[1] CHAY W, KIRSHBLUM S. Predicting Outcomes After Spinal Cord Injury. Phys Med Rehabil Clin N Am. 2020;31(3):331-343.
[2] KIRSHBLUM S, SNIDER B, EREN F, et al. Characterizing Natural Recovery after Traumatic Spinal Cord Injury. J Neurotrauma. 2021;38(9):1267-1284.
[3] ELI I, LERNER DP, GHOGAWALA Z. Acute Traumatic Spinal Cord Injury. Neurol Clin. 2021;39(2):471-488.
[4] IZZY S. Traumatic Spinal Cord Injury. Continuum (Minneapolis, Minn). 2024;30(1):53-72.
[5] BAI XY, LIU XL, DENG ZZ, et al. Ferroptosis is a new therapeutic target for spinal cord injury. Front Neurosci. 2023;17:1136143.
[6] LI JZ, FAN BY, SUN T, et al. Bioinformatics analysis of ferroptosis in spinal cord injury. Neural Regen Res. 2023;18(3):626-633.
[7] ANANDHAN A, DODSON M, SHAKYA A, et al. NRF2 controls iron homeostasis and ferroptosis through HERC2 and VAMP8. Sci Adv. 2023; 9(5):eade9585.
[8] 杜华勇,李泽辉,王晓昕,等. 脊髓损伤后微环境中免疫反应的文献计量分析[J]. 中国康复理论与实践,2024,30(11):1322-1333.
[9] LI X, FU J, GUAN M, et al. Biochanin A attenuates spinal cord injury in rats during early stages by inhibiting oxidative stress and inflammasome activation. Neural Regen Res. 2024;19(9):2050-2056.
[10] 李姝君,漆国栋,漆伟,等. 川芎嗪对脊髓损伤后小鼠神经保护作用的实验研究[J]. 中国中药杂志,2023,48(14):3848-3854.
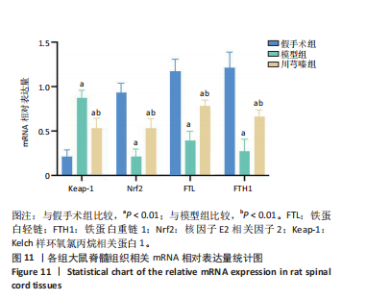
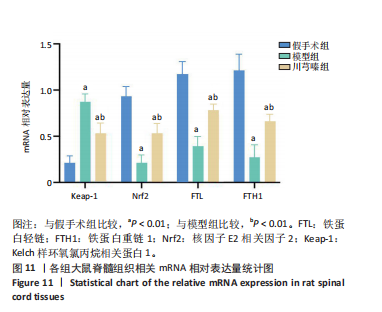
[11] 陶经纬,周婧雅,赵毅,等. 川芎嗪对脊髓损伤大鼠铁死亡的调控作用及机制[J]. 中国组织工程研究,2024,28(26):4158-4163.
[12] 范筱,陶经纬,蒋昇源,等. 川芎嗪对大鼠脊髓损伤后铁代谢的影响[J]. 中国组织工程研究,2023,27(22):3561-3566.
[13] 吴杨鹏,范筱,张俐. 急性脊髓损伤动物模型的建立与评估[J]. 中国组织工程研究,2016,20(49):7341-7348.
[14] FAN X, ZANG C, LAO K, et al. Neuroprotective effects of tetramethylpyrazine on spinal cord injury-Related neuroinflammation mediated by P2X7R/NLRP3 interaction. Eur J Pharmacol. 2024;964:176267.
[15] HU J, LANG Y, CAO Y, et al. The Neuroprotective Effect of Tetramethylpyrazine Against Contusive Spinal Cord Injury by Activating PGC-1α in Rats. Neurochem Res. 2015;40(7):1393-1401.
[16] 贺丰,穆晓红,付玲玲,等. 脊髓损伤的中医研究现状[J]. 世界中西医结合杂志,2017,12(3):440-444.
[17] 张刘波,周峻,王佩佩,等. 脊髓损伤中医药辨证论治研究进展[J]. 现代中西医结合杂志,2020,29(16):1813-1817.
[18] 范筱,徐立柱,陶经纬,等. 脊髓损伤“气滞血瘀”病机理论与铁死亡的关系[J]. 世界中医药,2024,19(8):1188-1191.
[19] LI F, WANG H, CHEN H, et al. Mechanism of Ferroptosis and Its Role in Spinal Cord Injury. Front Neurol. 2022;13:926780.
[20] SHI Z, YUAN S, SHI L, et al. Programmed cell death in spinal cord injury pathogenesis and therapy. Cell prolif. 2021;54(3):e12992.
[21] LIU G, DENG B, HUO L, et al. Tetramethylpyrazine alleviates ferroptosis and promotes functional recovery in spinal cord injury by regulating GPX4/ACSL4. Eur J Pharmacol. 2024;977:176710.
[22] ZHU Z, LI J, SONG Z, et al. Tetramethylpyrazine attenuates renal tubular epithelial cell ferroptosis in contrast-induced nephropathy by inhibiting transferrin receptor and intracellular reactive oxygen species. Clin Sci (Lond). 2024;138(5):235-249.
[23] LIU J, REN Z, YANG L, et al. The NSUN5-FTH1/FTL pathway mediates ferroptosis in bone marrow-derived mesenchymal stem cells. Cell Death Discov. 2022;8(1):99.
[24] OHSHIMA T, YAMAMOTO H, SAKAMAKI Y, et al. NCOA4 drives ferritin phase separation to facilitate macroferritinophagy and microferritinophagy. J Cell Biol. 2022;221(10):e202203102.
[25] ZHANG N, YU X, XIE J, et al. New Insights into the Role of Ferritin in Iron Homeostasis and Neurodegenerative Diseases. Mol Neurobiol. 2021; 58(6):2812-2823.
[26] YANATORI I, KISHI F, TOYOKUNI S. New iron export pathways acting via holo-ferritin secretion. Arch Biochem Biophys. 2023;746:109737.
[27] WANG Y, QIU S, WANG H, et al. Transcriptional Repression of Ferritin Light Chain Increases Ferroptosis Sensitivity in Lung Adenocarcinoma. Front Cell Dev Biol. 2021;9:719187.
[28] LEE J, HYUN DH. The Interplay between Intracellular Iron Homeostasis and Neuroinflammation in Neurodegenerative Diseases. Antioxidants (Basel). 2023;12(4):918.
[29] SHEN L, LIN D, LI X, et al. Ferroptosis in Acute Central Nervous System Injuries: The Future Direction? Front Cell Dev Biol. 2020;8:594.
[30] BAIRD L, YAMAMOTO M. The Molecular Mechanisms Regulating the KEAP1-NRF2 Pathway. Mol Cell Biol. 2020;40(13):e00099-20.
[31] LIU S, PI J, ZHANG Q. Signal amplification in the KEAP1-NRF2-ARE antioxidant response pathway. Redox Biol. 2022;54:102389.
[32] CRISMAN E, DUARTE P, DAUDEN E, et al. KEAP1-NRF2 protein-protein interaction inhibitors: Design, pharmacological properties and therapeutic potential. Med Res Rev. 2023;43(1):237-287.
[33] CHEW LY, ZHANG H, HE J, et al. The Nrf2-Keap1 pathway is activated by steroid hormone signaling to govern neuronal remodeling. Cell Rep. 2021;36(5):109466.
[34] LIU C, WU X, BING X, et al. H1N1 influenza virus infection through NRF2-KEAP1-GCLC pathway induces ferroptosis in nasal mucosal epithelial cells. Free Radic Biol Med. 2023;204:226-242.
[35] UCAR BI, UCAR G, SAHA S, et al. Pharmacological Protection against Ischemia-Reperfusion Injury by Regulating the Nrf2-Keap1-ARE Signaling Pathway. Antioxidants (Basel). 2021;10(6):823.
[36] HE F, RU X, WEN T. NRF2, a Transcription Factor for Stress Response and Beyond. Int J Mol Sci. 2020;21(13):4777.
[37] WANG L, ZHANG X, XIONG X, et al. Nrf2 Regulates Oxidative Stress and Its Role in Cerebral Ischemic Stroke. Antioxidants (Basel). 2022; 11(12): 2377.
[38] YAN R, LIN B, JIN W, et al. NRF2, a Superstar of Ferroptosis. Antioxidants (Basel). 2023;12(9):1739.
[39] FENG H, WANG L, ZHANG G, et al. Oxidative stress activated by Keap-1/Nrf2 signaling pathway in pathogenesis of preeclampsia. Int J Clin Exp Pathol. 2020;13(3):382-392.
[40] YU H, GAO Y, ZHOU R. Oxidative Stress From Exposure to the Underground Space Environment. Front Public Health. 2020;8:579634.
[41] HSU WL, WANG CM, YAO CL, et al. Blockage of Nrf2 and autophagy by L-selenocystine induces selective death in Nrf2-addicted colorectal cancer cells through p62-Keap-1-Nrf2 axis. Cell Death Dis. 2022;13(12):1060.
|