Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (36): 5877-5883.doi: 10.12307/2024.747
Previous Articles Next Articles
Impact of measurement of joint space width on effectiveness and prognosis of medial unicondylar knee arthroplasty
Xu Gengbin, Ru Jiangying
- Department of Orthopedics, The Sixth Affiliated Hospital of Guangzhou Medical University, Qingyuan People’s Hospital, Qingyuan 511518, Guangdong Province, China
-
Received:2023-11-01Accepted:2023-12-14Online:2024-12-28Published:2024-02-28 -
Contact:Ru Jiangying, MD, Associate professor, Chief physician, Master’s supervisor, Department of Orthopedics, The Sixth Affiliated Hospital of Guangzhou Medical University, Qingyuan People’s Hospital, Qingyuan 511518, Guangdong Province, China -
About author:Xu Gengbin, Master candidate, Department of Orthopedics, The Sixth Affiliated Hospital of Guangzhou Medical University, Qingyuan People’s Hospital, Qingyuan 511518, Guangdong Province, China
CLC Number:
Cite this article
Xu Gengbin, Ru Jiangying. Impact of measurement of joint space width on effectiveness and prognosis of medial unicondylar knee arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(36): 5877-5883.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

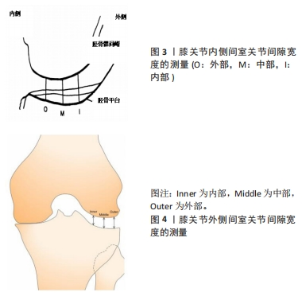
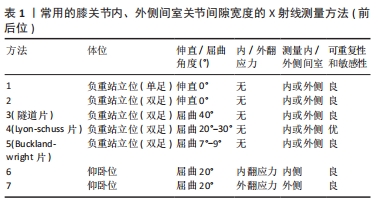
2.1 膝关节JSW的测量方法 影像学发展至今,X射线检查和临床评估一直是诊断骨关节炎的标准方法。1957年提出的主要基于X射线检查进行膝骨关节炎分级的Kellgren-Lawrence(KL)方案[32],目前仍在广泛使用。但有研究表明,对于有关节镜证实存在关节间隙狭窄而无明显骨赘的膝骨关节炎患者,通过KL量表无法进行分类,故通过JSW和骨赘两个不同变量进行膝骨关节炎的全面评估,可能更为科学、合理[2]。与其他成像手段相比,如超声波、磁共振等,JSW的X射线片测量被认为是目前评估软骨破坏进展最佳的替代方法,也被美国食品和药品管理局(Food and Drug Admini-stration,FDA)和欧洲医疗产品人类药物委员会评估机构,推荐作为评估改善病情的骨关节炎药物临床试验的终点指标[33-34]。目前有多种测量膝关节内、外侧间室JSW的X射线片方法,见表1。但由于其测量受许多因素的影响,包括检查者的经验、患者的固定体位、负重程度、中心X射线束与胫骨平台前后缘对齐的水平及膝关节的旋转和屈曲程度等,故每一种测量方法的可重复性和敏感性也不尽相同。"

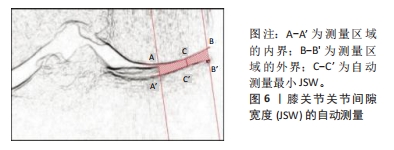
并且他们对这些手动的测量方法做了相关研究。然而,JANSEN等[36]研究表明,负重位X射线片上测量的JSW与MRI测量软骨厚度变化之间的相关性较差,可能与软骨的变形能力及半月板外突有关。此外,PIPERNO等[37]使用图像分析计算机(Mediscan,Hologic)和由T. Conrozier开发的髋关节关节间隙测量软件,最早对膝关节内、外侧间室的关节间隙面积、平均JSW和mJSW分别进行了自动测量,见图5。他们将X射线片先经过512/512像素和256级灰度的数字化处理,计算机再通过自动确定关节边缘两侧端点,以恒定的172°角度反复修改最终获得非常清晰的胫股关节间隙的轮廓,其中测量内侧间室时采用胫骨平台关节缘两侧端点,而测量外侧间室时则采用股骨髁关节边缘两侧端点。然后,计算机自动测量内或外侧间室关节间隙面积、平均JSW和mJSW。"
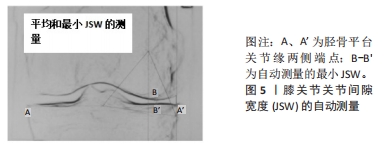

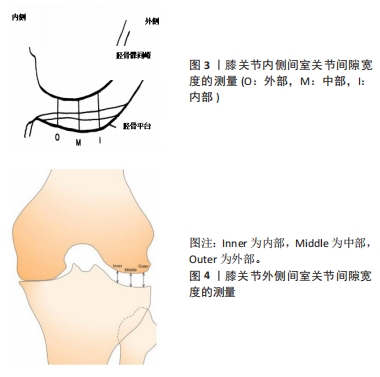
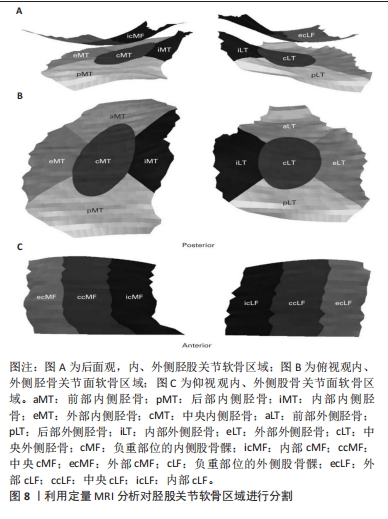
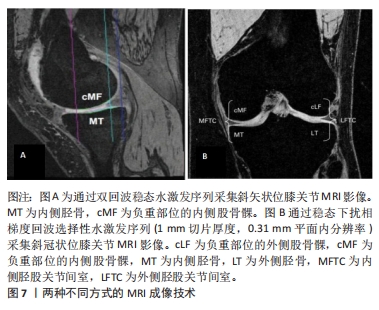
首先,他们通过数字化图像对测量区域进行精确描绘,其外侧界限在胫股关节内侧或外侧的非骨赘边缘处划定,而在距外侧边界恒定距离处由计算机自动确定内侧边界。mJSW是目前临床上定量膝骨关节炎关节间隙狭窄程度的一个主要参数,而CHEUNG等[39]基于深度学习的模型,提出一种计算机辅助工具,通过对关节空间参数的全自动、准确和高效的计算,以自动方式连续测量多个固定位置的JSW,结果表明,与常用的mJSW相比,多位置JSW的自动测量法在膝骨关节炎严重程度分级和预测疾病进展方面更有效。JSW的测量是对软骨厚度的间接反映。虽然绝对JSW与软骨厚度相关,但是通过软骨厚度变化来解释的JSW变异在健康个体中还不及一半。由于绝对JSW与个人身高之间存在显著相关性,即身高差异也会导致绝对JSW测量误差[40],PAIXAO 等[40]描述了一种新的由IB Lab KoALA软件包衡量的标准化JSW定量测量方法,结果显示,其对关节间隙狭窄的变化更敏感,也比绝对JSW更适合跟踪关节间隙狭窄等级的变化。 2.3 其他测量方法 尽管X射线平片是评估关节JSW的主要方法,但在确定纵向进展方面,对随时间变化的敏感性较差。超声波检查与普通X射线片相比,具有无电离辐射、分辨率更高和性能更快的优势。YANGGISAWA等[41]报道了一种使用超声波测量膝关节JSW的方法,即测量从股骨周围皮质到胫骨周围皮质的距离,但由于股骨内髁内侧边缘为弧形结构,故在超声波检查中,股骨内髁内侧边缘与胫骨内侧边缘并不在同一条直线上。在此基础上,ZHU 等[42]在膝关节内侧间室重新定义了4个相对稳定的测量点,通过超声波进行JSW测量,结果表明,其可有效避免干扰JSW测量的诸多影响因素,如测量对象体位、超声扫描程序、测量部位、测量方法和阅读器。通过标准化的超声波扫描程序提高了JSW测量的可重复性。 另有研究表明,采用易显示软骨和软组织的MRI成像技术对缺失的软骨进行定量分析,结果比X射线片评估更敏感[43-44],并可预测骨关节炎患者是否需要行膝关节置换手术[45-46]。通过稳态下扰相梯度回波序列(1 mm切片厚度,0.31 mm平面内分辨率)或三维双回波稳态水激发序列三维双回波稳态水激发序列采集斜冠状位和斜矢状位MRI影像,见图7,使用专有软件(Chondrometrics GmbH,Ainring, Germany)对胫股软骨进行定量分析;先采用盲法对内、外侧胫股关节面软骨区域进行分割,胫骨部位分5个区域(中央、外部、内部、前部和后部),股骨部位分3个区域(中央、外部和内部),共16个区域。基于以上16个区域,可独立计算各区域的平均软骨厚度(ThCtAB.Me),也可使用扩展有序值方法确定与位置无关的软骨厚度变化(按绝对值计算)[47-48],见图8。此外,与传统的固定屈曲位X射线片相比,三维负重位CT成像技术已被证明对检测骨赘、软骨下囊肿、软骨和半月板形态更加灵敏和准确。与MRI相比,三维负重位CT扫描时间更短(≤2 min)、底板更小(1.2 cm×1.5 cm)、价格和维护成本更低。KOTHARI等[49]应用三维负重位CT成像技术测量膝关节JSW,结果表明,在JSW < 2.0 mm的内侧胫股区域与躯体功能之间似乎存在关联性。TURMEZEI等[50-51]研究报道,三维负重位CT成像技术可在三个维度上提供JSW的个性化测量,从而提高检测膝关节重要结构变化的灵敏度和可重复性,故可作为一种评估膝骨关节炎疾病进展的时间和成本效应的替代方法。"

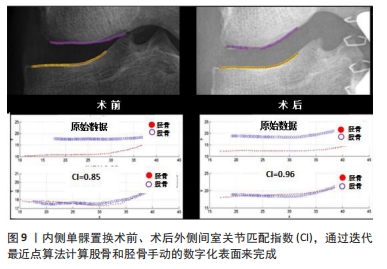
2.4 术前内侧间室JSW对内侧活动平台UKA疗效的影响 以牛津(Oxford)单髁为代表的活动平台假体最早于1978年推出,经过不断改良和验证,于1998年又推出第3代活动平台的Oxford单髁假体系统,其主要适应证包括膝关节内侧间室全层软骨损伤伴严重疼痛的骨关节炎患者,屈曲20°可矫正内翻畸形、小于15°的屈曲或内翻畸形、前交叉韧带完整和股骨内髁骨坏死的患者[17]。但在临床实践中,经常碰到膝关节内侧持续疼痛并有明确“一指征”的患者,在负重位X射线片上内侧间室出现关节间隙狭窄,却未呈现全层软骨损伤的征象。此时,许多关节外科医生会为之感到困惑,困惑一是除了负重位X射线片,是否需要进一步行MRI,甚至关节镜检查,来明确骨关节炎病变是否已发展至全层软骨缺失或全层软骨损伤的程度;困惑二是对有明确骨关节炎症状而仅部分软骨缺失或未达到全层软骨损伤(即JSW=0 mm)磨损程度的患者,是否可行UKA术。因此,对于UKA术的手术指征,一直以来是临床骨科医生争议的热点问题。 NIINIM?KI等[18]对113例行内侧UKA术的膝骨关节炎患者进行了一项回顾性研究,平均随访时间为63个月。结果表明,术前内侧间室JSW > 2 mm组患者术后的假体翻修率是JSW < 2 mm组的6倍(P < 0.001),并且术前内侧JSW/外侧JSW > 40%组患者术后的假体翻修率是内侧JSW/外侧JSW < 40%组的8倍(P < 0.001),而年龄、性别、关节镜检查结果或体质量指数与翻修率无关。对于关节间隙仅有部分软骨缺失的患者,其疼痛来源可能并非软骨损伤,而是由于早期炎症递质的释放,此类患者行UKA术的疗效可能不太令人满意。PANDIT等[19]在注册有 1 000多例行内侧间室牛津(Oxford)UKA术患者的数据库中,选取29例术前存在部分软骨缺失患者、29例内侧间室两侧骨暴露患者和29例内侧间室两侧骨缺失患者,进行了一项回顾性研究。研究表明,在平均随访2年(1-6年)中,部分软骨缺失组患者术后牛津膝关节评分显著低于骨暴露组和骨缺失组(P < 0.001);在部分软骨缺失组中约21%的患者并未从内侧间室UKA术中获益,而骨暴露组和骨缺失组中所有患者均获益。部分软骨缺失组患者未获益的原因可能在于:①疼痛可能并非来源于膝关节的内侧间室;②对疼痛有更高的期望和较低的耐受性;③软骨无神经支配,不会产生疼痛。在以往的关于无症状膝关节的尸体解剖研究中,已证实内侧间室软骨厚度部分损伤的发生率很高[19]。与NIINIM?KI等[18]和PANDIT等[19]结果不一致的是,MAIER等[20]回顾性分析了64例行内侧间室UKA术膝骨关节炎患者的临床疗效和假体生存率。结果显示,在牛津膝关节评分、美国膝关节协会评分、目测类比评分和末次随访时膝关节最大屈曲度方面,部分软骨缺失组和全层软骨缺失组患者之间比较差异均无统计学意义(P均> 0.05);尽管如此,部分软骨缺失组的假体5年累计生存率(84%)低于全层软骨缺失组(92%)。翻修风险增加可能与外科医生扩大UKA手术指征有关;术前可通过拍摄前后位、侧位、站立负重位和内翻/外翻应力位X射线片,来排除膝关节内侧间室存在部分软骨缺失情况的患者。同样,KNIFSUND等[21]对241例(294侧)内侧间室膝骨关节炎患者行第3代牛津UKA术,平均随访时间8.7年。结果显示,与术前KL分级(3-4级)组患者相比,KL分级(0-2级)组患者UKA术后具有更高的翻修风险(OR=1.89,95%CI:1.03-3.45,P=0.04)。显然,KL分级越高,JSW则越窄,UKA术后的假体翻修率也将越低。有趣的是,HAMILTON等[22]研究了94例术前存在部分软骨缺失的膝骨关节炎患者和188例术前存在全层软骨缺失的膝骨关节炎患者(1∶2),行内侧间室UKA术后的临床结果与假体生存率。结果表明,在术后1,2和5年随访时,部分软骨缺失组患者与全层软骨缺失组患者的假体生存率比较差异无显著性意义(P > 0.05),但部分软骨缺失组术后行关节镜检查的再手术率(10.9%)较全层软骨缺失组(3.9%)高出3倍;此外,与全层软骨缺失组患者相比,部分软骨缺失组患者术后的功能结果明显更差(P < 0.05)。尽管一些部分软骨缺失组患者在UKA术后也能获得良好的临床疗效,但目前尚不能在术前有效筛选出适合行UKA术的部分软骨缺失组患者,而JSW测量在一定程度上可间接反映关节间隙软骨缺失情况。WURM等[23]选取150例膝骨关节炎患者,分为JSW(0-1 mm)组和JSW(≥2 mm)组,术后1年随访时结果显示,术前JSW(0-1 mm)组患者的WOMAC功能评分和5年假体生存率均显著优于JSW(≥2 mm)组(P均< 0.05),该结果再次证实了部分软骨缺失患者并不适合行UKA手术。 然而,CARLSON等[24]报道,对于术前X射线片上非全层软骨损伤的重度膝骨关节炎患者,UKA也是一种安全可靠的手术选择,不应将缺乏全层软骨损伤作为活动平台UKA术的禁忌证。原因在于先前的研究存在一定的局限性,均未按国际膝关节文献委员会验证的骨关节炎分级系统(A-D级)来确定每个膝关节的严重程度,即轻度或重度膝骨关节炎患者均可能被纳入非全层软骨损伤组。该文作者将163例(185膝)D级重度骨关节炎患者,分为全层软骨损伤组(94膝)和非全层软骨损伤组(91膝),并探讨了两组患者的临床结果与假体生存率。结果表明,在最后一次随访时,两组在膝关节协会疼痛评分和功能评分方面,差异均无显著性意义(P=0.59和P=0.90);此外,在术后8年假体生存率方面,两组差异也无显著性意义(P=0.62)。不可否认的是,除了JSW外,影响内侧UKA术疗效的因素可能还包括高龄、体质量指数、髌股关节退变程度、假体力线匹配不良、骨质疏松程度、医生手术技术、患者的体质等,故在确定UKA手术指征时,应权衡利弊、综合考虑后才能取得满意的疗效。此外,需要强调的是,在负重X射线片上测量的JSW,即使超过2 mm,也不能完全排除膝骨关节炎患者出现全层软骨缺失或全层软骨损伤,甚至股骨内髁骨坏死存在的可能性,故对于伴严重疼痛、非全层软骨损伤的膝骨关节炎患者,MRI检查、甚至关节镜检查可能有助于明确疼痛的来源。 2.5 对内侧固定平台UKA术疗效的影响 根据术前的影像学结果和现有的文献,对于固定平台UKA术的手术指征尚未达成普遍共识。大多数研究关注的是,对术前存在全层软骨损伤的膝骨关节炎患者行固定平台UKA术的临床结果,尚缺乏不同程度膝骨关节炎患者与固定平台UKA术后临床结果和假体生存率之间关系的研究报道。近年来,WONG等[25]研究了153例固定平台UKA术的膝骨关节炎患者,术前通过在站立负重位X射线片上测量内侧间室的mJSW,将所有患者分为4组,即0 mm组、< 2 mm组、2-4 mm组和> 4 mm组。随访时间超过10年,对4组患者术后的牛津膝关节评分、SF-36健康调查简表的生理评分和心理评分、膝关节协会临床评估系统的功能评分和膝关节评分、假体生存率分别进行比较分析。结果显示,在术后2年随访时,mJSW=0 mm组患者在膝关节功能评分方面显著低于mJSW < 2 mm组(P=0.047)和2-4 mm组(P=0.019);术后10年随访时,mJSW=0 mm组患者的功能评分显著低于mJSW > 4 mm组(P=0.013),而mJSW < 2 mm组的SF-36健康调查简表生理评分也显著低于2-4 mm组(P=0.001 1);此外,术后14年随访时,4组的累计假体生存率分别为28.9%,7.2%,12.8%和9.1%,虽然差异无显著性意义(P > 0.05),但mJSW=0 mm组具有假体翻修率升高的趋势。有趣的是,该结论与先前关于内侧间室JSW对内侧活动平台UKA术疗效影响的研究结果正相反,原因可能与假体设计有关。 2.6 内侧UKA术后外侧间室JSW变化对预后的影响 大量研究表明,UKA术后假体生存率显著低于全膝关节置换术,而外侧间室软骨退变是影响内侧UKA术后假体生存率的最常见的并发症之一[18,26-27]。众所周知,外侧间室的软骨完整性对于恰当选择UKA术至关重要,在内侧UKA术中,经过精确确定假体置放和插入适当厚度的垫块,而实现韧带平衡的恢复和部分内翻畸形的矫正。VASSO等[28]报道,保留轻度内翻畸形(< 7°)可改善内侧UKA术后的疗效,在最后一次随访时,所有患者均未出现外侧间室软骨退变及骨关节炎进展。然而,目前尚无能够完全阻止外侧间室退变的方法。因此,亟待确定一种经济可靠的影像学方法测量外侧间室JSW的变化,来判定内侧UKA术后外侧间室软骨的退变程度,以及时有效地阻止外侧间室骨关节炎的进展。令人遗憾的是,至今尚缺乏关于这方面的研究文献报道。YUE等[29]对42例行内侧UKA术的患者开展了一项前瞻性研究,术后使用3种不同的膝关节X射线测量方法,包括站立负重下前后位X射线片、膝关节屈曲20°前后位X射线片(仰卧位)和膝关节屈曲20°外翻应力位X射线片(仰卧位),分别对患者外侧间的JSW进行了评估和比较,并在站立负重下前后位X射线片上测量了髋-膝-踝角度,同时对术前、术后髋-膝-踝角度和外侧间室JSW之间的关系进行了线性分析。结果显示,在不同时间点,3种X射线方法测量的外侧间隙JSW之间差异均无显著性意义(P均> 0.05),3种膝关节X射线方法经过验证,对测量外侧间室JSW均具有较好的准确性和可重复性。尽管如此,对于行内侧UKA术后伴发关节不稳定或严重外翻畸形等情况的患者,仍有必要在膝关节屈曲20°外翻应力位X射线片(仰卧位)下进行外侧间室JSW的测量。此外,术前和术中确认外侧间室关节软骨的完整性、确保手术对韧带平衡性的恢复及保留轻度内翻畸形的力线,可能有助于延缓外侧间室骨关节炎的进展及延长UKA术后假体生存率。鉴于外侧间室骨关节炎进展仍是内侧UKA术后假体翻修的主要指征,KHAMAISY等[30]对174例行内侧UKA术的患者进行了一项回顾性研究,评估了术后外侧间室关节匹配度和JSW的变化。在膝关节隧道位X射线片(站立位屈曲40°)上,应用专门开发的基于迭代最近点的软件代码(MATLAB,MathWorks Inc,Natick,MA,2012)计算关节一致性程度,以匹配指数表示,见图9。其中,匹配指数=1表示几何形态完全一致,匹配指数=0示关节面100%脱位。同时,按图4的方法对外侧间室JSW进行了测量。结果显示,所有患者术后匹配指数值和外侧间室JSW较术前均有显著改善(P均< 0.001)。但此次研究仍无法确定外侧间室匹配指数和JSW变化对临床结果和假体生存率的影响,未来的研究应关注这一点。总之,良好的内侧UKA术不仅重建了内侧间室关节表面,且影响了外侧间室的生物力学,并通过改善外侧间室的关节匹配度和恢复JSW,延缓了外侧间室关节退变的进展,从而降低内侧UKA术后的假体翻修率。需要注意的是,UKA术中应严格控制力线,防止胫股关节半脱位,以减少可能发生的术后并发症。 "
| [1] HADA S, ISHIJIMA M, KANEKO H, et al. Association of medial meniscal extrusion with medial tibial osteophyte distance detected by T2 mapping MRI in patients with early-stage knee osteoarthritis. ArthritiRes Ther. 2017;19(1):201-212. [2] SEKIYA, I, SASAKI, S, MIURA, Y, et al. Medial ibial osteophyte width strongly reflects medial meniscus extrusion distance and medial joint space width moderately reflects cartilage thickness in knee radiographs.J Magn Reson Imaging. 2022;56(3):824-834. [3] BLOECKER K, WIRTH W, HUNTER DJ, et al. Contribution of regional 3D meniscus and cartilage morphometry by MRI to joint space width in fixed flexion knee radiography-a between-knee comparison in subjects with unilateral joint space narrowing. Eur J Radiol. 2013; 82(12):e832-e839. [4] HUNTER DJ, ZHANG YQ, TU X, et al. Change in joint space width: hyaline articular cartilage loss or alteration in meniscus. Arthritis Rheum. 2006; 54(8):2488-2495. [5] PARSONS CM, JUDGE A, MEYER R, et al.Determining individual trajectories of joint space loss: improved statistical methods for monitoring knee osteoarthritis disease progression. Osteoarthritis Cartilage. 2021;29(1): 59-67. [6] HUNTER DJ, BUCK R, VIGNON E, et al. Relation of regional articular cartilage morphometry and meniscal position by MRI to joint space width in knee radiographs. Osteoarthritis Cartilage. 2009;17(9):1170-1176. [7] ADAMS JG, MCALINDON T, DIMASI M, et al. ontribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol. 1999;54(8):502-506. [8] BEATTIE KA, DURYEA J, PUI M, et al. Minimum joint space width and tibial cartilage morphology in the knees of healthy individuals: a cross-sectional study. BMC Musculoskelet Disord. 2008;9:119. [9] ROTH M, EMMANUEL K, WIRTH W, et al.Sensitivity to change and association of three-dimensional meniscal measures with radiographic joint space width loss in rapidclinical progression of knee osteoarthritis.Eur Radial. 2018;28(5):1844-1853. [10] ELLIS RT, NETTROUR JF, KEENEY JA. TKA is More Durable Than UKA for Morbidly Obese Patients: A Two-Year Minimum Follow-Up Study. Arthroplasty. 2021;36(6):1933-1941. [11] O’NEILL CN, GOWD AK, WATERMAN BR, et al. Significant Reduction in Short-Term Complications Following Unicompartmental Versus Total Knee Arthroplasty: A Propensity Score Matched Analysis. Arthroplasty. 2022;37(10):2014-2019. [12] KLASAN A, TAY ML, FRAMPTON C, et al. High usage of medial unicompartmental knee arthroplasty negatively influences total knee arthroplasty revision rate.Knee Surg Sports Traumatol Arthrosc. 2022; 30(9):3199-3207. [13] PONGCHAROEN B, LIENGWATTANAKOL P, BOONTANAPIBUL K. Comparison of Functional Recovery Between Unicompartmental and Total Knee Arthroplasty: A Randomized Controlled Trial. J Bone Joint Surg. 2023;105(3):191-201. [14] DI MARTINO A, BORDINI B, BARILE F, et al. Unicompartmental knee arthroplasty has higher revisions than total knee arthroplasty at long term follow-up: a registry study on 6453 prostheses. Knee Surg Sports Traumatol Arthrosc. 2021;29(10):3323-3329. [15] LEE CS, SU EP, CROSS MB, et al. Unicompartmental Knee Arthroplasty Is Associated With a Lower Rate of Periprosthetic Joint Infection Compared to Total Knee Arthroplasty. Arthroplast Today. 2021;10:117-122. [16] FISHER N, AGARWAL M, REUBEN SF, et al. Sporting and physical activity following Oxford medial unicompartmental knee arthroplasty. Knee. 2006;13(4):296-300. [17] GOODFELLOW J, O’CONNOR J, DODD C, et al. Unicompartmental arthroplasty with the Oxford knee. New York: Oxford University Press, 2006: 44-45,169. [18] NIINIMÄKI TT, MURRAY DW, PARTANEN J, et al.Unicompartmental knee arthroplasties implanted for osteoarthritis with partial loss of joint space have high re-operation rates. Knee. 2011;18(6):432-435. [19] PANDIT H, GULATI A, JENKINS C, et al. Unicompartmental knee replacement for patientswith partial thickness cartilage loss in the affected compartment. Knee. 2011;18(3):168-171. [20] MAIER MW, KUHS F, STREIT MR, et al. Unicompartmental knee arthroplasty in patients with full versus partial thickness cartilage loss (PTCL): equal in clinical outcome butwithhigher reoperation rate for patients with PTCL. Arch Orthop Trauma Surg. 2015;135(8):1169-1175. [21] KNIFSUND J, HATAKKA J, KEEMU H, et al. Unicompartmental knee arthroplasties are performed on the patients with radiologically too mild osteoarthritis.ScandJ Surg. 2017;106(4):338-341. [22] HAMILTON TW, PANDIT HG, INABATHULA A, et al. Unsatisfactory outcomes following unicompartmental knee arthroplasty in patients with partial thickness cartilage loss: a medium-term follow-up. Bone Joint J. 2017;99-B(4):475-482. [23] WURM A, ZECHLING A, LEITNER H, et al. Medial unicondylar knee arthroplasty should be reserved for patients with complete joint space collapse. Knee Surg Sports Traumatol Arthrosc. 2022; 30(9):3162-3167. [24] CARLSON SW, VARGAS-HERNANDEZ JS, CARLSON BC, et al. Lack of bone-on-bone arthritis is not a strict contraindication for mobile-bearing unicompartmental knee arthroplasty. JBJS Open Access. 2020; 5(3):e19.00058-e19.00058. [25] WONG KC, LEE M, LIOW L, et al. Bone-on-bone contact on radiograph is not a prerequisite for successful outcome in fixed-bearing medial unicompartmental kneearthroplasty-A 10-year follow-up study. J Knee Surg. 2023;36(6):658-666. [26] NIINIMAKI T, ESKELINEN A, MAKELA K, et al. Unicompartmental knee arthroplasty survivorship is lower than TKA survivor-ship:A 27-year finnish registry study. Clin Orthop Relat Res. 2014;472(5):1496-1501. [27] 李世超,解光越,孙振,等.应力位X射线片与单髁置换后膝关节对位对线的关系[J].中国组织工程研究,2023,27(18):2910-2914. [28] VASSO M, DEL REGNO C, D’AMELIO A, et al.Minor varus alignment provides better results than neutral alignment in medial UKA. Knee. 2015;22(2):117-121. [29] YUE J, GUO W, WAN F, et al. Quantitative Evaluation of joint space width in the lateral compartment after medial unicompartmental knee arthroplasty: comparison of three radiographic views. J Knee Surg. 2018; 31(8):730-735. [30] KHAMAISY S, ZUIDERBAAN HA, VAN DER LIST JP, et al. Medial unicompartmental knee arthroplasty improves congruence and restores joint space width of the lateral compartment.Knee. 2016;23(3):501-505. [31] 俞颖豪,赵继军,刘冬铖,等. 数字图像术前规划辅助单髁置换对固定平台假体摆位的临床指导意义[J]. 中国组织工程研究,2021,25(21): 3324-3331. [32] KELLGREN JH, LAWRENCE JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16(4):494-502. [33] FDA/CDER resource page. Food and Drug Administration Web site. Guidance for industry: clinical development programs for drugs, devices, and biological products intended for the treatment of osteoarthritis. Available at: http://www.fda.gov/cder/guidance/2199dft.htm. Accessed November 28, 2002. [34] The European Agency for the Evaluation of Medicinal Products Human Medicines Committee for proprietary medicinal products (CTMP) points to consider on the clinical investigation of medicinal products used in the treatment of osteoarthritis. Available at:http://www.eudra.org. Accessed November 28, 2002. [35] BUCKLAND-WRIGHT JC, MACFARLANE DG, WILLIAMS SA, et al. Accuracy and precision of joint space width measurements in standard and macroradiographs of osteoarthritic knees. Ann Rheum Dis. 1995;54(11): 872-880. [36] JANSEN MP, MASTBERGEN SC, ECKSTEIN F, et al. Comparison between 2D radiographic weight-bearing joint space width and 3D MRI non-weight-bearing cartilage thickness measures in the knee using non-weight-bearing 2D and 3D CT as an intermediary. Ther Adv Chronic Dis. 2021;12:20406223211037868. [37] PIPERNO M, HELLIO LE GRAVERAND MP, CONROZIER T, et al. Quantitative evaluation of joint space width in femorotibial osteoarthritis: comparison of three radiographic views. Osteoarthritis Cartilage. 1998;6(4):252-259. [38] VIGNON E, PIPERNO M, LE GRAVERAND MP, et al. Measurement of radiographic joint space width in the tibiofemoral compartment of the osteoarthritic knee: comparison of standing anteroposterior and Lyon schuss views. Arthritis Rheum. 2003;48(2):378-384. [39] CHEUNG JC, TAM AY, CHAN LC, et al. Superiority of multiple-joint space width over minimum-joint space width approach in the machine learning for radiographic severity and knee osteoarthritis progression. Biology (Basel). 2021;10(11):1107. [40] PAIXAO T, DIFRANCO MD, LJUHAR R, et al. A novel quantitative metric for joint space width: data from the Osteoarthritis Initiative (OAI). Osteoarthritis Cartilage. 2020;28(8):1055-1061. [41] YANAGISAWA S, OHSAWA T, SAITO K, et al. Morphological evaluation and diagnosis of medial type osteoarthritis of the knee using ultrasound. J Orthop Sci. 2014;19(2):270-274. [42] ZHU J, LI B, QIU L, et al. A measurement method of knee joint space width by ultrasound: a large multicenter study. Quant Imag Med Sug. 2020;10(5):979-987. [43] ECKSTEIN F, GUERMAZI A, GOLD G, et al. Imaging of cartilage and bone: promises and pitfalls in clinical trials of osteoarthritis. Osteoarthritis Cartilage. 2014;22(10):1516-1532. [44] PELLETIER JP, COOPER C, PETERFY C, et al. What is the predictive value of MRI for the occurrence of knee replacement surgery in knee osteoarthritis? Ann Rheum Dis. 2013;72(10):1594-1604. [45] CICUTTINI FM, JONES G, FORBES A, et al. Rate of cartilage loss at two years predicts subsequent total knee arthroplasty: a prospective study. Ann Rheum Dis. 2004;63(9):1124-1127. [46] RAYNAULD JP, MARTEL-PELLETIER J, HARAOUI B, et al. Risk factors predictive of joint replacement in a 2-year multicentre clinical trial in knee osteoarthritis using MRI: results from over 6 years of observation.Ann Rheum Dis. 2011;70(8):1382-1388. [47] ECKSTEIN F, BOUDREAU R, WANG Z, et al. Comparison of radiographic joint space width and magnetic resonance-imaging for prediction of knee replacement-A longitudinal case-control study from the osteoarthritis initiative. Eur Radiol. 2016;26(6): 1942-1951. [48] LE GRAVERAND MP, BUCK RJ, WYMAN BT, et al. Change in regional cartilage morphology and joint space width in osteoarthritis participants versus healthy controls: a multicentre study using 3.0 Tesla MRI and Lyon-Schuss radiography. Ann Rheum Dis. 2010;69(1):155-162. [49] KOTHARI MD, RABE KG, ANDERSON DD, et al. The relationship of three-dimensional joint space width on weight bearing CT with pain and physical function. J Orthopaed Res. 2019:10.1002/jor.24566. [50] TURMEZEI TD, BLOW S, RUPRET S, et al. Quantitative three-dimensional assessment of knee joint space width from weight-bearing CT. Radiology. 2021;299(3):649-659. [51] TURMEZEI TD, LOW SB, RUPRET S, et al. Multiparametric 3-D analysis of bone and joint space width at the knee from weight bearing computed tomography. Osteoarthr Imaging. 2022;2(2):100069. |
| [1] | Shan Jiaxin, Zhang Yilong, Wu Hongtao, Zhang Jiayuan, Li Anan, Liu Wengang, Xu Xuemeng, Zhao Chuanxi. Changes in muscle strength and pain in patients receiving Jianpi Yiqi Huoxue Formula after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1378-1382. |
| [2] | Shen Jiangyong, He Xi, Tang Yuting, Wang Jianjun, Liu Jinyi, Chen Yuanyuan, Wang Xinyi, Liu Tong, Sun Haoyuan. RAS-selective lethal small molecule 3 inhibits the fibrosis of pathological scar fibroblasts [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1168-1173. |
| [3] | Tan Nengxian, Wu Wenzheng, Zheng Churong, Luo Lieliang, Gu Peng, Ouyang Chongzhi, Zheng Xiaohui. Finite element analysis of different fixation methods of partially threaded cannulated screws for treating vertical femoral neck fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 873-878. |
| [4] | Zheng Jiafa, Song Xiufeng, Li Hongzhi, Zhou Jinming, Guan Shengyi, Yu He. Open reduction and internal fixation via the para-Achilles tendon approach for the treatment of posterior malleolus sandwich fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(6): 934-938. |
| [5] | Zhou Xiaowen, Fu Zuchang, Huang Fei, Ai Jianguo, Zhao Feng. Bone defect blocked by bone cement segmental filling in single-plane tibial bone transport [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 736-740. |
| [6] | Ge Jin, Huang Dong, Yan Jinlian, Xu Zhengquan, Wang Yehua. Relationship between low back pain and spinal-pelvic sagittal parameter changes in patients with hip-spine syndrome after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(36): 5823-5827. |
| [7] | Zhao Yan, Wu Fan, Li Hong, Wan Shengyu, He Jin, Zhu Binren, Jiang Congbing. Prolonging use of tranexamic acid is helpful to reduce perioperative hidden blood loss in senile patients with intertrochanteric fractures [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(36): 5858-5864. |
| [8] | Zhang Xiurong, Cui Xinmei, Zhao Haiyan, Dai Jin, Fu Jiaxin, Wang Bo. Effect of Tiaodu Tongmai acupuncture therapy on rheumatoid arthritis at different ages by generalized estimating equation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(35): 5584-5590. |
| [9] | Lan Yao, Chen Liuyang, Song Wenhui. Key biomarkers for the diagnosis of intervertebral disc degeneration associated with oxidative stress: identification based on bioinformatics and machine learning [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(35): 5591-5597. |
| [10] | Yuan Ping, Wang Zhihua, Wang Weizhou, Wang Wentong, He Fei. Exosome-derived microRNA with bone and joint diseases: role and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(31): 5063-5069. |
| [11] | Wu Tian, Zhao Yue, Hu Rong. Effect of nanobubbles carrying double antibodies on the proliferation of ovarian cancer cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 341-346. |
| [12] | Gao Xueyu, Zhang Wentao, Sun Tianze, Zhang Jing, Li Zhonghai. Application of metal ions in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 439-444. |
| [13] | Zhao Guangjian, Liu Danan, Zhou Bo, Wang Yao. Action mechanism by which fibronectin type III domain-containing protein 5 inhibits macrophage pyroptosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(25): 4005-4012. |
| [14] | Dong Hanqing, Wu Xing, Xu Pengcheng, Wang Qingwen, Zhang Zhisheng, Zhao Jianyong. 3D printing precise positioning guided ulnar groove plasty for treatment of cubital tunnel syndrome [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(18): 2825-2829. |
| [15] | Yuan Tianyi, Liu Hongjiang, Yang Zengqiang, Lu Xingbao, Maimaitiyibubaji, Zhou Zhiheng, Cui Yong. Identification of differences in N6-methyladenosine-related genes in steroid-induced femoral head necrosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(14): 2159-2165. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||