复重建外科杂志, 2016, 30(6): 690-694.[12] 陈刚,付维力,唐新,等. 关节镜辅助治疗陈旧性膝关节后外侧旋转脱位[J]. 华西医学, 2016, 31(6): 1057-1061.[13] 张承昊, 李棋, 李箭. 华西膝关节脱位多发韧带损伤分期分型诊断及对治疗的指导意义的初步研究[A].中华医学会第十七届骨科学术会议暨第十届COA国际学术大会.重庆, 2015.[14] Howells NR, Brunton LR, Robinson J, et al. Acute knee dislocation: an evidence based approach to the management of the multiligament injured knee. Injury. 2011;42(11): 1198-1204.[15] Tibor LM. Management of medial-sided knee injuries. Part2: Posteromedial corner. Am J Sports Med. 2011;39(6): 1332-1340.[16] Levy BA, Dajani KA, Whelan DB, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25(4): 430-438.[17] 皇甫小桥,赵金忠,何耀华,等. 膝关节多发韧带损伤的修复与重建[J]. 中华骨科杂志, 2011, 31(2): 164-168.[18] Khakha RS, Day AC, Gibbs J, et al. Acute surgical management of traumatic knee dislocations - Average follow-up of 10years. Knee, 2015.[19] McKee L, Ibrahim MS, Lawrence T, et al. Current concepts in acute knee dislocation: the missed diagnosis? Open Orthop J. 2014;27(8): 162-167.[20] Polyzois VD, Stathopoulos IP, Benetos IS, et al. A Two-stage procedure for the treatment of a neglected posterolateral knee dislocation: Gradual reduction with an Ilizarov external fixator followed by arthroscopic anterior and posterior cruciate ligament reconstruction. Knee. 2016;23(1): 181-184.[21] Kohl S, Stock A, Ahmad SS, et al. Dynamic intraligamentary stabilization and primary repair: a new concept for the treatment of knee dislocation. Injury. 2015;46(4): 724-728.[22] Said HG, Learmonth DJ. Chronic irreducible posterolateral knee dislocation: two-stage surgical approach. Arthroscopy. 2007;23(5): e561-564.[23] Laprade RF, Wijdicks CA. The management of injuries to the medial side of the knee. J Orthop Sports Phys Ther. 2012; 42(3):221-233.[24] Fanelli GC, Edson CJ. Surgical treatment of combined PCL/ACL medial and lateral side injuries (global laxity): surgical technique and 2- to 18-year results. J Knee Surg. 2012;25: 307-316.[25] Georgoulis AD. Three-dimensional tibiofemoral kinematics ofthe anterior cruciate ligament-deficient and reconstructed knee during walking. Am J Sports Med. 2003;31(1): 75-79.[26] Hall M, Stevermer CA, Gillette JC. Gait analysis post anteriorcruciate ligament reconstruction: knee osteoarthritis perspective. Gait Posture. 2012;36(1): 56-60.[27] Takeda K, Hasegawa T, Kiriyama Y, et al. Kinematic motion of the anterior cruciate ligament deficient knee during functionally high and low demanding tasks. J Biomech. 2014;47(10): 2526-2530.[28] Polyzois VD, Stathopoulos IP, Benetos IS, et al. A Two-stage procedure for the treatment of a neglected posterolateral knee dislocation: Gradual reduction with an Ilizarov external fixator followed by arthroscopic anterior and posterior cruciate ligament reconstruction. Knee. 2016;23(1): 181-184.[29] 周敬滨,李国平,李方祥. 慢性膝关节前交叉韧带损伤患者步态的运动学分析[J]. 中国运动医学杂志, 2012, 31(10): 898-901, 912.[30] Brevetti C, De Caterina M, Martone VD, et al. Exercise increases soluble adhesion molecules ICAM-1 and VCAM-1 in patients with intermittent claudication. Clin Hemorheol Micorcirc. 2001;24(3): 193-199.[31] Wexler G, Hurwitz DE , Bush-Joseph CA, et al .Functional gait adaptations in patients with anterior cruciate ligament deficiency over time. Clin Orthop Relat Res. 1998;348 : 166-175.[32] 林泽枫,张余,马立敏,等. 外侧盘状半月板损伤患者膝关节在体运动学参数研究[J]. 中国骨科临床与基础研究杂志, 2014, 10(6): 291-296.[33] Barcellona MG, Morrissey MC, Milligan P, et al. The effect of thigh muscle activity on anterior knee laxity in the uninjured and anterior cruciate ligament-injured knee. Knee Surg Sports Traumatol Arthrosc. 2014;22(11): 2821-2829. [34] Griffith CJ, Wijdicks CA, LaPrade RF, et al. Force measurements on the posterior oblique ligament and superficial medial collateral ligament proximal and distal divisions to applied loads. Am J Sports Med. 2009;37: 140-148.[35] Leiter JR, Gourlay R, McRae S, et al. Long-term followup of ACL reconstruction with hamstring autograft. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1061-1069.[36] Lafortune MA, Cavanagh PR,Sommer HJ 3rd, et al. Three dimensional kinematics of the human knee during walking. J Biomech. 1992;25(4):347-357.[37] Snyder -Mackler L, Ladin Z, Schepsis AA, et al.Electrical stimulation of the thigh muscles after reconstruction of the anterior cruciate ligament .Effects of electrically elicited contraction of the quadriceps femoris and hamstring muscles on gaitand on strength of the thigh muscles. J Bone Joint Surg Am. 1991;73(7):1025-1036.[38] Timoney JM, Inman WS , Quesada PM, et al. Return of normal gait patterns after anterior cruciate ligament reconstruction.Am J Sports Med. 1993;21(6):887-889.[39] Houston ME, Goemans PH. Leg muscle performance of atheletes with and without brace. Arch Phys Med Rehabil. 1982;63 :431-436.[40] Branch T, Hunter R, Donath M. Dynamic EMG analysis of anterior cruciate deficient legs with and without bracing during cutting. Am J Sports Med. 1989;17:35-39.[41] Gao B, Cordova ML, Zheng NN. Three-dimensional joint kinematics of ACL-deficient and ACL-reconstructed knees during stair ascent and descent. Hum Mov Sci. 2012;31(1): 222-235. |
| [1] | Wang Jianping, Zhang Xiaohui, Yu Jinwei, Wei Shaoliang, Zhang Xinmin, Xu Xingxin, Qu Haijun. Application of knee joint motion analysis in machanism based on three-dimensional image registration and coordinate transformation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(在线): 1-5. |
| [2] | Zhuang Zhikun, Wu Rongkai, Lin Hanghui, Gong Zhibing, Zhang Qianjin, Wei Qiushi, Zhang Qingwen, Wu Zhaoke. Application of stable and enhanced lined hip joint system in total hip arthroplasty in elderly patients with femoral neck fractures complicated with hemiplegia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1429-1433. |
| [3] | Zhang Jichao, Dong Yuefu, Mou Zhifang, Zhang Zhen, Li Bingyan, Xu Xiangjun, Li Jiayi, Ren Meng, Dong Wanpeng. Finite element analysis of biomechanical changes in the osteoarthritis knee joint in different gait flexion angles [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1357-1361. |
| [4] | Bai Zixing, Cao Xuhan, Sun Chengyi, Yang Yanjun, Chen Si, Wen Jianmin, Lin Xinxiao, Sun Weidong. Construction and biomechanical analysis of ankle joint finite element model in gait cycle [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1362-1366. |
| [5] | Liu Feng, Feng Yi. Finite element analysis of different Kirschner wire tension bands on transverse patella fractures during gait cycle [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1367-1371. |
| [6] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [7] | Wu Bingshuang, Wang Zhi, Tang Yi, Tang Xiaoyu, Li Qi. Anterior cruciate ligament reconstruction: from enthesis to tendon-to-bone healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1293-1298. |
| [8] | Liu Gang, Ma Chao, Wang Le, Zeng Jie, Jiao Yong, Zhao Yi, Ren Jingpei, Hu Chuanyu, Xu Lin, Mu Xiaohong. Ankle-foot orthoses improve motor function of children with cerebral palsy: a Meta-analysis based on 12 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1299-1304. |
| [9] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [10] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [11] | Shao Yangyang, Zhang Junxia, Jiang Meijiao, Liu Zelong, Gao Kun, Yu Shuhan. Kinematics characteristics of lower limb joints of young men running wearing knee pads [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 832-837. |
| [12] | Zhou Jianguo, Liu Shiwei, Yuan Changhong, Bi Shengrong, Yang Guoping, Hu Weiquan, Liu Hui, Qian Rui. Total knee arthroplasty with posterior cruciate ligament retaining prosthesis in the treatment of knee osteoarthritis with knee valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 892-897. |
| [13] | Shan Sharui, Huang Xuming, Zhang Mingxing, Wang Xiukun, Zheng Xiang, Bao Sairong, Hong Feng. Three-dimensional gait analysis of low-frequency repetitive transcranial magnetic stimulation for post-stroke hemiplegia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 762-767. |
| [14] | Wei Xing, Liu Shufang, Mao Ning. Roles and values of blood flow restriction training in the rehabilitation of knee joint diseases [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 774-779. |
| [15] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||