Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (11): 1786-1791.doi: 10.3969/j.issn.2095-4344.0180
Previous Articles Next Articles
Perioperative hidden blood loss in unilateral total knee arthroplasty: problems and characteristics
Wang Yun-long, Zhen Ping
- Orthopedic Center of PLA, Lanzhou General Hospital, Lanzhou 730050, Gansu Province, China
-
Online:2018-04-18Published:2018-04-18 -
Contact:Zhen Ping, Professor, Chief physician, M.D., Orthopedic Center of PLA, Lanzhou General Hospital, Lanzhou 730050, Gansu Province, China -
About author:Wang Yun-long, Master candidate, Orthopedic Center of PLA, Lanzhou General Hospital, Lanzhou 730050, Gansu Province, China
CLC Number:
Cite this article
Wang Yun-long, Zhen Ping. Perioperative hidden blood loss in unilateral total knee arthroplasty: problems and characteristics[J]. Chinese Journal of Tissue Engineering Research, 2018, 22(11): 1786-1791.
share this article
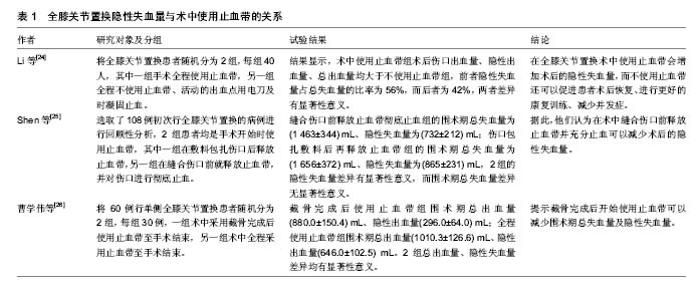
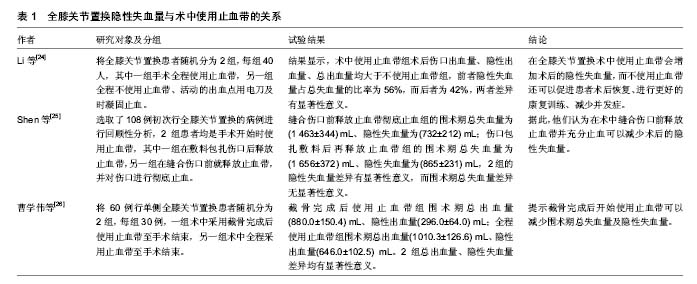
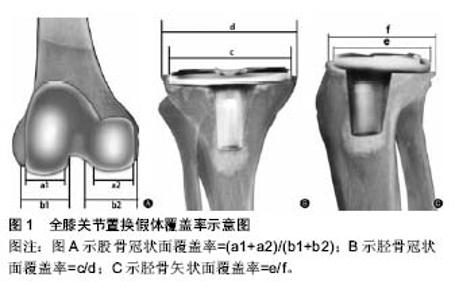
2.1 隐性失血量的计算 全膝关节置换的总出血量包括显性出血量与隐性出血量两个部分,故隐性出血量=总出血量-显性出血量。显性出血量由术中出血及术后伤口引流量组成,总出血量通常使用Gross方程估算得出[7],因此也可称为预估出血量。Gross于1983年首次提出使用围术期平均红细胞压积计算有效循环血量的线性方程,其在实践中验证了该方法的准确性,实际上通过Gross方程计算的血液丢失量已经基本接近真实情况,除非患者的失血量巨大或者迅速失血使得方程偏离正常的基线。Gross方程是通过术前、术后红细胞压积的变化值及术前的有效循环血量,求得总出血量,即总出血量=术前有效血容量×(术前红细胞压积-术后红细胞压积)。术前的有效循环血量可以通过Nadler方法计算[8]:术前有效血容量=K1×身高3+K2×体质量+K3,其中身高的单位为m,体质量的单位为kg,男性患者:K1=0.366 9,K2=0.032 19,K3=0.604 1;女性患者:K1=0.356 1,K2=0.033 08,K3=0.183 3。使用Gross方程计算总出血量,术后红细胞压积对其计算准确性的影响最为显著。有些研究认为,可取术后两至三天红细胞压积进行计 算[5-6]。Prasad等[9]发现,全膝关节置换后的大部分患者血红蛋白持续下降,直至术后第7天才开始上升。李征等[10]在研究中同样发现,约有50%的患者红细胞压积和血红蛋白的最低值出现在术后4-7 d。因此取术后两至三天红细胞压积值进行计算并不准确,应当取术后7 d内所查红细胞压积的最低值进行计算较为妥当。 2.2 氨甲环酸的应用 近些年,各类纤溶蛋白酶抑制物在全膝关节置换术中广泛应用,以期降低出血量及输血量[11]。氨甲环酸是一种赖氨酸类似物,被认为是效果最好、副作用最小的纤溶蛋白酶抑制物[12],因此被广泛应用于牙科手术、心脏手术等[13-14]。它可与纤维蛋白上的赖氨酸结合位点可逆性结合,从而抑制纤维蛋白溶解、稳定血凝块,达到止血的目的[15]。已有大量的研究证实氨甲环酸可以降低全膝关节置换术的出血量[16-17],但对于减少隐性出血量的给药方式及剂量尚未有共识。 Xie等[18]进行了151例全膝关节置换静脉用氨甲环酸对照研究,他们将患者随机分为3组,分别在切皮前 3 h给予氨甲环酸10 mg/kg,切皮后3 h 10 mg/kg,切皮后3,6 h各给予10 mg/kg。结果显示平均隐性出血量切皮前组(763.0±373.3) mL,切皮后一次给药组(637.5± 303.5) mL,切皮后两次给药组(467.6±305.9) mL,结论认为静脉多次给药可以显著减少隐性失血量。Huang等[19]的一项临床对照研究显示,术后立刻给予15 mg氨甲环酸+100 mL生理盐水组与术后只给予100 mL生理盐水组相比,隐性失血量显著降低[(170.8±37.2) mL,(364.2 mL±41.5) mL],同时输血率也显著降低(3.7%,25.9%)。冯贵喜等[20]对380例全膝关节置换患者进行观察,他们将患者分为3组,在术中紧密缝合关节囊后分别局部注射浓度为30 g/L的氨甲环酸生理盐水50 mL,10 g/L的氨甲环酸生理盐水50 mL,普通生理盐水 50 mL。术后的隐性失血量分别是(693.29±377.91) mL、(835.42±481.97) mL、(1 032.75±322.19) mL,差异有显著性意义,给药组要小于未给药组,高浓度组要小于低浓度组,同时输血率也随着药物浓度的增加而降低。 无论何种给药方式,使用氨甲环酸均能降低全膝关节置换术后隐性失血量。在安全浓度范围内,给药浓度与隐性失血降低量呈正相关性。 2.3 术中止血带的使用 目前,全膝关节置换术中常规使用止血带,其优势是可以减少术中出血、使术野清晰、有利于骨水泥的使用、缩短手术时间等,对这一点均已形成共识[21]。最近的一项Meta分析显示,使用止血带可以减少术中及总出血量[22]。然而,止血带的直接压迫可使软组织局部缺血。使用止血带增加血栓形成风险的同时,下列并发症也被认为与使用止血带相关:术后患肢肿胀、关节僵硬、伤口延迟愈合、神经麻痹、血管损伤、横纹肌溶解、大腿皮下脂肪坏死及术后大腿疼痛[23]。使用止血带是否会降低术后隐性失血量,以及术中是否应该释放止血带、使用止血带的时机等问题,大多数学者还存在着争议,见表1。 Li等[24]进行了一项80例患者的有关止血带对全膝关节置换术隐性失血量的前瞻性研究。他们将患者随机分为2组,每组40人,其中一组手术全程使用止血带,另一组全程不使用止血带、活动的出血点用电刀及时凝固止血。研究结果显示术中使用止血带组术后伤口出血量、隐性出血量、总出血量均大于不使用止血带组,前者隐性失血量占总失血量的比率为56%,而后者为42%,两者差异有显著性意义。因此他们认为在全膝关节置换术中使用止血带会增加术后的隐性失血量,而不使用止血带还可以促进患者术后恢复、进行更好的康复训练、减少并发症。Shen等[25]选取了108例初次行全膝关节置换的病例进行回顾性分析,2组患者均是手术开始时使用止血带,其中一组在敷料包扎伤口后释放止血带,另一组在缝合伤口前就释放止血带,并对伤口进行彻底止血。他们的研究结果是,缝合伤口前释放止血带彻底止血组的围术期总失血量为(1 463±344) mL、隐性失血量为(732±212) mL;伤口包扎敷料后再释放止血带组的围术期总失血量为(1 656±372) mL、隐性失血量为(865±231) mL,2组的隐性失血量差异有显著性意义,而围术期总失血量差异无显著性意义。据此,他们认为在术中缝合伤口前释放止血带并充分止血可以减少术后的隐性失血量。曹学伟等[26]同样也对术中使用止血带的不同方法进行了研究。他们将60例行单侧全膝关节置换的患者随机分为2组,每组30例,一组术中采用截骨完成后使用止血带至手术结束,另一组术中全程采用止血带至手术结束。发现截骨完成后使用止血带组围术期总出血量(880.0±150.4) mL、隐性出血量(296.0±64.0) mL;全程使用止血带组围术期总出血量(1 010.3±126.6) mL、隐性出血量(646.0±102.5) mL。2组总出血量、隐性失血量差异均有显著性意义,据此,他们认为截骨完成后开始使用止血带可以减少围术期总失血量及隐性失血量。国内还有文献指出术中止血带的使用时间与隐性失血量存在较大的相关性,随着止血带使用时间的延长对组织造成的机械性和缺血性损伤也随之加重[27]。 手术全程使用止血带与其他使用止血带方法及不使用止血带相比均会增加围术期的总出血量及隐性出血量,其原因一方面是由于机械性因素导致缺血再灌注损伤造成局部纤溶剂激活、诱发溶血反应,以及长时间缺血产生大量的过氧化物引起血管通透性增加等[24]。另一方面在不使用或不全程使用止血带的情况下,在无止血带的时候微小血管出血非常明显,术中可以彻底止血,减少术后微小血管出血及肌肉渗血,从而降低了术后隐性失血量[26]。"
2.4 术后患肢体位 术后患肢的体位可以影响静脉血流速率、关节囊内压力等,进而影响全膝关节置换术后隐性失血量[28]。Li等[29]通过一项108例全膝关节置换术患者前瞻性研究支持这一结果。他们将患者随机分为2组,2组患者术后均在踝关节下放置一垫子,使患肢高于心脏平面,根据经验他们将这一垫子的厚度定为25 cm,其中膝关节弯曲组在小腿近侧端再放置一20 cm厚的垫子。他们观察到术后膝关节弯曲组的膝关节周径增加了3.1%,术后膝关节完全伸直组周径增加了4.7%,因此他们认为术后适度(< 30°)弯曲膝关节可以明显减少隐性失血量及膝关节肿胀程度,且患肢的静脉血流速率前者亦明显高于后者。郭兵等[30]对60例行人工全膝关节置换术的患者进行观察,他们将患者随机分为2组,分别为术后6 h髋膝关节均完全伸直、术后6 h屈髋30°屈膝70°。结果发现,术后6 h髋膝关节完全伸直组隐性失血量为(480.23±57.64) mL,占总失血量的47.2%;术后6 h屈髋屈膝组隐性失血量为(315.23±56.32) mL,占总失血量的31.75%,两者差异有显著性意义。因此研究结果认为,术后将患肢屈髋30°、屈膝70°与髋、膝关节均完全伸直相比,前者可有效降低术后的隐性失血量。 抬高患肢可降低术后隐性失血量,其可能的机制是下肢长时间完全伸直,腘窝处局部张力较高,会使该处的静脉血管处于拉紧状态,进而影响静脉回流。而抬高的肢体使静脉血管张力降低,可以促进静脉血液回流,从而减少隐性出血。且弯曲的膝关节腔内压力较高,同样有止血效果。弯曲患肢膝关节还可加速恢复术后下肢功能,对于术后恢复是一种简单易行且廉价的方法[29]。 2.5 计算机辅助技术的应用 20世纪90年代,Stindel 等[31]在膝关节置换术中使用计算机导航系统,开启了无影像导航系统在该类手术中的应用。无影像导航系统是指没有采用患者任何术前或术后的影像资料(包括X射线片、CT、MRI及C臂透视),而是在术中通过安置在手术区域的三维光学定位装置,实时获取关节的解剖、肢体的机械轴线和关节的位置等信息,经过计算机处理后,形成患肢三维模拟工作模型[31]。 Singla等[32]报告使用德国蛇牌Orthopilot导航系统,应用计算机辅助技术进行57例全膝关节置换随机对照研究。该系统采用特殊的数学算法进行膝关节运动中心配准[33]。与传统手术相比,计算机辅助导航系统手术中不破坏股骨与胫骨的骨髓腔,股骨与胫骨的截骨均在导航系统的辅助下精准完成。他们的结论是:传统手术平均总失血量980 mL,导航系统辅助手术平均总失血量970 mL,隐性失血量分别为54.8%,59.5%,总出血量与隐性出血量两种手术方式无明显差异。可能的原因是虽然运用导航系统没有开放股骨、胫骨的骨髓腔,但止血带的使用时间比传统手术要长(15-20 min),已有多篇研究结果报道止血带的使用会增加总的出血量,因此未开放骨髓腔所减少的出血量被延长止血带使用时间引起的出血所抵消[32]。Saragaglia等[34]报告使用Orthopilot导航系统可以提高截骨的精确度,避免矫正不足或过度,比传统手术减少了超出预定目标范围的病例。因此,使用导航系统虽然不能减少隐性出血量,但对术后下肢力线、运动功能恢复有很大帮助。 2.6 置换假体与膝关节的匹配 在中国国内使用和制造的膝关节置换假体,很多都是根据西方人膝关节解剖、形态参数设计的。然而东西方人种之间膝关节的解剖和形态存在较大的差异[35-37]。因此,伴随着全膝关节置换术手术量在国内的与日俱增,根据西方人体参数设计的假体跟国人膝关节不匹配的问题也越来越显著[37]。假体的几何形状与截骨面出现错配,就可能增加全膝关节置换术手术的隐性出血量[35-36]。Gao等[38]对120例全膝关节置换患者(男36例,占30%;女84例,占70%;平均年龄64.8岁)。他们通过术后拍摄膝关节正侧位X射线片,用假体的长径除以截骨面的长径获得假体的覆盖率(图1)。术后计算得到股骨冠状面、胫骨冠状面、胫骨矢状面的假体覆盖率分别是(87.9±2.5)%,(88.5±2.2)%,(89.1±2.3)%。然后分别记录了术后1 d及术后3 d的隐性失血量,通过Pearson相关系数分析证实术后隐性失血量与假体覆盖率存在显著相关性,即覆盖率越大、隐性失血量越小。国内有文献对使用股骨髁间开放式假体及股骨髁间闭合式假体术后隐性失血量进行比较,发现后者的隐性失血量小于前者,差异有显著性意义[27]。 许多需要行全膝关节置换的患者为骨性关节炎、类风湿关节炎晚期患者,这些患者的膝关节解剖已不同于正常解剖[35]。有亚洲学者比较了亚洲人与其他人种的病态膝关节,结果显示前者前后径与内外侧径的比值高于后者[35-37]。在中国大量使用设计参数来源于西方人种的假体,这就要求手术医生术前判断假体与截骨面的覆盖率[38]。如果假体与截骨面的匹配度不高,会使更多的截骨面暴露,增加术后隐性出血量[39]。手术医生可以同时测量患膝的前后径及内外侧径计算二者比值,通过该比值选择假体要优于采用平均值及标准差[26]。 2.7 游离脂肪酸 在全膝关节置换过程中,打入股骨髓腔的髓腔挫、股骨柄假体等都会导致髓腔内压力增高,此时增高的压力会使髓腔内的脂滴通过毛细血管进入血液循环[40]。这些游离的脂肪酸可以刺激中性粒细胞产生大量的过氧化物及其代谢产物[41-42],当其水平超过机体的代谢平衡时,就会损伤红细胞胞膜及胞浆内的血红蛋白,使得红细胞变形、破裂、分解[43-44]。 Bao等[41]提出假说,隐性失血与游离脂肪酸导致红细胞损伤与血红蛋白破坏有关,他们预测在术中及术后使用抗氧化剂药物可以降低隐性失血量。王绍刚等[45]对42例全膝关节置换患者术后的游离脂肪酸、血红蛋白等指标进行研究,他们分别记录了术前、术后24,48,72,96 h血红蛋白量、红细胞计数及隐性失血量,观察到上述指标均在术后持续下降,至术后96 h平稳,而游离脂肪酸含量在术后骤升,术后24 h达到最高值,至术后96 h逐渐恢复正常。初步确认了循环血液中游离脂肪酸会在术后隐性失血中发挥一定作用。"

| [1] Leta TH, Lygre SH, Skredderstuen A,et al. Failure of aseptic revision total knee arthroplasties. Acta Orthop.2015;86(1):48-57.[2] Lemaire R. Strategies for blood management in orthopaedic and trauma surgery. J Bone Joint Surg Br. 2008;90(9):1128-1136.[3] Ferraris VA, Brown JR, Despotis GJ, et al. 2011 update to the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists blood conservation clinical practice guideline. Ann Thorac Surg. 2011;91(3):944-982.[4] Sehat KR, Evans R, Newman JH. How much blood is really lost in total knee arthroplasty: correct blood loss management should take hidden loss into account. Knee. 2000;7(3):151-155.[5] Newman JH, Bowers M, Murphy J. The clinical advantages of autologous transfusion. A randomized, controlled study after knee replacement. J Bone Joint Surg Br. 1997;79(4):630-632.[6] Sehat KR, Evans Rl, Newman JH. Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br. 2004;86(4): 561-565.[7] Gross JB, Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983;58(3):277-280.[8] Nanler SB, Hidalgo JU, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;57:224-232.[9] Prasad N, Padmanabhan V, Mullaji A. Blood loss in total knee arthroplasty: an analysis of risk factors. Orthop. 2007;31(1):39-44.[10] 李征,曹光磊,沈惠良.全膝关节置换术的隐性失血及影响因素分析[J].中华创伤杂志,2010,26(9):831-834.[11] Eubanks JD. Antifibrinolytics in major orthopaedic surgery. Am Acad Orthop Surg. 2010;18:132-138.[12] Roy SP, Tanki UF, Dutta A, et al. Efficacy of intra-articular tranexamic acid in blood loss reduction following primary unilateral total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:2494-2501.[13] MJ C. The use of topical crushed tanexamic acid tablets to control bleeding after dental surgery and from skin ulcers in haemophilia. Haemophlia. 2007;13:443-444.[14] Dhillon MS, Bali K, Prabhakar S. Tranexamic acid for control of blood loss in bilateral total knee replacement in a single stage. Indian J Orthop. 2011;45:148-152.[15] MacGillivray RG, Tarabichi SB, Hawari MF, et al. Tranexamic acid to reduce blood loss after bilateral total knee arthroplasty: a prospective, randomized double blind study. Artoroplasty.2011; 26:24-28.[16] Lee SH, Cho KY, Khurana S, et al. Less blood loss under concomitant administration of tranexamic acid and indirect factor Xa inhibitor following total knee arthroplasty: a prospective randomized controlled trial. Knee Surg Sports Traumatol Artorosc. 2013;21:2611-1617.[17] Shen PF, Hou WL, Chen JB et al. Effectiveness and safety of tranexamic acid for total knee arthroplasty: a prospective randomized trial. Med Sci Monit. 2015;21:576-581.[18] Xie J, Ma J, Yao H, et al. Multiple boluses of intravenous tranexamic acid to reduce hidden blood loss after primary total knee arthroplasty without tourniquet: a randomized clinical trial. J Arthroplasty. 2016;31:2458-2464.[19] Huang GP, Jia XF, Xiang Z, et al. Tranexamic acid reduces hidden blood loss in patients undergoing total knee arthroplasty: a comparative study and meta-analysis. Med Sci Monit. 2016;22: 797-802.[20] 冯贵喜,刘军,张福江,等.氨甲环酸局部应用对单侧全膝关节置换术后隐性失血量的影响[J].中华骨科杂志, 2016,36(3):151-155.[21] Hersekli MA, Akpinar S, Ozkoc G, et al. The timing of tourniquet release and its influence on blood loss after total knee arthroplasty. Inter Orthop. 2004;28:138-141.[22] Alcelik I, Pollock RD, Sukeik M, et al. A comparison of out comes with and without a tourniquet in total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. Arthroplasty. 2002;27(3):331-340.[23] Smith TO, Hing CB. Is a tourniquet beneficial in total knee replacement surgery? A meta-analysis and systematic review. Knee. 2012;17(2):141-147.[24] Li B, Wen Y, Wu H, et al. The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop. 2009;33: 1263-1268.[25] Shen HL, Li Z, Feng ML, et al. Analysis on hidden blood loss of total knee arthroplasty in treating knee osteoarthritis. Chin Med J. 2011;124(11):1653-1656.[26] 曹学伟,杨伟毅,梁比记,等.不同止血带使用方法对TKA围手术期失血量影响的临床研究[J].中国骨与关节外科,2011,4(6): 455-459.[27] 高福强,李子剑,张克,等.初次全膝关节置换术后隐性失血的影响因素研究[J].中华外科杂志, 2011,49(5):419-423.[28] Faldini C, Traina F, De Fine M, et al. Post-operative limb position can influence blood loss and range of motion after total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrose. 2015;23(3):852-859.[29] Li B, Wang G, Wang Y, et al. Effect of two limb positions on venous hemodynamics and hidden blood loss following total knee arthroplasty. Knee Surg. 2017;30:70-74.[30] 郭兵,陈小杰,郭卫.体位对初次人工膝关节置换术后隐性失血的影响[J].中国矫形外科杂志, 2013,21(3):305-306.[31] Stindel E, Merloz P, Graf P, et al. Computer assisted orthopedics surgery. Rev Chir Orthop Reparatrice Appar Mot. 2007, 93(4): 11-32.[32] Singla A, Malhotra R, Kumar V, et al. A randomized controlled study to compare the total and hidden blood loss in computer assisted surgery and conventional surgical technique of total knee replacement. Clin Orhop Surg. 2015;7:211-216.[33] 吴昊.无需影像导航系统在矫形外科的应用[J].中国矫形外科,2009, 13(9):1681-1686. [34] Saragaglia D, Roberts J. Navigated osteotomies around the knee in 170 patients with osteoarthritis secondary to genu varum. Orthopedics. 2005;28(10):1269-1274.[35] Cheng CK, Lung CY, Lee YM, et al. A new approach of designing the tibial baseplate of total knee prostheses. Clin Biomech. 1999; 14:112-117.[36] Uehara K, Kadoya Y, Kobayashi A, et al. Anthropometry of the proximal tibia to design a total knee prosthesis for the Japanese population. Arthroplasty. 2002;17:1028-1032.[37] Kwak DS, Surendran S, Pengatteeri YH, et al. Morphometry of the proximal tibia to design the tibial component of total knee arthroplasty for the Korean population. Knee. 2007;14:295-300.[38] Gao FQ, Guo WS, Sun W, et al. Correlation between the coverage percentage of prosthesis and postoperative hidden blood loss in primary total knee arthroplasty. Chin Med J. 2014; 127(12):2265-2269.[39] 高福强,李子剑,刘延青,等.初次全膝关节置换术后隐性失血的影响因素研究[J].中华外科杂志, 2011,49(5):419-423.[40] O’Connor MI, Brodersen MP, Feinglass NG, et al. Fat emboli in total knee arthroplasty: a prospective randomized study of computer-assisted navigation vs standard surgical technique. Arthroplasty. 2010;25(7):1034-1040.[41] Bao N, Zhou L, Cong Y, et al. Free fatty acids are responsible for the hidden blood loss in total hip and knee arthroplasty. Med Hypotheses. 2013;81(1):104-107.[42] Schönfeld P, Wojtczak L. Fatty ackds as modulators of the cellular production of reactive oxygen species. Free Rad Bio Med. 2008; 45(3):231-241.[43] Das T, Firdaus SB, Mishro S, et al. Aqueous bark extract of Terminalia arjuna protects against phenylhydrazine induced oxidative damage in goat red blood cell membrane protein, phospholipid asymmetry and structural morphology: a flow cytometric and biochemical analysis. Phar Res. 2014;8(12): 1790-1804.[44] Ramkumar KM, Vijayakumar RS, Vanitha P, et al. Protective effect of gallic acid on alloxan-induced oxidative stress and osmotic fragility in rats. Human Exp Toxicol.2014;33(6):638-649.[45] 王绍刚,陶忠亮,汪胜,等.游离脂肪酸与全膝关节置换后隐性失血的相关性[J].中国骨与关节损伤, 2016,20(26):3830-3836. |
| [1] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [2] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [3] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [4] | Li Dadi, Zhu Liang, Zheng Li, Zhao Fengchao. Correlation of total knee arthroplasty efficacy with satisfaction and personality characteristics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1346-1350. |
| [5] | Wei Wei, Li Jian, Huang Linhai, Lan Mindong, Lu Xianwei, Huang Shaodong. Factors affecting fall fear in the first movement of elderly patients after total knee or hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1351-1355. |
| [6] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [7] | Xiao Guoqing, Liu Xuanze, Yan Yuhao, Zhong Xihong. Influencing factors of knee flexion limitation after total knee arthroplasty with posterior stabilized prostheses [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1362-1367. |
| [8] | Huang Zexiao, Yang Mei, Lin Shiwei, He Heyu. Correlation between the level of serum n-3 polyunsaturated fatty acids and quadriceps weakness in the early stage after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1375-1380. |
| [9] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [10] | Yuan Jiawei, Zhang Haitao, Jie Ke, Cao Houran, Zeng Yirong. Underlying targets and mechanism of Taohong Siwu Decoction in prosthetic joint infection on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1428-1433. |
| [11] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [12] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [13] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [14] | Zhong Hehe, Sun Pengpeng, Sang Peng, Wu Shuhong, Liu Yi. Evaluation of knee stability after simulated reconstruction of the core ligament of the posterolateral complex [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 821-825. |
| [15] | Zhao Zhongyi, Li Yongzhen, Chen Feng, Ji Aiyu. Comparison of total knee arthroplasty and unicompartmental knee arthroplasty in treatment of traumatic osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 854-859. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||