| [1] Fujimori T, Le H, Ziewacz JE, et al. Is there a difference in range of motion, neck pain, and outcomes in patients with ossification of posterior longitudinal ligament versus those with cervical spondylosis, treated with plated laminoplasty? Neurosurg Focus. 2013;35(1):E9.
[2] Kato M, Nakamura H, Konishi S, et al. Effect of preserving paraspinal muscles on postoperative axial pain in the selective cervical laminoplasty. Spine. 2008;33:E455-459.
[3] Hatta Y, Shiraishi T,Hase H, et al.Is posterior spinal cord shifting by extensive posterior decompression clinically significant for multisegmental cervical apondylotic myeloparhy? Spine. 2005;30(21):2414-2419.
[4] Luk KD,Kamath V, Avadhani A, et al. Cervical laminoplasty. Eur Spine J. 2010;19(2):347-348.
[5] Ratliff JK,Cooper PR. Cervical laminoplasty a critical review. Neurosurg(Spine 3). 2003;98:230-238.
[6] Sakaura H, Hosono N, Mukai Y, et al. C3-6 laminoplasty for cervical spondylotic myelopathy maintains satisfactory long-term surgical outcomes. Global Spine J. 2014;4(3): 169-174.
[7] Riew KD, Raich AL, Dettori JR,et al.Neck Pain Following Cervical Laminoplasty: Does Preservation of the C2 Muscle Attachments and/or C7 Matter? Evid Based Spine Care J. 2013;4(1):42-53.
[8] 王伟,任龙喜,高成杰,等.保留颈后方韧带复合体重建伸肌附着点单开门椎板成形术治疗颈椎疾患的临床观察[J].中国脊柱脊髓杂志,2008,18(4):253-256.
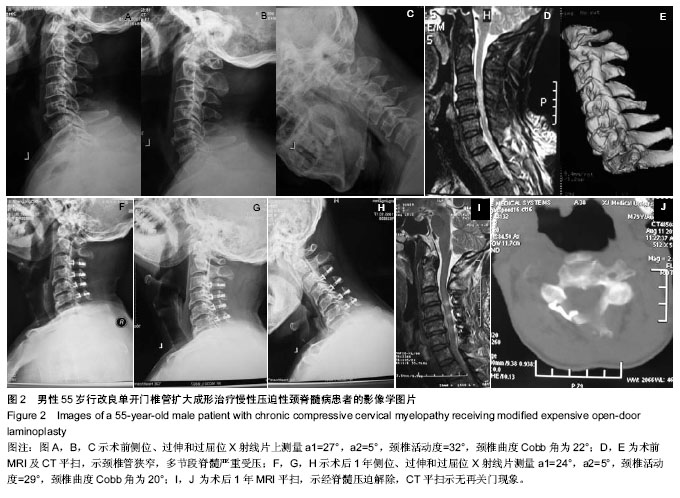
[9] 苏小桃,李平元,谭健,等.改良颈椎后路单开门椎管扩大成形术治疗多节段脊髓型颈椎病的效果评价[J].中外医学研究,2014, 12 (17):138-139.
[10] 孔凡磊,聂志红,刘中坡,等.改良颈椎后路单开门椎管扩大成形术治疗多节段脊髓型颈椎病[J].中国脊柱脊髓杂志,2013,23(1):16-19.
[11] Shiraishi T.A new technique for exposure of the cervical spine laminae.Technical note. J Neurosurg. 2002;96:122-126.
[12] Wang XY, Dai LY, Xu HZ, et al.Prediction of spinal canal expansion following cervical laminoplasty: a computer-simulated comparison between single and double-door techniques. Spine (Phila Pa 1976). 2006;31(24): 2863-2870.
[13] Hirabayashi K,Watanabe K,Wakano K,et al.Expansive open-door laminoplasty for cervical spinal tenotic elopathy. Spine.1983;8:693-699.
[14] Kawaguchitl Y,Matsui H,lshihara H,et al.Axial symptoms after en bloc cervical laminoplasty.J Spinal Disord.1999;12(5):392-395.
[15] Xie S, Sun T, Tian R, et al.Analysis of risk factors of axial symptoms after single door laminoplasty for cervical myelopathy. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014;28(5):620-624.
[16] 朱继超,刘晓光,刘忠军,等.术前颈椎曲度与椎管扩大成形术后脊髓后移程度及疗效的相关性[J].中国脊柱脊髓杂志,2013,23(7):587-593.
[17] Wu ZW, Ren SJ, Sheng XY, et al.Centerpiece plating in the cervical single open-door laminoplasty. Zhongguo Gu Shang. 2013;26(3):252-256.
[18] 李玉伟,王海蛟,严晓云,等. 颈椎单开门椎管扩大成形术不同椎板固定方法治疗多节段脊髓型颈椎病的疗效分析[J].中国脊柱脊髓杂志,2013,23(11):973-978.
[19] Della Pepa GM, Roselli R, La Rocca G, et al.Laminoplasty is better of laminectomy in cervical stenotic myelopathy: myth or truth? Eur Rev Med Pharmacol Sci. 2014;18(1 Suppl):50-54.
[20] Lee TT,Green BA,Gromelski EB,et al.Safety and stability of opendoor cervical extensive laminoplasty. J Spinal Disord. 1998;11(1):12-15.
[21] 张成程,林月秋,陈建明, 等.单开门椎管扩大成形术后保留颈后韧带复合体加微型钛板固定的生物力学[J].中国脊柱脊髓杂志,2011,21(1):59-61.
[22] Kotani Y, Abumi K, Ito M, et al.Minimum 2-year outcome of cervical laminoplasty with deep extensor muscle-preserving approach:impact on cervical spine function and quality of life. Eur Spine J. 2009;18:663-671.
[23] Kotani Y, Abumi K, Ito M, et al.Impact of deep extensor muscle-preserving approach on clinical outcome of laminoplasty for cervical spondylotic myelopathy: comparative cohort study. Eur Spine J. 2012;21(8):1536-1544.
[24] Schomacher J, Petzke F, Falla D,et al.Localised resistance selectively activates the semispinalis cervicis muscle in patients with neck pain. Man Ther. 2012;17(6):544-548. |