Chinese Journal of Tissue Engineering Research ›› 2016, Vol. 20 ›› Issue (48): 7175-7184.doi: 10.3969/j.issn.2095-4344.2016.48.005
Previous Articles Next Articles
Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion for treating two-level contiguous cervical spondylotic myelopathy
Shen Qiang1, Ding Hao1, Zhu Zong-hao1, Zhu Liang1, Wei Xiao-kang1, He Xu-feng2
- 1Department of Orthopedic Surgery, Shanghai First People’s Hospital, Shanghai Jiao Tong University, Shanghai 200080, China; 2Department of Traumatology, Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 200025, China
-
Revised:2016-09-12Online:2016-11-25Published:2016-11-25 -
About author:Shen Qiang, M.D., Chief physician, Professor, Department of Orthopedic Surgery, Shanghai First People’s Hospital, Shanghai Jiao Tong University, Shanghai 200080, China -
Supported by:The Key Project for Medical Science from the Shanghai Committee of Science and Technology of China, No.12441900702
CLC Number:
Cite this article
Shen Qiang, Ding Hao, Zhu Zong-hao, Zhu Liang, Wei Xiao-kang, He Xu-feng. Anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion for treating two-level contiguous cervical spondylotic myelopathy[J]. Chinese Journal of Tissue Engineering Research, 2016, 20(48): 7175-7184.
share this article
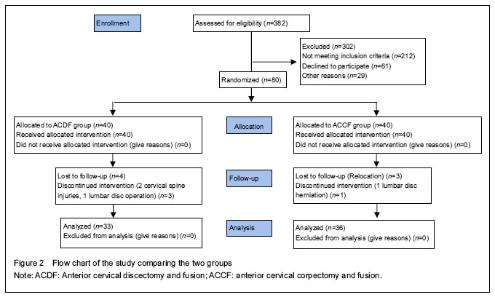
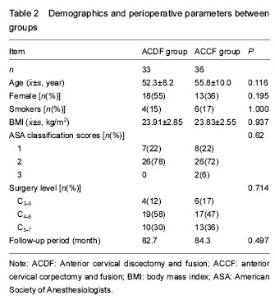
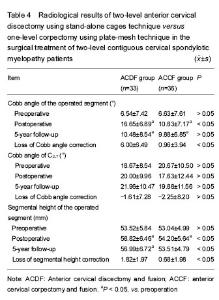
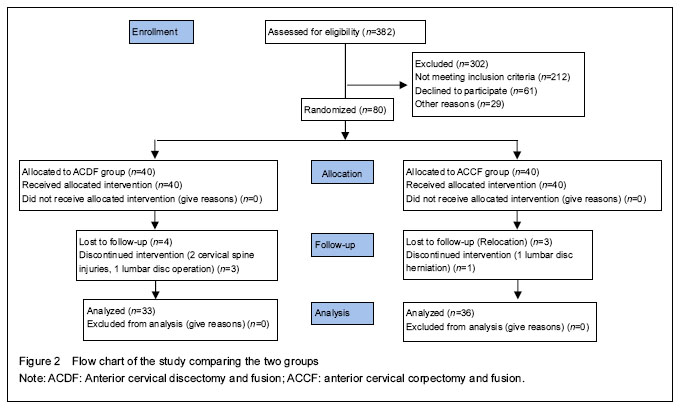
Quantitative analysis of participants The follow-up period of the patients ranged from 62 to 98 months (average 83.6). Of the original 80 patients, 11 (14%) withdrew from the study, and 7 were lost to follow-up (4 in ACDF group; 3 in ACCF group). Two of the patients in ACDF group withdrew from the study because of a cervical spine injury during follow-up, and another withdrew because of a lumbar disc disease operation during follow-up. In addition, one patient in the ACCF group withdrew because of lumbar disc herniation during follow-up. Of the remaining 69 patients (86%), 33 were in the ACDF group, and 36 were in the ACCF group. ACDF group comprised 15 men and 18 women with a mean age of 52.3 years (range: 37–67 years), whereas ACCF group comprised 23 men and 13 women with a mean age of 55.8 years (range: 25-71 years). The surgery levels involved were C3-5 in 10 cases, C4-6 in 36 cases, and C5-7 in 23 cases. Study flow chart is shown in Figure 2."
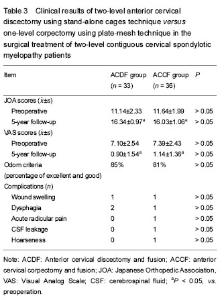
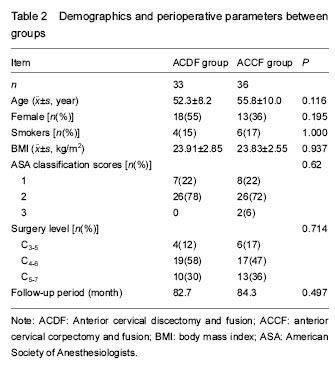
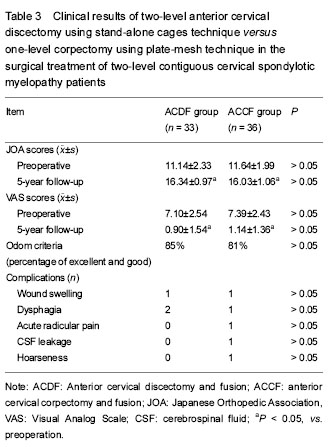
Clinical outcome The JOA scores significantly increased in the ACDF group and ACCF group (P < 0.01). The corresponding VAS scores significantly decreased in the ACDF group and ACCF group (P < 0.01). According to Odom’s criteria, the percentage of patients with excellent and good clinical outcomes was 85% in the ACDF group and 81% in the ACCF group. Although significant JOA scores and VAS scores improvement have been achieved in each group at the final follow-up, there were no significant differences between groups (P > 0.05; Table 3). Radiological analysis results The mean operated segmental Cobb angles at pre-, post-operation and 5-year follow-ups were 6.54, 16.65, and 10.48 degrees for ACDF group and 6.63, 10.83, and 9.88 degrees for ACCF group, respectively. There were significant differences in operated segmental Cobb angel between pre-operation and post-operation or 5-year follow-up in each group (P < 0.05). There was no significant difference in the operated segmental Cobb angle between these two groups at 5-year follow-up. The mean C2-7 Cobb angles at pre-, post-operation and 5-year follow-ups were 18.67, 20, and 21.96 degrees for ACDF group and 20.67, 17.63, and 19.88 degrees for ACCF group, respectively. There were no significant differences in C2-7 Cobb angel between pre-operation and post-operation or 5-year follow-up in each group. There was no significant difference in C2-7 Cobb angle between these two groups (Table 4). In the ACDF group, both post-operative and 5-year follow-up segmental height was significantly larger than pre-operative segmental height (P < 0.05); in the ACCF group, only post-operative segmental height was significantly larger than pre-operative segmental height (P < 0.05), not 5-year follow-up segmental height. At both post-operation and 5-year follow-up, segmental height of the ACDF group was significantly larger than that of ACCF group (P < 0.05). The loss of correction of segmental height in the ACDF group was significantly larger than that in the ACCF group at 5-year follow-up (P < 0.05; Table 4). The subsidence rates were 31% and 13% in the ACDF group and ACCF group, respectively. There was no significant difference between them. Solid fusion and bone union in the operated segments were observed in all patients at 5-year follow-up. No patient presented with instrumentation displacement. "
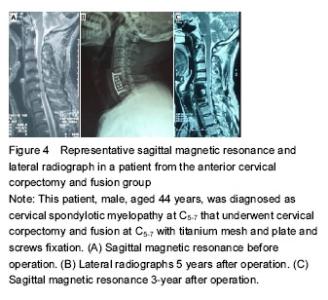
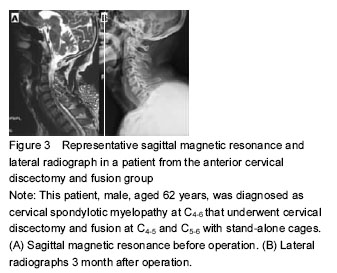
Case two: This patient, male, aged 44 years, was diagnosed as CSM at C5-7 that underwent cervical corpectomy and fusion at C5-7 with titanium mesh and plate and screw fixation (Figure 4). Adverse reactions There were some complications after the surgical treatment (Table 2). These complications were completely recovered within two months of after surgery."

| [1] Rao RD, Currier BL, Albert TJ, et al. Degenerative cervical spondylosis: clinical syndromes, pathogenesis, and management. J Bone Joint Surg Am. 2007;89(6):1360-1378.[2] Topuz K, Colak A, Kaya S, et al. Two-level contiguous cervical disc disease treated with peek cages packed with demineralized bone matrix: results of 3-year follow-up. Eur Spine J. 2009;18(2):238-243. [3] Chen Y, Wang X, Lu X, et al. Comparison of titanium and polyetheretherketone (PEEK) cages in the surgical treatment of multilevel cervical spondylotic myelopathy: a prospective, randomized, control study with over 7-year follow-up. Eur Spine J. 2013;22(7): 1539-1546. [4] Jang JW, Lee JK, Lee JH, et al. Effect of posterior subsidence on cervical alignment after anterior cervical corpectomy and reconstruction using titanium mesh cages in degenerative cervical disease. J Clin Neurosci. 2014;21(10):1779-1785. [5] 5. Song KJ, Lee KB, Song JH. Efficacy of multilevel anterior cervical discectomy and fusion versus corpectomy and fusion for multilevel cervical spondylotic myelopathy: a minimum 5-year follow-up study. Eur Spine J. 2012;21(8):1551-1557. [6] Oh MC, Zhang HY, Park JY, et al. Two-level anterior cervical discectomy versus one-level corpectomy in cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2009;34(7):692-696. [7] Mason RL, Gunst RF, Hess JL. Statistical Design and Analysis of Experiments: With Applications to Engineering and Science. 2nd ed. New Jersey: John Wiley and Sons, Inc. 2003:14-19.[8] Hacker RJ, Cauthen JC, Gilbert TJ, et al. A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine (Phila Pa 1976). 2000;25(20):2646-2654; discussion 2655.[9] Fessler RG, Steck JC, Giovanini MA. Anterior cervical corpectomy for cervical spondylotic myelopathy. Neurosurgery. 1998;43(2):257-265; discussion 265-267.[10] Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15(6): 602-617.[11] Matz PG, Pritchard PR, Hadley MN. Anterior cervical approach for the treatment of cervical myelopathy. Neurosurgery. 2007;60(1 Supp1 1):S64-70.[12] Cheng L, Nie L, Zhang L, et al. Fusion versus Bryan Cervical Disc in two-level cervical disc disease: a prospective, randomised study. Int Orthop. 2009; 33(5):1347-1351.[13] Kim SW, Limson MA, Kim SB, et al. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Eur Spine J. 2009;18(2):218-231. [14] Song KJ, Lee KB, Song JH. Efficacy of multilevel anterior cervical discectomy and fusion versus corpectomy and fusion for multilevel cervical spondylotic myelopathy: a minimum 5-year follow-up study. Eur Spine J. 2012;21(8):1551-1557.[15] Yang L, Gu Y, Liang L, et al. Stand-alone anchored spacer versus anterior plate for multilevel anterior cervical diskectomy and fusion. Orthopedics. 2012; 35(10):e1503-1510. [16] Bagby GW. Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopedics. 1988;11(6):931-934.[17] Cho DY, Liau WR, Lee WY, et al. Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery. 2002;51(6):1343-1349; discussion 1349-1350.[18] Cho DY, Lee WY, Sheu PC. Treatment of multilevel cervical fusion with cages. Surg Neurol. 2004;62(5):378-385, discussion 385-386.[19] Dufour T, Huppert J, Louis C, et al. Radiological analysis of 37 segments in cervical spine implanted with a peek stand-alone device, with at least one year follow-up. Br J Neurosurg. 2010;24(6):633-640.[20] Kolstad F, Nygaard ØP, Andresen H, et al. Anterior cervical arthrodesis using a "stand alone" cylindrical titanium cage: prospective analysis of radiographic parameters. Spine (Phila Pa 1976). 2010;35(16):1545-1550.[21] Ha SK, Park JY, Kim SH, et al. Radiologic Assessment of Subsidence in Stand-Alone Cervical Polyetheretherketone (PEEK) Cage. J Korean Neurosurg Soc. 2008;44(6):370-374.[22] Hwang SL, Hwang YF, Lieu AS, et al. Outcome analyses of interbody titanium cage fusion used in the anterior discectomy for cervical degenerative disc disease. J Spinal Disord Tech. 2005;18(4):326-331.[23] Uribe JS, Sangala JR, Duckworth EA, et al. Comparison between anterior cervical discectomy fusion and cervical corpectomy fusion using titanium cages for reconstruction: analysis of outcome and long-term follow-up. Eur Spine J. 2009;18(5):654-662. [24] Park Y, Maeda T, Cho W, et al. Comparison of anterior cervical fusion after two-level discectomy or single-level corpectomy: sagittal alignment, cervical lordosis, graft collapse, and adjacent-level ossification. Spine J. 2010;10(3):193-199. [25] Han YC, Liu ZQ, Wang SJ, et al. Is anterior cervical discectomy and fusion superior to corpectomy and fusion for treatment of multilevel cervical spondylotic myelopathy? A systemic review and meta-analysis. PLoS One. 2014;9(1):e87191. [26] Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J. 2007;16(9):1395-1400.[27] Schmieder K, Wolzik-Grossmann M, Pechlivanis I, et al. Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine. 2006;4(6):447-453.[28] Flynn TB. Neurologic complications of anterior cervical interbody fusion. Spine (Phila Pa 1976). 1982;7(6):536-539.[29] Apfelbaum RI, Kriskovich MD, Haller JR. On the incidence, cause, and prevention of recurrent laryngeal nerve palsies during anterior cervical spine surgery. Spine (Phila Pa 1976). 2000;25(22): 2906-2912.[30] Heeneman H. Vocal cord paralysis following approaches to the anterior cervical spine. Laryngoscope. 1973;83(1):17-21.[31] Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine (Phila Pa 1976). 2002;27(22):2453-2458.[32] Riley LH 3rd, Skolasky RL, Albert TJ, et al. Dysphagia after anterior cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study. Spine (Phila Pa 1976). 2005;30(22):2564-2569.[33] Hilibrand AS, Fye MA, Emery SE, et al. Increased rate of arthrodesis with strut grafting after multilevel anterior cervical decompression. Spine (Phila Pa 1976). 2002;27(2):146-151.[34] Wang JC, McDonough PW, Endow KK, et al. A comparison of fusion rates between single-level cervical corpectomy and two-level discectomy and fusion. J Spinal Disord. 2001;14(3):222-225. |
| [1] | Jiang Tao, Ma Lei, Li Zhiqiang, Shou Xi, Duan Mingjun, Wu Shuo, Ma Chuang, Wei Qin. Platelet-derived growth factor BB induces bone marrow mesenchymal stem cells to differentiate into vascular endothelial cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3937-3942. |
| [2] | Chen Yang, Huang Denggao, Gao Yuanhui, Wang Shunlan, Cao Hui, Zheng Linlin, He Haowei, Luo Siqin, Xiao Jingchuan, Zhang Yingai, Zhang Shufang. Low-intensity pulsed ultrasound promotes the proliferation and adhesion of human adipose-derived mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3949-3955. |
| [3] | Zhang Lishu, Liu Anqi, He Xiaoning, Jin Yan, Li Bei, Jin Fang. Alpl gene affects the therapeutic effect of bone marrow mesenchymal stem cells on ulcerative colitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3970-3975. |
| [4] | Ruan Guangping, Yao Xiang, Liu-Gao Miyang, Cai Xuemin, Li Zian, Pang Rongqing, Wang Jinxiang, Pan Xinghua. Umbilical cord mesenchymal stem cell transplantation for traumatic systemic inflammatory response syndrome in tree shrews [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3994-4000. |
| [5] | Mo Jianling, He Shaoru, Feng Bowen, Jian Minqiao, Zhang Xiaohui, Liu Caisheng, Liang Yijing, Liu Yumei, Chen Liang, Zhou Haiyu, Liu Yanhui. Forming prevascularized cell sheets and the expression of angiogenesis-related factors [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3479-3486. |
| [6] | Chen Lei, Zheng Rui, Jie Yongsheng, Qi Hui, Sun Lei, Shu Xiong. In vitro evaluation of adipose-derived stromal vascular fraction combined with osteochondral integrated scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3487-3492. |
| [7] | Wei Qin, Zhang Xue, Ma Lei, Li Zhiqiang, Shou Xi, Duan Mingjun, Wu Shuo, Jia Qiyu, Ma Chuang. Platelet-derived growth factor-BB induces the differentiation of rat bone marrow mesenchymal stem cells into osteoblasts [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 2953-2957. |
| [8] | Chen Xiao, Guo Zhi, Chen Lina, Liu Xuanyong, Zhang Yihuizhi, Li Xumian, Wang Yueqiao, Wei Liya, Xie Jing, Lin Li. Factors affecting the mobilization and collection of autologous peripheral blood hematopoietic stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 2958-2962. |
| [9] | Guo Zhibin, Wu Chunfang, Liu Zihong, Zhang Yuying, Chi Bojing, Wang Bao, Ma Chao, Zhang Guobin, Tian Faming. Simvastatin stimulates osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 2963-2968. |
| [10] | Li Congcong, Yao Nan, Huang Dane, Song Min, Peng Sha, Li Anan, Lu Chao, Liu Wengang. Identification and chondrogenic differentiation of human infrapatellar fat pad derived stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 2976-2981. |
| [11] | Gao Yuanhui, Xiang Yang, Cao Hui, Wang Shunlan, Zheng Linlin, He Haowei, Zhang Yingai, Zhang Shufang, Huang Denggao. Comparison of biological characteristics of adipose derived mesenchymal stem cells in Wuzhishan inbreed miniature pigs aged two different months [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 2988-2993. |
| [12] | Cao Yang, Zhang Junping, Peng Li, Ding Yi, Li Guanghui. Isolation and culture of rabbit aortic endothelial cells and biological characteristics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 3000-3003. |
| [13] | Dai Min, Wang Shuai, Zhang Nini, Huang Guilin, Yu Limei, Hu Xiaohua, Yi Jie, Yao Li, Zhang Ligang. Biological characteristics of hypoxic preconditioned human amniotic mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 3004-3008. |
| [14] | Qin Yanchun, Rong Zhen, Jiang Ruiyuan, Fu Bin, Hong Xiaohua, Mo Chunmei. Chinese medicine compound preparation inhibits proliferation of CD133+ liver cancer stem cells and the expression of stemness transcription factors [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 3016-3023. |
| [15] | Dai Yaling, Chen Lewen, He Xiaojun, Lin Huawei, Jia Weiwei, Chen Lidian, Tao Jing, Liu Weilin. Construction of miR-146b overexpression lentiviral vector and the effect on the proliferation of hippocampal neural stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(19): 3024-3030. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||