Chinese Journal of Tissue Engineering Research ›› 2014, Vol. 18 ›› Issue (43): 6889-6895.doi: 10.3969/j.issn.2095-4344.2014.43.001
Application of bone repair materials containing recombinant human bone morphogenetic protein-2 in anterior cervical discectomy and fusion
Xu Yun1, Jin Yao1, Shi Yong1, Jiang Wei-min2, Tang Tian-si2
- 1Department of Orthopaedics, Suzhou Xiangcheng People’s Hospital, Suzhou 215131, Jiangsu Province, China; 2Department of Orthopaedics, the First Affiliated Hospital of Suzhou University, Suzhou 215006, Jiangsu Province, China
-
Received:2014-09-13Online:2014-10-15Published:2014-10-15 -
Contact:Jiang Wei-min, Master’s supervisor, Chief physician, Department of Orthopaedics, the First Affiliated Hospital of Suzhou University, Suzhou 215006, Jiangsu Province, China -
About author:Xu Yun, Master, Attending physician, Department of Orthopaedics, Suzhou Xiangcheng People’s Hospital, Suzhou 215131, Jiangsu Province, China
CLC Number:
Cite this article
Xu Yun, Jin Yao, Shi Yong, Jiang Wei-min, Tang Tian-si. Application of bone repair materials containing recombinant human bone morphogenetic protein-2 in anterior cervical discectomy and fusion[J]. Chinese Journal of Tissue Engineering Research, 2014, 18(43): 6889-6895.
share this article
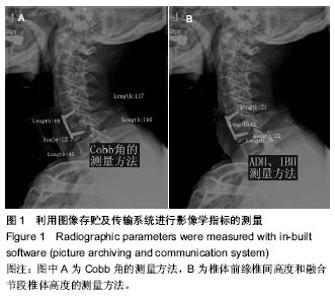
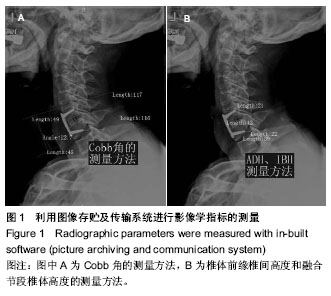
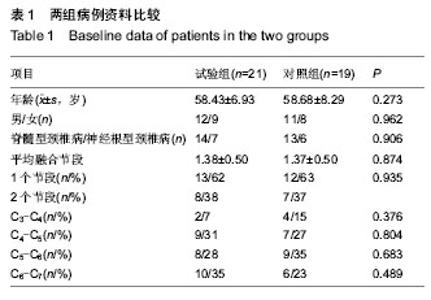
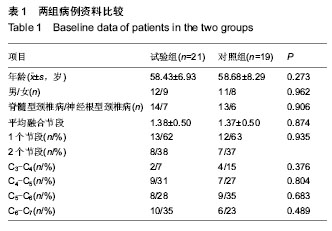
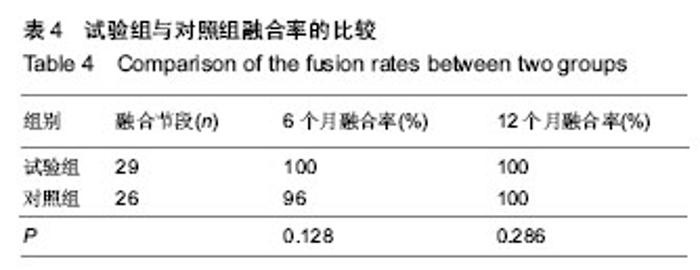
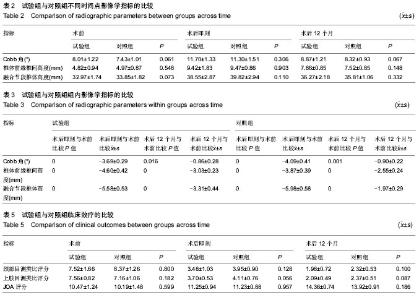
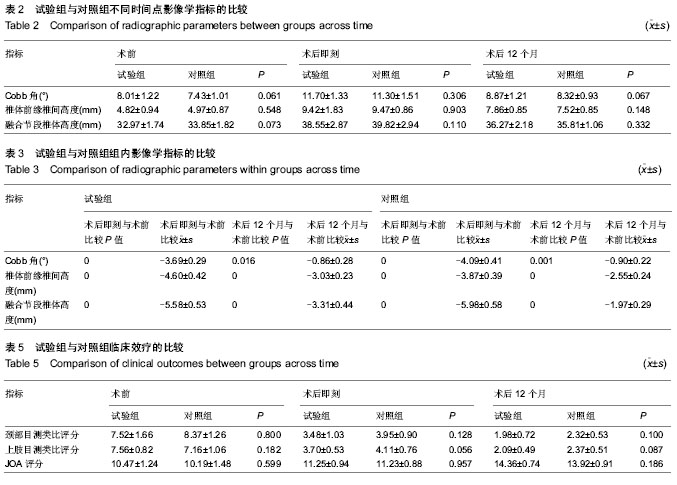
2.1 参与者数量分析 40例患者均完成12个月随访,进入结果分析。 2.2 基线资料比较 两组患者在年龄、性别、颈椎病类型、手术节段分布等方面比较差异均无显著性意义(P > 0.05),见表1。 2.3 术后影像学指标测量结果 6个月左右大部分病例获得满意的骨性融合,无假关节形成。 颈椎前凸(Cobb角)的变化:术前两组颈Cobb角比较差异无显著性意义(P=0.061)。术后两组Cobb角均较术前显著增加(P < 0.001)。随着随访时间的延长,两组颈椎前凸均有逐渐的丢失,末次随访时试验组Cobb角大于对照组(P=0.026),表明试验组对颈椎前凸的维持优于对照组;并且末次随访时,两组Cobb角仍然大于术前(P=0.016,P=0.001),见表2,3。 椎间高度的变化:术前两组融合节段椎间隙前缘高度比较差异无显著性意义(P=0.061)。术后两组前缘高度均较术前显著增加,两组间比较差异无显著性意义(P=0.903)。随着随访时间的延长,融合节段前缘高度逐渐丢失,至末次随访时,试验组融合节段前缘高度稍高于对照组,但差异无显著性意义(P=0.148)。融合节段高度的变化趋势与融合节段前缘高度大致相同,见表2,3。 融合率:试验组29个融合节段,对照组26个融合节段。随访6个月时,试验组融合率为100%,对照组融合率96%,至末次随访两组病例全部获得骨性融合,见表4。 2.4 两组临床疗效评价 术后两组患者颈部及上肢疼痛麻木症状及脊髓压迫受损JOA评分均有不同程度改善,见表5。 JOA评分:术前两组JOA评分比较差异无显著性意义(P=0.599)。术后24-48 h两组JOA评分较术前稍有改善,两组之间比较差异无显著性意义(P=0.957)。至末次随访时,两组JOA评分均有明显改善,两组之间比较差异无显著性意义(P=0.186)。 颈部目测类比评分:两组术前均有不同程度的颈部疼痛不适,两组术前目测类比评分差异无显著性意义(P=0.800)。术后24-48 h,两组目测类比评分均明显低于术前(P < 0.001),两组间比较差异无显著性意义(P=0.128)。至末次随访时,两组间比较差异无显著性意义(P=0.100)。 上肢目测类比评分:两组术前上肢疼痛麻木程度情况相当(P=0.182)。术后24-48 h,两组目测类比评分均较术前均有不同程度改善(P < 0.001)。末次随访时,两组间比较差异无显著性意义(P=0.087)。 2.5 手术情况及相关并发症 试验组与对照组手术时间分别为(107.76±18.24),(114.63±24.31) min,两组间比较差异无显著性意义(P=0.316)。试验组与对照组术中出血量分别为(122.86±53.02),(186.32±74.03) mL,组间差异有显著性意义(P=0.003)。试验组未发生严重的颈前软组织水肿,气道阻塞而致的呼吸困难。试验组有2例、对照组有3例出现一过性咽部不适或吞咽困难,但症状较轻,术后3 d后均自行缓解。两组各有1例术中发生硬脊膜破裂,以明胶海绵填塞、抬高床尾、减低颅内压、减少脑积液分泌药物治疗,均未出现严重的脑脊液漏。对照组有2例出现cage塌陷下沉,其中1例形成颈椎反曲,无脊髓及神经根受压症状,临床症状恢复好。试验组无cage下沉并发症出现。术后7个月随访X射线检查发现对照组有1例出现螺钉松动,但手术节段已牢固融合,"
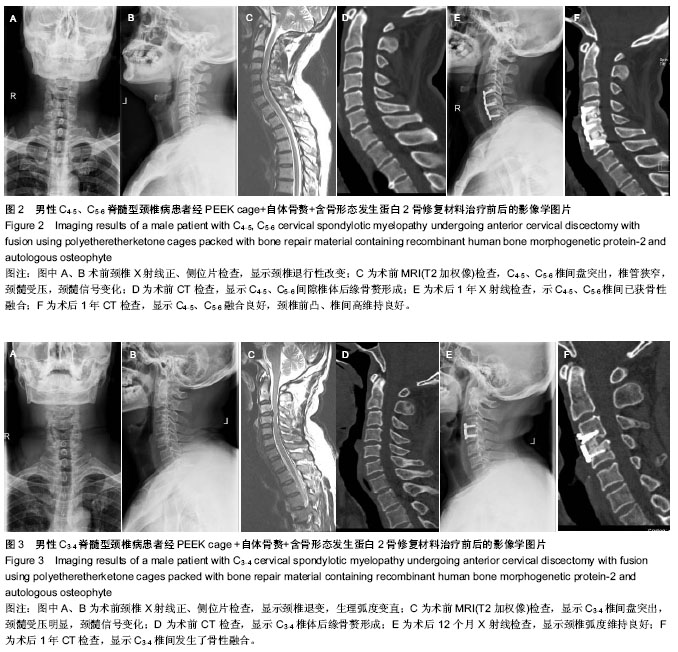
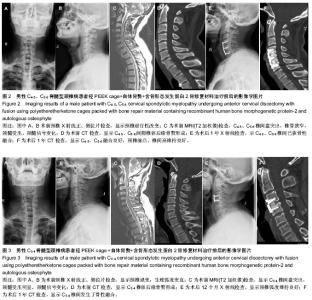
给予取出。对照组6例出现取骨处疼痛不适感(术后3个月后),取髂骨处发生浅表感染1例,经换药后治愈;另有髂前上棘骨折1例,麻木10例。 2.6 典型病例 病例1:49岁男性因“四肢麻木伴行走不稳1年”入院。术前依据颈椎正侧位片、CT及MRI,结合临床表现,诊断为脊髓型颈椎病,病变间隙为C4-5、C5-6,JOA评分8.5分。后行C4-6两个节段前路减压植骨融合,即PEEK cage+自体骨赘+骨优导,治疗前后影像学检查见图2。 病例2:46岁男性因“四肢乏力伴麻木2年”入院。术前依据颈椎正侧位片、CT及MRI,结合临床表现,诊断为脊髓型颈椎病,病变间隙为C3-4,JOA评分9.5分。后行C3-4前路减压植骨融合(PEEK cage+自体骨赘+骨优导),治疗前后影像学检查见图3。"
| [1] Smith GW,Robinson RA.The treatment of certain cervical- spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am.1958;40-A(3):607-624. [2] Cahill KS,Chi JH,Day A,et al.Prevalence, complications, and hospital charges associated with use of bone-morphogenetic proteins in spinal fusion procedures. JAMA. 2009;302(1): 58-66. [3] Smucker JD,Rhee JM,Singh K,et al.Increased swelling complications associated with off-label usage of rhBMP-2 in the anterior cervical spine.Spine (Phila Pa 1976).2006;31(24): 2813-2819. [4] Buttermann GR.Prospective nonrandomized comparison of an allograft with bone morphogenic protein versus an iliac-crest autograft in anterior cervical discectomy and fusion. Spine J.2008;8(3):426-435. [5] Vaidya R,Carp J,Sethi A,et al.Complications of anterior cervical discectomy and fusion using recombinant human bone morphogenetic protein-2.Eur Spine J.2007;16(8): 1257-1265. [6] Poynton AR,Lane JM.Safety profile for the clinical use of bone morphogenetic proteins in the spine.Spine (Phila Pa 1976). 2002;27(16 Suppl 1):S40-48. [7] McKay B,Sandhu HS.Use of recombinant human bone morphogenetic protein-2 in spinal fusion applications. Spine (Phila Pa 1976).2002;27(16 Suppl 1):S66-85. [8] Anderson DW,Burton DC,Jackson RS.Postoperative cervical myelopathy and cord compression associated with the use of recombinant bone morphogenetic protein-2 in posterior cervical decompression, instrumentation, and arthrodesis: a report of two cases.Spine (Phila Pa 1976).2011;36(10): E682-686. [9] Haid RW Jr,Branch CL Jr,Alexander JT,et al.Posterior lumbar interbody fusion using recombinant human bone morphogenetic protein type 2 with cylindrical interbody cages.Spine J.2004;4(5):527-538. [10] Vaccaro AR,Carrino JA,Venger BH,et al.Use of a bioabsorbable anterior cervical plate in the treatment of cervical degenerative and traumatic disc disruption. J Neurosurg.2002;97(4 Suppl):473-480. [11] Semantic D,Shen FH,Matthews DK,et al.Comparision of allograft to autograft in multilevel anterior cervical discectomy and fusion with rigid plate fixation. Spine (Phila Pa 1976). 2008; 3(2):451. [12] Baskin DS,Ryan P,Sonntag V,et al.A prospective, randomized, controlled cervical fusion study using recombinant human bone morphogenetic protein-2 with the CORNERSTONE-SR allograft ring and the ATLANTIS anterior cervical plate. Spine (Phila Pa 1976).2003;28(12):1219-1224. [13] Shields LB,Raque GH,Glassman SD,et al.Adverse effects associated with high-dose recombinant human bone morphogenetic protein-2 use in anterior cervical spine fusion.Spine (Phila Pa 1976).2006;31(5):542-547. [14] Boakye M,Mummaneni PV,Garrett M,et al.Anterior cervical discectomy and fusion involving a polyetheretherketone spacer and bone morphogenetic protein.J Neurosurg Spine. 2005;2(5):521-525. [15] Lanman TH,Hopkins TJ.Early findings in a pilot study of anterior cervical interbody fusion in which recombinant human bone morphogenetic protein-2 was used with poly (L-lactide-co-D,L-lactide) bioabsorbable implants.Neurosurg Focus. 2004;16(3):E6. [16] Tumialán LM,Pan J,Rodts GE,et al.The The safety and efficacy of anterior cervical discectomy and fusion with polyetheretherketone spacer and recombinant human bone morphogenetic protein-2: a review of 200 patients.J Neurosurg Spine. 2008;8(6):529-535. [17] Vaidya R,Carp J,Sethi A,et al.Complications of anterior cervical discectomy and fusion using recombinant human bone morphogenetic protein-2. Eur Spine J. 2007;16(8): 1257-1265. [18] Vaidya R,Weir R,Sethi A,et al.Interbody fusion with allograft and rhBMP-2 leads to consistent fusion but early subsidence.J Bone Joint Surg Br.2007;89(3):342-345. [19] Tumialán LM,Pan J,Rodts GE,et al.The safety and efficacy of anterior cervical discectomy and fusion with polyetheretherketone spacer and recombinant human bone morphogenetic protein-2: a review of 200 patients. J Neurosurg Spine.2008;8(6):529-535. [20] Frenkel MB,Cahill KS,Javahary RJ,et al.Fusion rates in multilevel, instrumented anterior cervical fusion for degenerative disease with and without the use of bone morphogenetic protein. J Neurosurg Spine.2013;18(3): 269-273. [21] Kandziora F,Bail H,Schmidmaier G,et a1.Bone morphogenetic protein-2 application by a poly(D,L-lactide)-coated interbody cage: in vivo results of a new carrier for growth factors.J Neurosurg.2002;97(1 Suppl):40-48. [22] Dickerman RD,Reynolds AS,Morgan BC,et al.rh-BMP-2 can be used safely in the cervical spine: dose and containment are the keys! Spine J. 2007;7(4):508-509. [23] Agrillo U,Mastronardi L,Puzzilli F.Anterior cervical fusion with carbon fiber cage containing coralline hydroxyapatite: preliminary observations in 45 consecutive cases of soft-disc herniation.J Neurosurg.2002;96(3 Suppl):273-276. [24] Chang WC,Tsou HK,Chen WS,et al.Preliminary comparison of radiolucent cages containing either autogenous cancellous bone or hydroxyapatite graft in multilevel cervical fusion.J Clin Neurosci.2009;16(6):793-796. [25] Niu CC,Liao JC,Chen WJ,et al.Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion: titanium cages versus polyetheretherketone (PEEK) cages.J Spinal Disord Tech.2010;23(5):310-316. [26] Cho DY,Liau WR,Lee WY,et al.Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease.Neurosurgery.2002;51(6):1343-1349. [27] Topuz K,Colak A,Kaya S,et al.Two-level contiguous cervical disc disease treated with peek cages packed with demineralized bone matrix: results of 3-year follow-up.Eur Spine J.2009;18(2):238-243. |
| [1] | Tang Xiaokai, Li Weiming. Role and mechanism of Nel-like molecule-1 in promoting bone fusion after spinal fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3914-3920. |
| [2] | Chen Jiang, Li Jinyu, Zheng Chenying, Bai Chunxiao, Zhang Fan, Liu Chuyin, Zhao Xueqian, Yuan Qiaomei, Di Xueshi, Kang Shengqian, Jia Yusong . Changes in sagittal parameters of cervical spine after double-segment artificial cervical disc replacement and anterior cervical discectomy and fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2341-2346. |
| [3] | Cao Liangliang, Xu Jianguang, Mei Wei. Three-dimensional finite element analysis of the biomechanical changes of the lumbar spine after the combination of intervertebral fusion with dynamic internal fixation of the interspinous process in the lumbosacral region [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(12): 1905-1910. |
| [4] | Wang Liang, Li Lijun, Zhu Fuliang, Jiang Zhuyan, Wang Shuai, Ni Dongkui . Cortical bone trajectory screw versus pedicle screw fixation after posterior lumbar interbody fusion: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(8): 1291-1298. |
| [5] | Liang Long, Wei Xu, Zhu Liguo, Yin He, Yu Jie, Feng Minshan, Chen Lin. Cervical posterior single-door laminoplasty versus double-door laminoplasty for cervical spondylotic myelopathy: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(8): 1299-1306. |
| [6] | Wang Xuefeng, Shang Xifu . Curative effects of three filling materials in the treatment of osteoporotic thoracolumbar fractures [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(6): 863-869. |
| [7] | Li Qingsong, Liu Shaoyu, Yin Zongsheng. Multiple posterior lumbar interbody fusion and posterolateral fusion instrumentation for thoracolumbar kyphosis and osteoporotic fracture in older adults [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(4): 512-517. |
| [8] | Tang Xianneng, Chen Yueping, Zhang Xiaoyun. Clinical application of bone morphogenetic proteins in bone and cartilage tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(4): 591-596. |
| [9] | Liu Junyin, Feng Wei, Xie Yingchun, Li Yuwan, Zeng Jitao, Liu Ziming, Tu Xiaolin. Bone morphologic protein signaling pathway in bone regeneration and repair: accurate regulation and treatment targets [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(4): 606-612. |
| [10] | Li Xianzhou, Wang Qian, Zhang Cunxin . Lumbar spondylolisthesis: status and prospects of implant treatment [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(4): 621-627. |
| [11] | Liu Shuzhong1, Lao Lifeng2. Effects of recombinant human bone morphogenetic protein-2 on the proliferation of breast cancer MCF-7 cells [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(3): 458-463. |
| [12] | Yi Guoliang, Wang Shankun, Song Xizheng. Biomechanical testing of the locking axial lumbosacral interbody fusion [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(28): 4546-4551. |
| [13] | Lu Yanqin, Yi Fang, Ju Wei, Li Wenjie, Lei Lei. Reparation of femoral defects with a Ca-P coated magnesium alloy scaffold carrying sustained release microspheres [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(2): 232-238. |
| [14] | Zhang Xiang1, Qian Yuzhang1, Xie Lin2, 3, Kang Ran2, 3 . Technological methods and result evaluation of establishing the animal models of vertebral artery type of cervical spondylosis [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(15): 2427-2435. |
| [15] | Li Haoliang, Wang Xibin, Zuo Ruiting. Calcium phosphate cement/fibrin glue composite loaded with recombinant human bone morphogenetic protein 2 promotes osteoporotic fracture healing [J]. Chinese Journal of Tissue Engineering Research, 2019, 23(14): 2156-2161. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||