Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (23): 3751-3758.doi: 10.3969/j.issn.2095-4344.0286
Previous Articles Next Articles
Efficacy and safety of drainage placement after primary total knee arthroplasty: a meta-analysis
Tang Jian, Wang Ren-chong, Tang Zhong-fei, Li Bai-chuan
- Department of Shoulder and Elbow Surgery, West Branch of Liuzhou Worker’s Hospital, Liuzhou 545001, Guangxi Zhuang Autonomous Region, China
-
Online:2018-08-18Published:2018-08-18 -
About author:Tang Jian, Master, Attending physician, Department of Sports Medicine and Shoulder and Elbow Surgery, West Branch of Liuzhou Worker’s Hospital, Liuzhou 545001, Guangxi Zhuang Autonomous Region, China
CLC Number:
Cite this article
Tang Jian, Wang Ren-chong, Tang Zhong-fei, Li Bai-chuan. Efficacy and safety of drainage placement after primary total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2018, 22(23): 3751-3758.
share this article

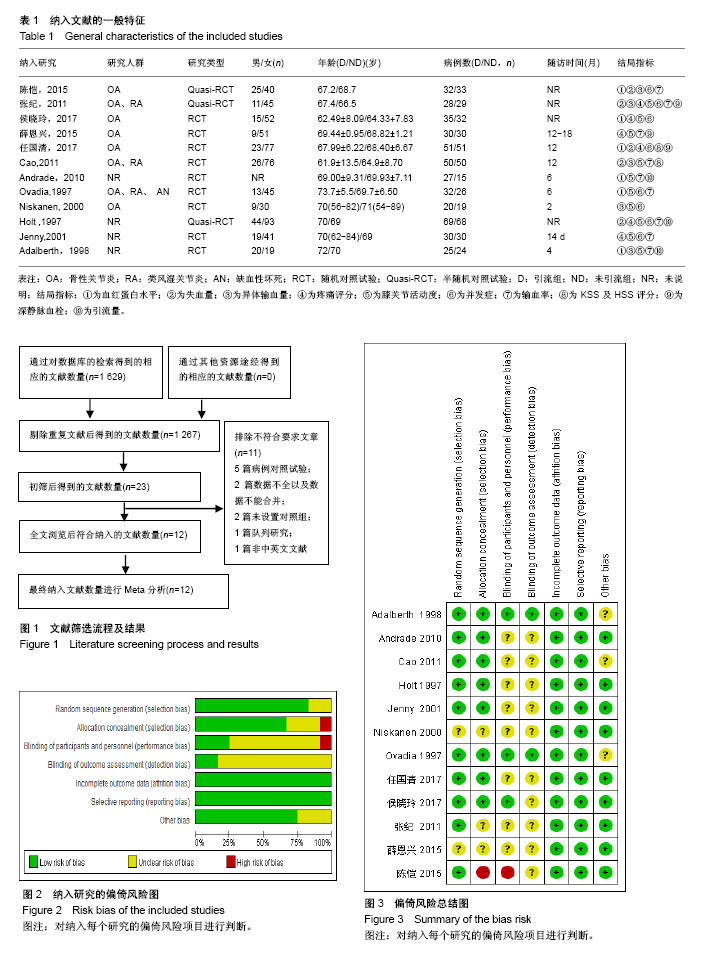
2.1 文献检索结果及纳入研究的方法学质量 根据制定的文献检索策略总共检索到1 629篇相关文献,通过阅读文献题目和摘要,排除重复文献362篇,不合符纳入标准和排除标准的文献的1 244篇,阅读全文排除不符合要求的文献11篇。最终纳入12篇文献,其中中文文献5篇,英文文献7篇,随机对照试验9篇,半随机对照试验3篇。总共纳入836例患者,其中引流组为429例,未引流组为407例,见表1。文献筛选流程及结果,见图1。 纳入的12篇文献质量相对较高,论证强度较大。12篇文献中有10篇文献采用的正确的随机方法,4篇文献未采用分配隐藏或未告知分配隐藏的方法,10篇文献盲法(对研究者、受试者、评价者施盲)的情况不清楚,所有纳入文献的数据均完整,所有研究均未存在失访。因此,纳入的文献在选择性偏倚、实施偏倚、测量偏倚及随访偏倚、报告偏倚的可能性比较小。纳入文献随访的时间长短不一,大部分均在12个月,可能会影响论证的强度。此次,系统评价纳入的研究的方法学质量较高,具有代表性,见图2,3。"

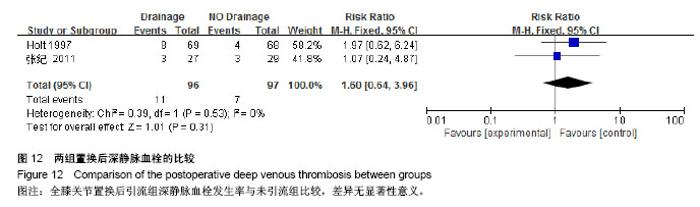
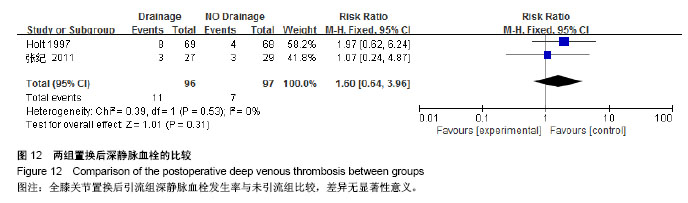
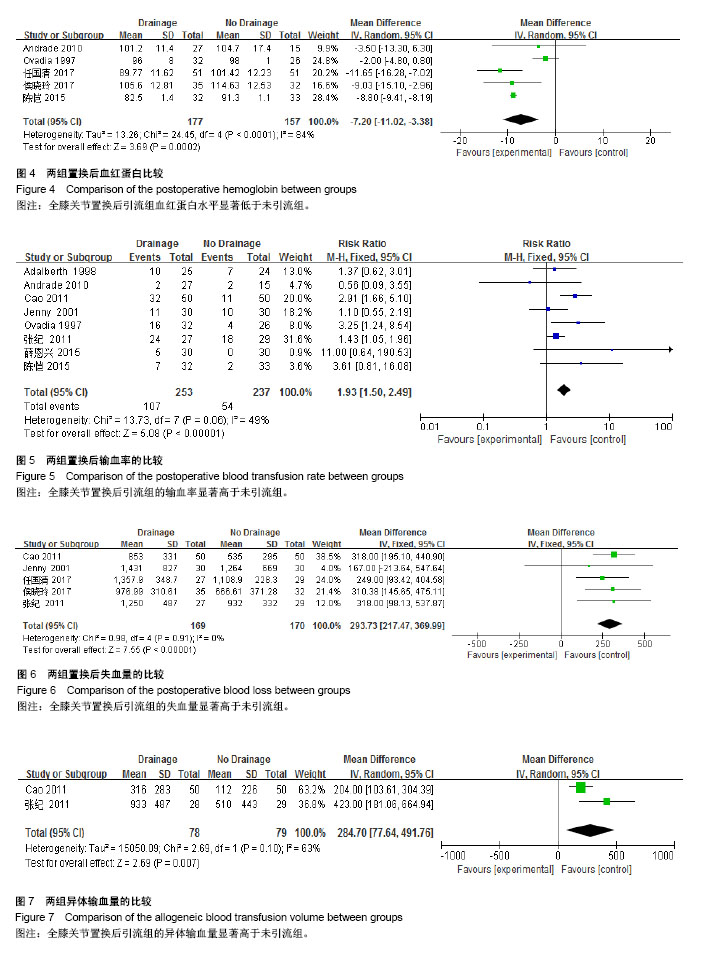
2.2 Meta分析结果 2.2.1 置换后血红蛋白 纳入12篇文献中只有8篇文献报道了术后血红蛋白的值,其中3篇文献的数值不能合并。8篇文献报道了置换后血红蛋白的比较[9,11-13,15-16,18,20],其中有2篇文献给出的是置换后血红蛋白下降值[12,18],1篇文献给出的是置换后血红蛋白范围[20]。最后5篇文献的数据纳入Meta分析[9,11,13,15-16],总共334例患者,其中引流组177例,未引流组157例,各研究间有异质性(P < 0.000 1,I2=84%),采用随机效应模型进行Meta分析,结果显示全膝关节置换后引流组血红蛋白要低于未引流组[MD= -7.20,95%CI(-11.02,-3.38),P=0.000 2]。见图4。 2.2.2 置换后输血率 纳入的文献中有8篇文献报道了置换后输血率的比较[9-10,12,13-16,19-20],总共490例患者,其中引流组253例,未引流组237例,各研究间有同质性(P=0.006,I2=49%),采用固定效应模型进行Meta分析,结果显示全膝关节置换后引流组输血率显著高于未引流组[RR=1.93,95%CI(1.50,2.49),P < 0.000 01]。见图5。 2.2.3 置换后失血量 纳入的文献中有5篇文献报道了置换后失血量的比较[10-11,13-14,19],总共339例患者,其中引流组169例,未引流组170例,各研究间有同质性(P=0.91, I,采用固定效应模型进行Meta分析,结果显示全膝关节置换后引流组失血量要显著高于未引流组[MD= 293.73,95%CI(217.47,369.99),P < 0.000 01],见图6。2=0%) 2.2.4 异体输血量 纳入的文献中有7篇文献报道了异体输血量的比较[9-10,14,16-18,20],其中有4篇文献给出的是异体输血量均值[16-18,20],1篇文献未引流组给出异体输血量均值[9]。最后2篇文献数据纳入Meta分析[10,14],总共157例患者,其中引流组78例,未引流组79例,各研究间有异质性(P=0.10,I2=63%),采用随机效应模型进行Meta分析,结果显示全膝关节置换后引流组异体输血量显著高于未引流组[MD=284.70,95%CI(77.64,491.76),P=0.007]。见图7。"

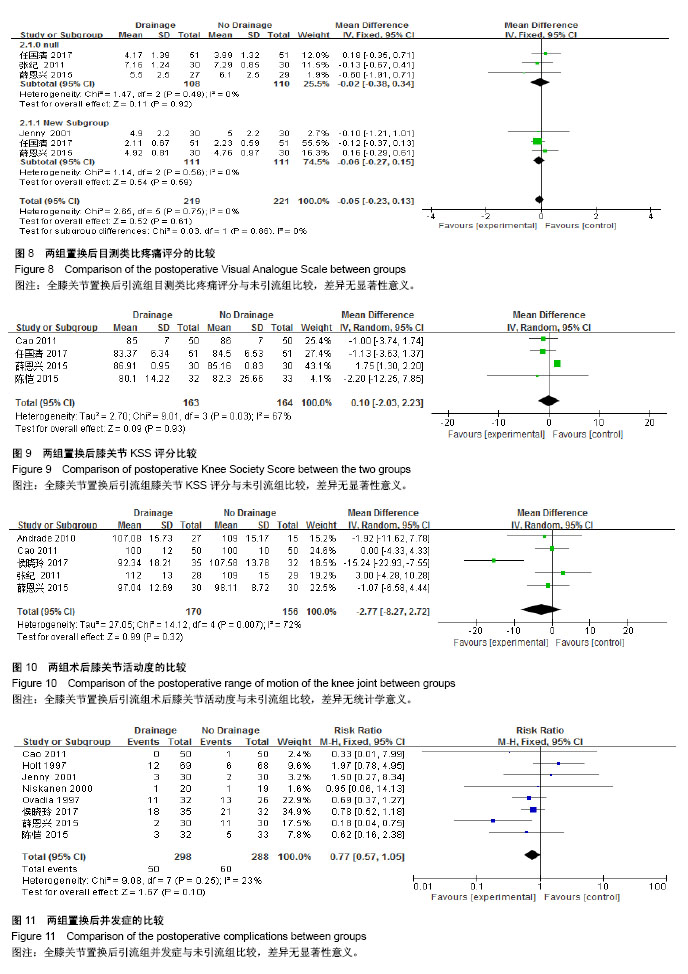
2.2.5 置换后VAS疼痛评分 纳入的文献中有6篇文 献报道了置换后VAS疼痛评分的比较[10-13,18-19],其中有1篇文献给出的是置换后镇痛药物剂量[18],另外1篇文献给出的是置换后VAS平均值[12]。最后4篇文献的数据纳入Meta分析[10-11,13,19],总共278例患者,其中引流组138例,未引流组140例。3篇文献报道了置换后第1天VAS疼痛评 分[10-11,13],总共218例患者,其中引流组108例,未引流组110例,各研究间有同质性(P=0.48,I2=0%),采用固定效应模型进行Meta分析,结果显示全膝关节置换后引流组第1天VAS疼痛评分与未引流组比较差异无显著性意义[MD=-0.02,95%CI(-0.38,0.34),P=0.92]。3篇文献报道了置换后第7天VAS疼痛评分[11,13,19],总共222例患者,其中引流组111例,未引流组111例,各研究间有同质性(P=0.75,I2=0%),采用固定效应模型进行Meta分析,结果显示全膝关节置换后引流组第7天VAS疼痛评分与未引流组比较差异无显著性意义[MD=-0.06,95%CI(-0.27,0.15),P=0.86]。见图8。 2.2.6 置换后膝关节KSS评分 纳入的文献中有4篇文 献报道了置换后膝关节KSS评分的比较[9,12-14],总共327例患者,其中引流组163例,未引流组164例,各研究间有异质性(P=0.03,I2=67%),采用随机效应模型进行Meta分析,结果显示全膝关节置换后引流组膝关节KSS评分与未引流组比较差异无显著性意义[MD=0.10,95%CI(-2.03,2.23),P=0.93]。见图9。 2.2.7 置换后膝关节活动度 纳入的文献中有9篇文 献报道了置换后膝关节活动度的比较[10-12,14-18,20],其中有3篇文献给出的是置换后膝关节活动度的范围[17-18,20],1篇文献给出的是置换后膝关节活动度的均值[16]。最后5篇文 献的数据纳入Meta分析[10-12,14-16],总共326例患者,其中引流组170例,未引流组156例,各研究间有异质性(P=0.007,I2=72%),采用随机效应模型进行Meta分析,结果显示全膝关节置换后引流组术后膝关节活动度与未引流组比较差异无显著性意义[MD=-2.77,95%CI(-8.27,2.72),P=0.32]。见图10。 2.2.8 置换后并发症 纳入的文献中有10篇文献报道了置换后并发症的比较[10-14,16-19],其中有2篇文献报道置换后并发症为0[10,13]。最后8篇文献数据纳入Meta分析[11-13,16-19],总共586例患者,其中引流组298例,未引流组288例,各研究间有同质性(P=0.25,I2=23%),采用固定效应模型进行Meta分析,结果显示全膝关节置换后引流组并发症与未引流组比较差异无显著性意义[RR=0.77,95%CI(0.57,1.05),P=0.10]。见图11。 "
| [1] Ebert JR, Munsie C, Joss B, et al. Guidelines for the early restoration of active knee flexion after total knee arthroplasty: Implications for rehabilitation and early intervention.Arch Phys Med Rehabil. 2014;95(6):1135-1140.[2] 裴福兴.中国髋、膝关节置换的现状及展望[J].中国骨与关节杂志, 2012, 1(1):4-8.[3] Waugh TR, Stinchficld FE. Suction drainage of orthopaedic wounds.J Bone Joint Surg.1961;43 :939-946.[4] Huang Z, Ma J, Pei F, et al.Meta-analysis of temporary versus no clamping in TKA. Orthopedics. 2013;36(7):543-550.[5] Heyse TJ, Haas SB, Drinkwater D, et al. Intraarticular fibrinogen does not reduce blood loss in TKA: A randomized clinical trial. Clin Orthop Relat Res. 2014; 472(1): 272-276.[6] 高明堂,蒋电明,张保龙.全膝关节置换术后引流时效性的临床评价[J].中华创伤杂志,2012,11:1018-1020.[7] Omonbude D, Masry MA, Connor PJ, et al. Measurement of joint effusion and haematoma formation by ultrasound in assessing the effectiveness of drains after total knee replacement: A prospective randomised study. J Bone Joint Surg Br. 2010;92(1): 51-55. [8] Esler CNA, Blakeway C, Fiddian NJ,The use of a closed-suction drain in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. 2003;85(2): 215-217. [9] 陈恺.全膝关节置换术后未放置引流管的有效性及安全性分析[J].福建医药杂志,2015,37(1):27-29.[10] 张纪,张洪.人工膝关节置换术后留置引流与否的对比研究[J].中华外科杂志,2011,49(12):1119-1122.[11] 侯晓玲,李玲利,涂晓晴,等.非止血带下初次全膝关节置换术安置引流与否的前瞻性对照研究[J].四川大学学报(医学版). 2017.48(2):326-328.[12] 薛恩兴,陈成旺,张宇.人工全膝关节置换术后是否留置引流对患者疗效影响的对比研究[J].中华全科医学, 2015,13(7):1111-1113.[13] 任国清,刘红云,滕学仁,等.人工全膝关节置换后是否放置引流管:随机对照试验[J].中国组织工程研究.2016,20(22):3219-3226.[14] Li C, Nijat A, Askar M.No clear advantage to use of wound drains after unilateral total knee arthroplasty: a prospective randomized, controlled trial. J Arthroplasty. 2011;26(4): 519-522 .[15] de Andrade MA, de Oliveira Campos TV, Silva BF, et al. Six month follow-up of patients submitted to total knee arthroplasty with and without placement of suction drainage devices. Rev Bras Ortop. 2010;45(6): 549-553. [16] Ovadia D, Luger E, Bickels J, et al. Efficacy of closed wound drainage after total joint arthroplasty. A prospective randomized study. J Arthroplasty. 1997;12(3): 317-321.[17] Niskanen RO, Korkala OL, Haapala J, et al. Drainage is of no use in primary uncomplicated cemented hip and knee arthroplasty for osteoarthritis: a prospective randomized study. J Arthroplasty. 2000; 15(5):567-569.[18] Holt BT, Parks NL, Engh GA, et al. Comparison of closed-suction drainage and no drainage after primary total knee arthroplasty. 1997; 20(12):1121-1124. [19] Jenny JY, Boeri C, Lafare S,No drainage does not increase complication risk after total knee prosthesis implantation: a prospective, comparative, randomized study. Knee Surg Sports Traumatol Arthrosc. 2001;9(5): 299-301.[20] Adalberth G, Byström S, Kolstad K ,et al. Postoperative drainage of knee arthroplasty is not necessary: a randomized study of 90 patients. Acta Orthop Scand.1998;69(05): 475-478. [21] Quinn M, Bowe A,Galvin R,et al.The use of postoperative suction drainage in total knee arthroplasty: a systematic review.Int Orthop. 2015;39(4):653-658.[22] Jung WH, Chun CW, Lee JH, et al. No difference in total blood loss, haemoglobin and haematocrit between continues and intermittent wound drainage after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2013;21 (12):2831-2836.[23] White RH, Henderson MC. Risk factors for venous thromboembolism after total hip and knee replacement surgery. Curr Opin Pulm Med. 2002;8(5):365-371.[24] 赵丽君,张惠清.全膝关节置换术后切口引流的临床观察[J].临床合理用药,2013,6 (4) :23-24.[25] 高娜,石跃.一期双侧人工全膝关节置换术后放置引流对患者康复进程的影响[J].中华现代护理杂,2011,17(35):4314-4315.[26] Wang G, Wang D, Wang B, et al. Efficacy and safety evaluation of intra-articular injection of tranexamic acid in total knee arthroplasty operation with temporarily drainage close. Int J Clin Exp Med. 2015; 8(8):14328-14334.[27] Seo JG, Lee SA, Moon YW, et al. Infrapatellar fat pad preservation reduces wound complications after minimally invasive total knee arthroplasty. Arch Orthop Trauma. Surg. 2015;135(8):1157-1162.[28] Kudrna J. New oral anticoagulants after total knee arthroplasty: clinical considerations for orthopaedic surgeons. Curr Orthop Pract. 2013; 24(4):424-432. |
| [1] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [2] | Li Dadi, Zhu Liang, Zheng Li, Zhao Fengchao. Correlation of total knee arthroplasty efficacy with satisfaction and personality characteristics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1346-1350. |
| [3] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [4] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [5] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [6] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [7] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [8] | Yuan Jiawei, Zhang Haitao, Jie Ke, Cao Houran, Zeng Yirong. Underlying targets and mechanism of Taohong Siwu Decoction in prosthetic joint infection on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1428-1433. |
| [9] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [10] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [11] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [12] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [13] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [14] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [15] | Zhong Hehe, Sun Pengpeng, Sang Peng, Wu Shuhong, Liu Yi. Evaluation of knee stability after simulated reconstruction of the core ligament of the posterolateral complex [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 821-825. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||