Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (21): 3349-3356.doi: 10.3969/j.issn.2095-4344.0881
Previous Articles Next Articles
Transplantation of neural stem cells from different sources in the treatment of cerebral ischemia injury in rats
Zhong Bo1, Liu Xia2, Wu Wei3
- 1Department of Neurology, 2Department of Electrocardiogram, Linqing People’s Hospital, Linqing 252600, Shandong Province, China; 3Department of Neurology, Qilu Hospital of Shandong University, Jinan 250012, Shandong Province, China
-
Revised:2017-02-26Online:2018-07-28Published:2018-07-28 -
About author:Zhong Bo, Associate chief physician, Department of Neurology, Linqing People’s Hospital, Linqing 252600, Shandong Province, China
CLC Number:
Cite this article
Zhong Bo, Liu Xia, Wu Wei . Transplantation of neural stem cells from different sources in the treatment of cerebral ischemia injury in rats[J]. Chinese Journal of Tissue Engineering Research, 2018, 22(21): 3349-3356.
share this article

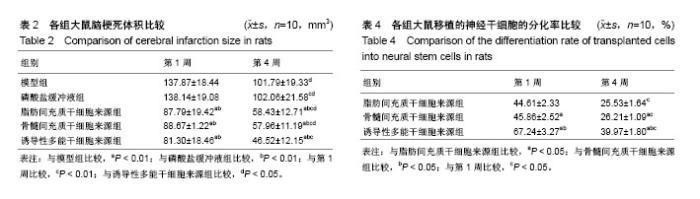
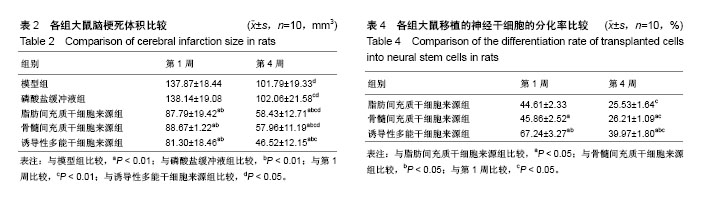
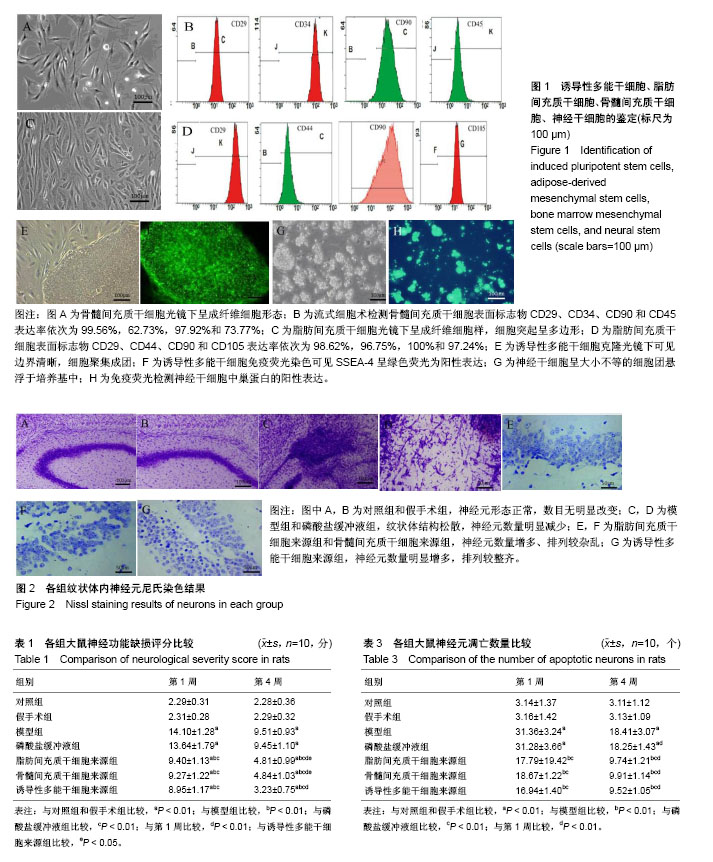
2.1 诱导性多能干细胞、脂肪间充质干细胞、骨髓间充质干细胞、神经干细胞的鉴定 倒置相差显微镜下,传代脂肪间充质干细胞和骨髓间充质干细胞呈典型的成纤维细胞样形态,多边形,轮廓清晰,骨髓间充质干细胞表面标志物CD29、CD34、CD90和CD45表达率依次为99.56%,62.73%,97.92%,73.77%,脂肪间充质干细胞表面标志物CD29、CD44、CD90和CD105表达率依次为98.62%,96.75%,100%和97.24%;诱导性多能干细胞克隆光镜下可见边界清晰,细胞聚集成团,免疫荧光染色细胞中SSEA-4呈绿色荧光为阳性表达;传代神经干细胞呈大小不等的细胞团悬浮于培养基中,免疫荧光染色细胞中巢蛋白呈绿色荧光为阳性表达,见图1。 2.2 不同来源神经干细胞的转化率比较 诱导分化7 d后,诱导性多能干细胞来源的神经干细胞的转化率为(89.46±2.63)%,明显高于脂肪间充质干细胞来源(65.32± 3.77)%和骨髓间充质干细胞来源(67.28±4.51)%,差异有显著性意义(P < 0.01),脂肪间充质干细胞来源的神经干细胞的转化率与骨髓间充质干细胞来源差异无显著性意义(P > 0.05)。 2.3 实验动物数量分析 用于研究的SD大鼠共150只,随机选取110只进行脑缺血模型建立,其中10只SD大鼠造模不理想予以剔除,将100只造模成功的SD大鼠随机分为5组进行后续实验,每组20只;另将剩余40只SD大鼠随机分为对照组和假手术组,每组20只;最终140只SD大鼠的研究数据进入结果分析,实验过程顺利,无中途脱落。 2.4 各组大鼠神经功能缺损评分比较 移植1周和4周后,脂肪间充质干细胞来源组、骨髓间充质干细胞来源组、诱导性多能干细胞来源组、模型组和磷酸盐缓冲液组大鼠的神经功能缺损评分均明显高于对照组和假手术组(P < 0.01);模型组和磷酸盐缓冲液组大鼠的神经功能缺损评分均明显高于脂肪间充质干细胞来源组、骨髓间充质干细胞来源组和诱导性多能干细胞来源组(P < 0.01);移植4周时脂肪间充质干细胞来源组、骨髓间充质干细胞来源组、诱导性多能干细胞来源组和磷酸盐缓冲液组大鼠的神经功能缺损评分均明显低于移植1周(P < 0.01);移植4周后,诱导性多能干细胞来源组神经功能缺损评分明显低于脂肪间充质干细胞来源组和骨髓间充质干细胞来源组(P < 0.05),见表1。 2.5 各组大鼠脑梗死体积比较 移植1周和4周后,脂肪间充质干细胞来源组、骨髓间充质干细胞来源组和诱导性多能干细胞来源组的大鼠脑梗死体积明显小于磷酸盐缓冲液组和模型组(P < 0.01);移植4周时,脂肪间充质干细胞来源组、骨髓间充质干细胞来源组、诱导性多能干细胞来源组、模型组和磷酸盐缓冲液组大鼠脑梗死体积明显低于移植1周(P < 0.01);移植4周时,诱导性多能干细胞来源组的大鼠脑梗死体积明显低于脂肪间充质干细胞来源组、骨髓间充质干细胞来源组(P < 0.01),见表2。 2.6 各组大鼠神经元凋亡数量比较 移植1周和4周后,脂肪间充质干细胞来源组、骨髓间充质干细胞来源组和诱导性多能干细胞来源组的大鼠神经元凋亡数量明显小于磷酸盐缓冲液组和模型组(P < 0.01);移植4周时,脂肪间充质干细胞来源组、骨髓间充质干细胞来源组、诱导性多能干细胞来源组、模型组和磷酸盐缓冲液组大鼠神经元凋亡数量明显低于移植1周(P < 0.01),见表3。 2.7 各组大鼠神经元丢失情况比较 尼氏染色显示,对照组纹状体的神经元形态正常,尼氏体呈蓝紫色斑块或颗粒状,分布均匀;假手术组纹状体的神经元形态正常,数目无明显改变,尼氏体分布正常;模型组、磷酸盐缓冲液组纹状体构松散、神经元排列紊乱、神经元数量明显减少;脂肪间充质干细胞来源组和骨髓间充质干细胞来源组神经元数量增多,聚集成团;诱导性多能干细胞来源组神经元数量明显增多,排列较整齐,见图2。 2.8 各组大鼠移植的神经干细胞分化率比较 移植1周和4周后,诱导性多能干细胞来源组高于脂肪间充质干细胞来源组、骨髓间充质干细胞来源组(P < 0.01);移植4周时,脂肪间充质干细胞来源组、骨髓间充质干细胞来源组、诱导性多能干细胞来源组大鼠神经干细胞分化率均明显低于移植1周(P < 0.05),见表4。"
| [1] 王晓平,倪京满. 脑缺血再灌注损伤的研究及药物治疗进展[J]. 中国新药杂志,2016,25(6):659-663.[2] 刘婕,张国华.脐血干细胞治疗脑卒中的作用与机制[J].中国组织工程研究,2017,21(9):1472-1476.[3] Andreopoulou E, Arampatzis A, Patsoni M, et al. Being a Neural Stem Cell: A Matter of Character But Defined by the Microenvironment. Adv Exp Med Biol. 2017;1041:81-118.[4] 刘一民,赵艳艳,陈红兵. 神经干细胞移植脑缺血模型大鼠神经细胞凋亡、分化及神经行为学的变化[J].中国组织工程研究, 2017,21(13):2029-2035.[5] Augestad IL, Nyman AKG, Costa AI, et al. Effects of Neural Stem Cell and Olfactory Ensheathing Cell Co-transplants on Tissue Remodelling After Transient Focal Cerebral Ischemia in the Adult Rat. Neurochem Res. 2017;42(6):1599-1609.[6] 钱晓丹,罗春霞,朱东亚.神经干细胞移植研究进展[J].中国细胞生物学学报,2012,34(3):212-217.[7] 李峰,蔡光先.脑缺血后神经再生及其治疗的研究进展[J].中华中医药杂志,2016,31(2):578-581.[8] 曲艺,孙正巍,杨东波,等. 神经干细胞移植治疗大鼠局灶性脑缺血损伤[J].中国组织工程研究,2013,17(10):1876-1883.[9] 冯年花,谢安,娄远蕾,等.人诱导性多能干细胞定向分化为神经干细胞的实验研究[J].基础医学与临床, 2010,30(12):1263-1267.[10] 魏雁,陈刚.神经干细胞工程化的研究进展[J].中国组织工程研究, 2009,13(6):1159-1162.[11] Ryu S, Lee SH, Kim SU, et al. Human neural stem cells promote proliferation of endogenous neural stem cells and enhance angiogenesis in ischemic rat brain. Neural Regen Res. 2016;11(2):298-304.[12] Watanabe T, Nagai A, Sheikh AM, et al. A human neural stem cell line provides neuroprotection and improves neurological performance by early intervention of neuroinflammatory system. Brain Res. 2016;1631:194-203.[13] 蒲晓姝,果磊,张敏珠,等.大鼠骨髓间充质干细胞的培养鉴定以及向神经干细胞分化的实验研究[J].重庆医科大学学报, 2013, 38(3):235-239.[14] 曲泽澎,管圆,崔璐,等.大鼠诱导性多能干细胞向神经前体细胞诱导分化研究[J].同济大学学报:医学版, 2013,34(3):1-6,11.[15] 陈旭东,范文娟,袁科理,等.不同培养条件对小鼠诱导性多能干细胞分化为神经元样细胞的影响[J].细胞与分子免疫学杂志, 2015, 31(9):1216-1223.[16] An J, Yan H, Li X, et al. The inhibiting effect of neural stem cells on proliferation and invasion of glioma cells. Oncotarget. 2017;8(44):76949-76960.[17] Cheng Q, Zhang Z, Zhang S, et al. Human umbilical cord mesenchymal stem cells protect against ischemic brain injury in mouse by regulating peripheral immunoinflammation. Brain Res. 2015;1594:293-304.[18] Yuan-Hsiang Chang, Abe K, Yokota H, et al. Human induced pluripotent stem cell region recognition in microscopy images using Convolutional Neural Networks. Conf Proc IEEE Eng Med Biol Soc. 2017;2017:4058-4061.[19] Pang AL, Xiong LL, Xia QJ, et al. Neural Stem Cell Transplantation Is Associated with Inhibition of Apoptosis, Bcl-xL Upregulation, and Recovery of Neurological Function in a Rat Model of Traumatic Brain Injury. Cell Transplant. 2017;26(7):1262-1275.[20] Gothié JD, Sébillot A, Luongo C, et al. Adult neural stem cell fate is determined by thyroid hormone activation of mitochondrial metabolism. Mol Metab. 2017;6(11):1551-1561.[21] Huang P, Gebhart N, Richelson E, et al. Mechanism of mesenchymal stem cell-induced neuron recovery and anti-inflammation. Cytotherapy. 2014;16(10):1336-1344.[22] Choi C, Oh SH, Noh JE, et al. Attenuation of Postischemic Genomic Alteration by Mesenchymal Stem Cells: a Microarray Study. Mol Cells. 2016;39(4):337-344.[23] 田胜男,王博,李琦,等.诱导多能干细胞的安全性及应用研究进展[J].中国组织工程研究,2017,21(5):815-820.[24] Lu P, Ceto S, Wang Y, et al. Prolonged human neural stem cell maturation supports recovery in injured rodent CNS. J Clin Invest. 2017;127(9):3287-3299.[25] 杨炎歌,段淑荣.脑梗死后VEGF及bFGF对神经干细胞增殖分化的机制研究进展[J].中国卒中杂志,2016,11(8):704-708.[26] Song S, Park JT, Na JY, et al. Early expressions of hypoxia-inducible factor 1alpha and vascular endothelial growth factor increase the neuronal plasticity of activated endogenous neural stem cells after focal cerebral ischemia. Neural Regen Res. 2014;9(9):912-918.[27] Natalwala A, Kunath T. Preparation, characterization, and banking of clinical-grade cells for neural transplantation: Scale up, fingerprinting, and genomic stability of stem cell lines. Prog Brain Res. 2017;230:133-150.[28] Bulstrode H, Johnstone E, Marques-Torrejon MA, et al. Elevated FOXG1 and SOX2 in glioblastoma enforces neural stem cell identity through transcriptional control of cell cycle and epigenetic regulators. Genes Dev. 2017;31(8):757-773.[29] Gao M, Dong Q, Zhang H, et al. Syringe needle skull penetration reduces brain injuries and secondary inflammation following intracerebral neural stem cell transplantation. Exp Ther Med. 2017;13(3):885-890.[30] Malloy KE, Li J, Choudhury GR, et al. Magnetic Resonance Imaging-Guided Delivery of Neural Stem Cells into the Basal Ganglia of Nonhuman Primates Reveals a Pulsatile Mode of Cell Dispersion. Stem Cells Transl Med. 2017;6(3):877-885.[31] Yaghoobi K. Neural regeneration after spinal cord injury treatment by lavandula angustifolia and human umbilical mesanchymal stem cell transplantation. Neural Regen Res. 2017;12(1):68-69.[32] Marsh SE, Blurton-Jones M. Neural stem cell therapy for neurodegenerative disorders: The role of neurotrophic support. Neurochem Int. 2017;106:94-100.[33] Meneghini V, Frati G, Sala D, et al. Generation of Human Induced Pluripotent Stem Cell-Derived Bona Fide Neural Stem Cells for Ex Vivo Gene Therapy of Metachromatic Leukodystrophy. Stem Cells Transl Med. 2017;6(2):352-368.[34] Ozaki M, Iwanami A, Nagoshi N, et al. Evaluation of the immunogenicity of human iPS cell-derived neural stem/progenitor cells in vitro. Stem Cell Res. 2017;19: 128-138.[35] Srivastava AK, Gross SK, Almad AA, et al. Serial in vivo imaging of transplanted allogeneic neural stem cell survival in a mouse model of amyotrophic lateral sclerosis. Exp Neurol. 2017;289:96-102.[36] Chen NN, Wei F, Wang L, et al. Tumor Necrosis Factor Alpha Induces Neural Stem Cell Apoptosis Through Activating p38 MAPK Pathway. Neurochem Res. 2016;41(11):3052-3062.[37] Bacigaluppi M, Russo GL, Peruzzotti-Jametti L, et al. Neural Stem Cell Transplantation Induces Stroke Recovery by Upregulating Glutamate Transporter GLT-1 in Astrocytes. J Neurosci. 2016;36(41):10529-10544.[38] Eckert A, Huang L, Gonzalez R, et al. Bystander Effect Fuels Human Induced Pluripotent Stem Cell-Derived Neural Stem Cells to Quickly Attenuate Early Stage Neurological Deficits After Stroke. Stem Cells Transl Med. 2015;4(7):841-851.[39] Wang X, Yu X, Xie C, et al. Rescue of Brain Function Using Tunneling Nanotubes Between Neural Stem Cells and Brain Microvascular Endothelial Cells. Mol Neurobiol. 2016;53(4): 2480-2488.[40] Cheng Y, Zhang J, Deng L, et al. Intravenously delivered neural stem cells migrate into ischemic brain, differentiate and improve functional recovery after transient ischemic stroke in adult rats. Int J Clin Exp Pathol. 2015;8(3):2928-2936.[41] Wu MF, Zhang SQ, Gu R, et al. Transplantation of erythropoietin gene-modified neural stem cells improves the repair of injured spinal cord. Neural Regen Res. 2015;10(9): 1483-1490.[42] 梁锐超,方芳.内源性神经干细胞在中枢神经系统创伤修复中的研究进展[J].华西医学,2014,29(1):150-154.[43] 王启征,王丽娟,张雄.脑缺血后神经可塑性的研究进展[J].中华老年心血管病杂志,2017,19(2):217-219. |
| [1] | Lin Qingfan, Xie Yixin, Chen Wanqing, Ye Zhenzhong, Chen Youfang. Human placenta-derived mesenchymal stem cell conditioned medium can upregulate BeWo cell viability and zonula occludens expression under hypoxia [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 4970-4975. |
| [2] | Pu Rui, Chen Ziyang, Yuan Lingyan. Characteristics and effects of exosomes from different cell sources in cardioprotection [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 1-. |
| [3] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [4] | Wang Xianyao, Guan Yalin, Liu Zhongshan. Strategies for improving the therapeutic efficacy of mesenchymal stem cells in the treatment of nonhealing wounds [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1081-1087. |
| [5] | Wang Shiqi, Zhang Jinsheng. Effects of Chinese medicine on proliferation, differentiation and aging of bone marrow mesenchymal stem cells regulating ischemia-hypoxia microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1129-1134. |
| [6] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [7] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [8] | Hou Jingying, Yu Menglei, Guo Tianzhu, Long Huibao, Wu Hao. Hypoxia preconditioning promotes bone marrow mesenchymal stem cells survival and vascularization through the activation of HIF-1α/MALAT1/VEGFA pathway [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 985-990. |
| [9] | Shi Yangyang, Qin Yingfei, Wu Fuling, He Xiao, Zhang Xuejing. Pretreatment of placental mesenchymal stem cells to prevent bronchiolitis in mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 991-995. |
| [10] | Liang Xueqi, Guo Lijiao, Chen Hejie, Wu Jie, Sun Yaqi, Xing Zhikun, Zou Hailiang, Chen Xueling, Wu Xiangwei. Alveolar echinococcosis protoscolices inhibits the differentiation of bone marrow mesenchymal stem cells into fibroblasts [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 996-1001. |
| [11] | Fan Quanbao, Luo Huina, Wang Bingyun, Chen Shengfeng, Cui Lianxu, Jiang Wenkang, Zhao Mingming, Wang Jingjing, Luo Dongzhang, Chen Zhisheng, Bai Yinshan, Liu Canying, Zhang Hui. Biological characteristics of canine adipose-derived mesenchymal stem cells cultured in hypoxia [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1002-1007. |
| [12] | Geng Yao, Yin Zhiliang, Li Xingping, Xiao Dongqin, Hou Weiguang. Role of hsa-miRNA-223-3p in regulating osteogenic differentiation of human bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1008-1013. |
| [13] | Lun Zhigang, Jin Jing, Wang Tianyan, Li Aimin. Effect of peroxiredoxin 6 on proliferation and differentiation of bone marrow mesenchymal stem cells into neural lineage in vitro [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1014-1018. |
| [14] | Zhu Xuefen, Huang Cheng, Ding Jian, Dai Yongping, Liu Yuanbing, Le Lixiang, Wang Liangliang, Yang Jiandong. Mechanism of bone marrow mesenchymal stem cells differentiation into functional neurons induced by glial cell line derived neurotrophic factor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1019-1025. |
| [15] | Duan Liyun, Cao Xiaocang. Human placenta mesenchymal stem cells-derived extracellular vesicles regulate collagen deposition in intestinal mucosa of mice with colitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1026-1031. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||