Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (28): 4479-4484.doi: 10.3969/j.issn.2095-4344.1469
Previous Articles Next Articles
Short-segment percutaneous pedicle screw instrumentation for the treatment of thoracolumbar fractures: bilateral fracture level and cross-fracture level
- Department of Orthopedics, First Affiliated Hospital, Soochow University, Suzhou 215006, Jiangsu Province, China
-
Online:2019-10-08Published:2019-10-08 -
Contact:Ni Li, Doctoral candidate, Assistant researcher, Department of Orthopedics, First Affiliated Hospital, Soochow University, Suzhou 215006, Jiangsu Province, China Wu Guizhong, Master, Attending surgeon, Department of Orthopedics, First Affiliated Hospital, Soochow University, Suzhou 215006, Jiangsu Province, China -
About author:Wang Jinning, Department of Orthopedics, First Affiliated Hospital, Soochow University, Suzhou 215006, Jiangsu Province, China
CLC Number:
Cite this article
Wang Jinning, Song Dawei, Qiao Yusen, Yang Yan, Zou Jun, Zhang Linlin, Geng Dechun, Yang Huilin, Wu Guizhong, Ni Li.
share this article
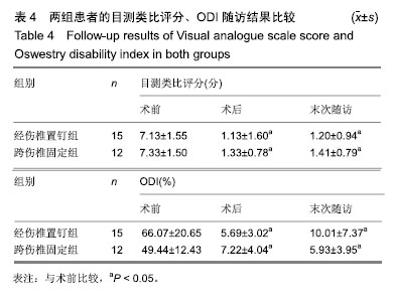
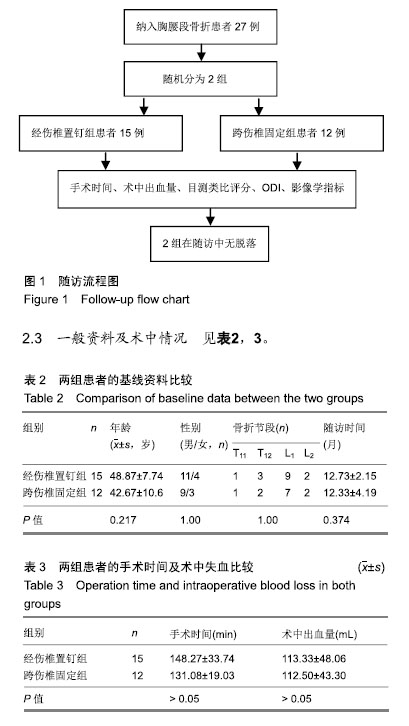
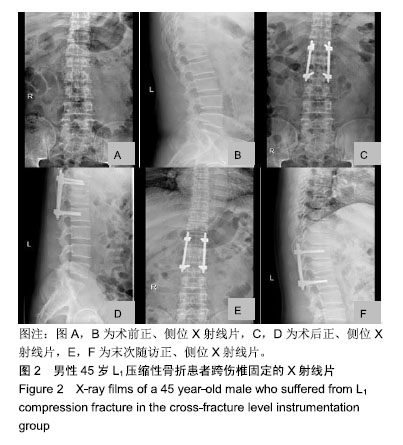
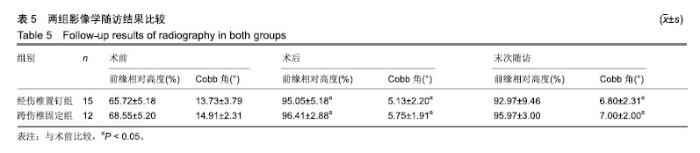
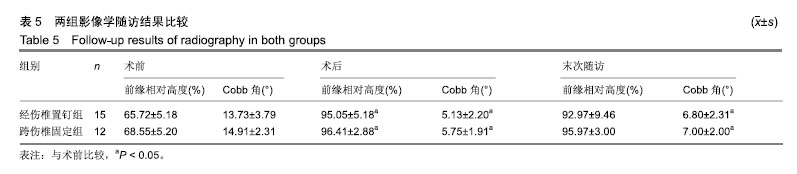
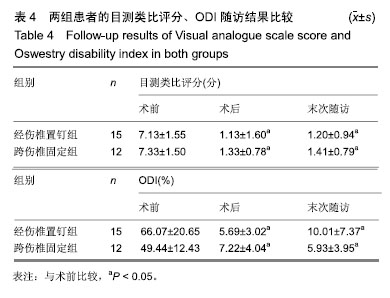
2组患者的基线资料比较差异无显著性意义(P > 0.05),具有可比性。2组患者的手术时间、术中出血量比较差异均无显著性意义(P > 0.05)。经伤椎置钉组随访时间为8-20个月,平均(12.73±2.15)个月;跨伤椎置钉组随访时间为5-17个月,平均(12.33±4.19)个月。 2.4 目测类比评分及ODI 所有患者均顺利完成手术,2组患者术后症状改善明显,术后及末次随访的目测类比评分及ODI见表4。2组患者目测类比评分、ODI较术前好转,经统计差异存在显著性意义(P < 0.05);术后和末次随访的目测类比评分及ODI差异无显著性意义(P > 0.05)。同一时间点2组的目测类比评分、ODI差异无显著性意义(P > 0.05)。"
| [1]Khare S, Sharma V. Surgical outcome of posterior short segment trans-pedicle screw fixation for thoracolumbar fractures. J Orthop. 2013;10(4)162-167.[2]Rajasekaran S, Kanna RM, Shetty AP. Management of thoracolumbar spine trauma: An overview. Indian J Orthop. 2015;49(1):72-82.[3]王圣杰,夏天,柳超,等. 经皮椎弓根螺钉棒无融合内固定治疗胸腰椎骨折[J]. 中国矫形外科杂志,2018,26(4):294-298.[4]Reinhold M, Knop C, Beisse R,et al. Operative treatment of 733 patients with acute thoracolumbar spinal injuries: comprehensive results from the second, prospective, internet-based multicenter study of the spine study group of the german association of trauma surgery. Eur Spine J. 2010; 19(10):1657-1676.[5]Alander DH, Cui S. Percutaneous pedicle screw stabilization: surgical technique, fracture reduction, and review of current spine trauma applications. J Am Acad Orthop Surg. 2018; 26(7):231-240.[6]Phan K, Rao PJ, Mobbs RJ. Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures: Systematic review and meta-analysis of comparative studies. Clin Neurol Neurosurg. 2015;135:85-92.[7]Scheer JK, Bakhsheshian J, Fakurnejad S, et al. Evidence-based medicine of traumatic thoracolumbar burst fractures: a systematic review of operative management across 20 years. Global Spine J. 2015;5(1):73-82.[8]Gejo R, Matsui H, Kawaguchi Y, et al. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine. 1999;24(10):1023-1028.[9]Magerl FP. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res. 1984(189):125-141.[10]Fogel GR, Reitman CA, Liu W, et al. Physical characteristics of polyaxial-headed pedicle screws and biomechanical comparison of load with their failure. Spine. 2003;28(5): 470-473.[11]Fan S, Hu Z, Zhao F, et al. Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. Eur Spine J. 2010;19(2):316-324.[12]Kim DY, Lee SH, Chung SK, et al. Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine. 2005;30(1):123-129.[13]Rodriguez-Vela J, Lobo-Escolar A, Joven-Aliaga E, et al. Perioperative and short-term advantages of mini-open approach for lumbar spinal fusion. Eur Spine J. 2009;18(8): 1194-1201.[14]Schmidt OI, Strasser S, Kaufmann V, et al. Role of early minimal-invasive spine fixation in acute thoracic and lumbar spine trauma. Indian J Orthop. 2007;41(4):374-380.[15]Zhao Q, Zhang H, Hao D, et al. Complications of percutaneous pedicle screw fixation in treating thoracolumbar and lumbar fracture. Medicine (Baltimore). 2018;97(29): e11560.[16]Gayet LE, Pries P, Hamcha H, et al. Biomechanical study and digital modeling of traction resistance in posterior thoracic implants.Spine.2002;27(7):707-714.[17]Liljenqvist U, Hackenberg L, Link T, et al. Pullout strength of pedicle screws versus pedicle and laminar hooks in the thoracic spine. Acta orthopaedica Belgica. 2001;67(2): 157-163.[18]Regev GJ, Lee YP, Taylor WR, et al. Nerve injury to the posterior rami medial branch during the insertion of pedicle screws: comparison of mini-open versus percutaneous pedicle screw insertion techniques. Spine. 2009;34(11): 1239-1242.[19]Koreckij T, Park DK, Fischgrund J. Minimally invasive spine surgery in the treatment of thoracolumbar and lumbar spine trauma. Neurosurg Focus. 2014;37(1):E11.[20]Liao JC, Fan KF, Keorochana G, et al. Transpedicular grafting after short-segment pedicle instrumentation for thoracolumbar burst fracture: calcium sulfate cement versus autogenous iliac bone graft. Spine. 2010;35(15):1482-1488.[21]Lehmann W, Ushmaev A, Ruecker A, et al. Comparison of open versus percutaneous pedicle screw insertion in a sheep model. Eur Spine J. 2008;17(6):857-863.[22]Hussain NS, Perez-Cruet MJ. Complication management with minimally invasive spine procedures. Neurosurg Focus. 2011; 31(4):E2.[23]Lee KH, Yue WM, Yeo W, et al. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. 2012;21(11):2265-2270.[24]Anekstein Y, Brosh T, Mirovsky Y. Intermediate screws in short segment pedicular fixation for thoracic and lumbar fractures: a biomechanical study. J Spinal Disord Tech. 2007; 20(1):72-77.[25]Baaj AA, Reyes PM, Yaqoobi AS, et al. Biomechanical advantage of the index-level pedicle screw in unstable thoracolumbar junction fractures. J Neurosurg Spine. 2011; 14(2):192-197.[26]Gelb D, Ludwig S, Karp JE, et al. Successful treatment of thoracolumbar fractures with short-segment pedicle instrumentation. J Spinal Disord Tech. 2010;23(5):293-301.[27]Tian JW, Wang L, Xia T, et al. Posterior short-segmental fixation combined with intermediate screws vs conventional intersegmental fixation for monosegmental thoracolumbar fractures. Orthopedics. 2011;34(8):e389-396.[28]Raley DA, Mobbs RJ. Retrospective computed tomography scan analysis of percutaneously inserted pedicle screws for posterior transpedicular stabilization of the thoracic and lumbar spine: accuracy and complication rates. Spine. 2012; 37(12):1092-1100.[29]Seng C, Tow BP, Siddiqui MA, et al. Surgically treated cervical myelopathy: a functional outcome comparison study between multilevel anterior cervical decompression fusion with instrumentation and posterior laminoplasty. Spine J. 2013; 13(7):723-731.[30]Fitschen-Oestern S, Scheuerlein F, Weuster M, et al. Reduction and retention of thoracolumbar fractures by minimally invasive stabilisation versus open posterior instrumentation. Injury. 2015;46 Suppl 4:S63-70. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||